“Father of Plastic Surgery.”
“Father of Plastic Surgery.”
PLASTIC AND
COSMETIC SURGERY
BY
FREDERICK STRANGE KOLLE, M.D.
FELLOW OF NEW YORK ACADEMY OF MEDICINE; MEMBER OF DEUTSCHE MEDEZINISCHE
GESELLSCHAFT, N. Y., KINGS COUNTY HOSPITAL ALUMNI SOCIETY,
AUTHORS’ COMMITTEE AMERICAN HEALTH LEAGUE, PHYSICIANS’
LEGISLATURE LEAGUE ETC.; AUTHOR OF “THE X-RAYS:
THEIR PRODUCTION AND APPLICATION,” “MEDICO-SURGICAL
RADIOGRAPHY,” “SUBCUTANEOUS
HYDROCARBON PROTHESES,” ETC.
WITH ONE COLORED PLATE AND FIVE HUNDRED AND
TWENTY-TWO ILLUSTRATIONS IN TEXT

NEW YORK AND LONDON
D. APPLETON AND COMPANY
1911
Copyright, 1911, by
D. APPLETON AND COMPANY
PRINTED AT THE APPLETON PRESS,
NEW YORK, U. S. A.
TO
ALPHONZO BENJAMIN BOWERS
WHO KINDLED THE FIRE OF MY AMBITION
AND KEPT IT BURNING BY
HIS INTEREST AND UNTIRING APPRECIATION
THIS WORK IS
WITH HEARTFELT GRATITUDE
INSCRIBED
The object of the author has been to place before the profession a thoroughly practical and concise treatise on plastic and cosmetic surgery. The importance of this branch of practice is at the present time undeniable, yet the literature on this subject is widely scattered and scanty. It consists mostly of small, detached papers or reports in different countries, with an occasional reference in text-books on general surgery.
The author feels, from the numerous inquiries made him by physicians from many parts of the world concerning methods herein described, that there is now an actual need for an authoritative work on this subject.
Great care has been taken to select the best matter and to present it with comprehensive illustrations every physician can readily and confidently refer to.
Skin-grafting has been particularly gone into, as well as electrolysis as applied to dermatology, with information as to the construction and scientific use of apparatus involved.
To the whole has been added the practical experience and criticism of the author, who has devoted many years to the scientific and faithful advancement of this specialty.
Frederick Strange Kolle.
12 East Thirty-first Street,
New York City.
| PAGE | |
| CHAPTER I HISTORICAL |
|
| Historical | 1 |
| CHAPTER II REQUIREMENTS FOR OPERATING |
|
| The operating room: The walls; The floors; Skylight; Disinfection; Instrument cabinet; Operating table; Instrument table; Irrigator—Care of instruments—Preparation of the surgeon and assistants: Care of the hands; Gowns—Preparing the patient: General preparation; Preparation of the operative field | 9 |
| CHAPTER III REQUIREMENTS DURING OPERATION |
|
| Sponges and sponging—Sterilization of dressings: Wallace sterilizer; Sprague sterilizer; Sterilizing plant; Dressing cases; Waste cans—Sutures and sterilization: Silkworm gut and silk; Catgut | 22 |
| CHAPTER IV PREFERRED ANTISEPTICS |
|
| Antiseptic solutions—Antiseptic powders | 34 |
| CHAPTER V WOUND DRESSINGS |
|
| Sutured wounds—Sutureless coaptation—Granulation—Changing dressings—Wounds of the mucous membrane—Pedunculated flaps—Foreign bodies | 43 |
| CHAPTER VI SECONDARY ANTISEPSIS |
|
| Septicemia following wound infection—Gangrene—Erysipelatous infection | 52[x] |
| CHAPTER VII ANESTHETICS |
|
| General anesthesia: Preparation for general anesthesia; Chloroform; Ether; Combined anesthesia; Nitrous oxid; Ethyl bromid; Ethyl chlorid—Local anesthesia: Ethyl chlorid; Cocain; Beta eucain; Liquid air; Stovain | 58 |
| CHAPTER VIII PRINCIPLES OF PLASTIC SURGERY |
|
| Incisions—Sutures—Needles—Needle holders—Methods in plastic operations: Stretching method; Sliding method; Twisting method; Implantation of pedunculated flaps by bridging; Transplantation of nonpedunculated flaps or skin-grafting; Autodermic skin-grafting; Heterodermic skin-grafting; Zoödermic skin-grafting—Mucous-membrane-grafting—Bone-grafting—Hair-transplantation | 76 |
| CHAPTER IX BLEPHAROPLASTY |
|
| Ectropion: Partial ectropion; Complete ectropion; Ectropion of both lids—Epicanthus—Canthoplasty—Ptosis—Ankyloblepharon—Wrinkled eyelids—Xanthelasma palpebrarum | 103 |
| CHAPTER X OTOPLASTY |
|
| Restoration of the auricle—Auricular protheses—Coloboma—Malformation of the lobule: Enlargement of the lobule; Attachment of the lobe—Malformation of the auricle: Microtia—Auricular Appendages—Polyotia—Malposition of the auricle | 120 |
| CHAPTER XI CHEILOPLASTY |
|
| Harelip: Classification of harelip deformities; The operative correction of harelip; Of unilateral labial cleft; Of congenital bilateral labial cleft; Post-operative treatment of harelip—Superior cheiloplasty: Classification of deformities of the upper lip; Operative correction of deformities of the upper lip—Inferior cheiloplasty—Labial deficiency—Labial ectropion—Labial entropion—Vermilion deficiency | 145 |
| CHAPTER XII STOMATOPLASTY |
|
| The correction of macrostoma—The correction of microstoma | 192[xi] |
| CHAPTER XIII MELOPLASTY |
|
| Small and medium defects—Large defects—Employment of protheses | 198 |
| CHAPTER XIV SUBCUTANEOUS HYDROCARBON PROTHESES |
|
| Indications—Precautions—The advantage of the method—Untoward results: Intoxication; Reaction; Infection; Necrosis; Sloughing; Sloughing due to pressure; Subinjection; Hyperinjection; Air embolism; Paraffin embolism; Primary diffusion or extension of paraffin; Interference with muscular action of the wings of the nose; Escape of paraffin after withdrawal of needle; Solidification of paraffin in needle; Absorption or disintegration of the paraffin; The difficulty of procuring paraffin with proper melting point; Hypersensitiveness of skin; Redness of the skin; Secondary diffusion of the injected mass; Hyperplasia of the connective tissue following the organization of injected matter; Yellow appearance and thickening of the skin after organization of the injected mass has taken place; The breaking down of tissue and resultant abscess due to the pressure of the injected mass upon the adjacent tissue after the injection has become organized—The proper instruments for the subcutaneous injection of hydrocarbon protheses—Preparation of the site of operation—Preparation of the instruments for operation—The practical technique—Specific classification for the employment and indication of hydrocarbon protheses about the face—Specific classification for the employment and indication of hydrocarbon protheses about the shoulders, etc.—Specific technique for the correction of regional deformities about the face: Transverse depressions; Deficient or receding forehead; Unilateral deficiency; Interciliary furrow; Temporal muscular deficiency; Deformities of the nose; Deformities about the mouth; Deformities about the cheeks; Deformities about the orbit; Deformities about the chin; Deformities about the ear—Specific technique for the correction of deformities about the shoulders | 209 |
| CHAPTER XV RHINOPLASTY |
|
| The causes of nasal destruction—Classification of deformities—Surgical technique—Protheses—Nasal replanting—Nasal transplanting—Total rhinoplasty: Pedunculated flap method; The Indian or Hindu method; The French method; The Italian method; The combined flap method; Organic support of nasal flaps; Periostitic supports; Osteoperiostitic supports; Cartilaginous support of flap—Partial rhinoplasty; Restoration of base of nose; Restoration of lobule and alæ; Restoration of the alæ; Restoration of nasal lobule; Restoration of subseptum | 339[xii] |
| CHAPTER XVI COSMETIC RHINOPLASTY |
|
| Angular nasal deformity—Correction of elevated lobule—Correction of bulbous lobule—Angular excision to correct lobule—Correction of malformations about nasal lobule—Deficiency of nasal lobule—Correction of widened base of nose—Reduction of thickness of alæ—Correction of nasal deviation—Undue prominence of nasal process of the superior maxillary | 448 |
| CHAPTER XVII ELECTROLYSIS IN DERMATOLOGY |
|
| The electric battery—The voltage or electromotive force—Cell selector—Milliampèremeter—The electric current—Portable batteries—Electrodes—Removal of superfluous hair—Removal of moles or other facial growths—Telangiectasis—Removal of nævi—Removal of tattoo marks—The treatment of scars | 470 |
| CHAPTER XVIII CASE RECORDING METHODS |
|
| Photographs—Stencil record—The rubber stamp—The plaster cast—Preparation of photographs | 491 |
Transcriber’s Note: Some illustrations have been moved to where they fit best with the surrounding text. Links lead to the illustration, not to the page number.
| FIG. | PAGE |
| A. Cornelius Celsus (“Father of Plastic Surgery”). | Frontispiece |
| Historical | |
| 1.—Celsus incision for restoration of defect | 2 |
| 2.—Celsus incision to relieve tension | 2 |
| Requirements for Operating | |
| 3.—Formaldehyd disinfecting apparatus | 11 |
| 4.—Instrument cabinet | 12 |
| 5.—Operating table | 13 |
| 6.—Instrument table | 14 |
| 7.—Irrigator | 15 |
| 8.—Instrument sterilizer | 16 |
| 9.—Aseptic washstand | 17 |
| 10.—Von Bergman operating gown | 19 |
| 11.—Triffe rubber apron | 19 |
| Requirements during Operation | |
| 12.—Basins and rack | 23 |
| 13.—Willy Meyer sterilizer | 25 |
| 14.—Wallace sterilizer | 25 |
| 15.—Sprague type of sterilizer | 26 |
| 16.—Sterilizing plant | 28 |
| 17.—Dressing case | 29 |
| 18.—Combination dressing case and table | 29 |
| 19.—Waste pail | 30 |
| 20.—Clark Kumol apparatus | 32 |
| Wound Dressing | |
| 21, 22.—Plaster sutures | 46 |
| 23, 24.—Angular plaster sutures | 46 |
| Secondary Antisepsis | |
| 25.—Walcher dressing forceps | 55 |
| 26.—Toothed seizing forceps | 55[xiv] |
| Anesthetics | |
| 27.—Schimmelbusch dropping bottle | 60 |
| 28.—Esmarch dropping bottle | 60 |
| 29.—Schimmelbusch folding mask | 61 |
| 30.—Esmarch inhaler | 61 |
| 31.—Allis inhaler | 65 |
| 32.—Fowler inhaler | 65 |
| 33.—Juillard mask | 66 |
| 34.—Simplex syringe | 72 |
| 35.—Kolle improved Pravaz syringe | 72 |
| 36.—“Sub-Q” syringe | 72 |
| Principles of Plastic Surgery | |
| 37.—⅝ circle Haagedorn needles | 77 |
| 38.—Crescent curve Haagedorn needles | 77 |
| 39.—Kersten-Mathieu needle holder | 78 |
| 40.—Haagedorn needle holder | 78 |
| 41.—Pozzi-Haagedorn needle holder | 78 |
| 42.—Weber-Haagedorn needle holder | 78 |
| 43.—Needleholder with suture carrier | 78 |
| 44.—Celsus skin incisions | 80 |
| 44 a.—Celsus relieving incisions | 80 |
| 45.—Rhomboid excision | 80 |
| 46.—Union of rhomboid excision | 80 |
| 47.—Oblong excision | 81 |
| 48.—Coaptation of wound | 81 |
| 49.—Bitriangular excision | 81 |
| 50.—Linear coaptation | 81 |
| 51.—Triangular excision | 81 |
| 52.—Coaptation of wound | 81 |
| 53.—Triangular excision with relieving incisions | 82 |
| 54.—Coaptation of wound | 82 |
| 55.—Square excision | 82 |
| 56.—Coaptation of wound | 82 |
| 57.—Square excision | 82 |
| 58.—Coaptation of flaps | 82 |
| 59.—Triangular excision | 83 |
| 60.—Coaptation of flap | 83 |
| 61.—Triangular excision | 83 |
| 62.—Coaptation of flaps | 83 |
| 63.—Triangular excision | 83 |
| 64.—Arrangement of flaps | 83 |
| 65.—Double triangular excision | 84 |
| 66.—Coaptation of wound | 84 |
| 67.—Tri-triangular excision | 84 |
| 68.—Coaptation of wound | 84[xv] |
| 69.—Rectangular-bitriangular excision | 84 |
| 70.—Coaptation of wound | 84 |
| 71.—Weber excision method | 85 |
| 72.—Coaptation of flaps | 85 |
| 73.—Elliptical excision | 85 |
| 74.—Coaptation of flaps | 85 |
| 75.—Triangular excision | 86 |
| 76.—Coaptation of flaps | 86 |
| 77.—Triangular excision | 86 |
| 78.—Coaptation of flaps | 86 |
| 79.—Lentenner method of excision | 86 |
| 80.—Coaptation of flap | 86 |
| 81.—Burns method of excision | 87 |
| 82.—Coaptation of flaps | 87 |
| 83.—Tagliacozza harness | 87 |
| 84.—Smith skin-grafting scissors | 89 |
| 85.—Thiersch skin-grafting razor | 93 |
| 86.—Thiersch folding razor | 93 |
| 87.—Method of cutting Thiersch graft | 94 |
| 88.—Method of placing Thiersch graft | 95 |
| Blepharoplasty | |
| 89.—Correction of ectropion, Dieffenbach method | 104 |
| 90 a and b.—Correction of partial ectropion (author’s case) | 104 |
| 91, 92.—Complete ectropion, Dieffenbach method | 106 |
| 93, 94.—Complete ectropion, Wolfe method | 107 |
| 95, 96.—Complete ectropion, Fricke method | 108 |
| 97, 98.—Complete ectropion, Ammon-Von Langenbeck method | 109 |
| 99, 100.—Complete ectropion, Dieffenbach-Serre method | 110 |
| 101, 102, 103.—Complete ectropion, Tripier method | 111 |
| 104, 105.—Complete ectropion, Von Artha method | 112 |
| 106, 107.—Epicanthus, Bull method | 113 |
| 108.—Probe-pointer angular scissors | 114 |
| 109, 110, 111.—External canthoplasty | 115 |
| 112, 113.—Blepharoplastics, author’s method | 116 |
| 114.—Curved eye scissors | 117 |
| Otoplasty | |
| 115.—Partial restoration of the auricle | 124 |
| 116.—Correction of lobular defect | 126 |
| 117.—Coaptation of wound | 126 |
| 118, 119.—Greene method correcting coloboma | 126 |
| 120.—Noyes’s clamp | 127 |
| 121, 122.—Correction of attached lobe | 128 |
| 123.—Restoration of auricle, Szymanowski method | 129 |
| 124.—Auricular stump for attachment of artificial ear | 130 |
| 125.—Auricular prothesis | 130[xvi] |
| 126.—Auricular prothesis applied to stump | 131 |
| 127.—Anterior view of auricular prothesis | 131 |
| 128.—Posterior view of auricular prothesis | 131 |
| 129, 130, 131.—Schwartze method of correction of macrotia | 134 |
| 132, 133.—Parkhill method of correction of macrotia | 135 |
| 134, 135.—Author’s method of correction of macrotia | 137 |
| 136, 137.—Author’s method of correction of macrotia | 137 |
| 138.—Monks’ method of correction of malposed ear | 139 |
| 139, 140.—Author’s method of correction of malposed ear | 140 |
| 141, 142.—Correction of malposed auricles, author’s case (anterior view) | 142 |
| 143, 144.—Posterior view of replaced auricles | 143 |
| Cheiloplasty | |
| 145.—Burchardt compression forceps | 145 |
| 146.—Beinl harelip clamp | 145 |
| 147.—Median cleft, Siegel’s case | 147 |
| 148.—Median cleft with rhinophyma, Trendelenburg’s case | 147 |
| 149, 150, 151.—Types of unilateral labial cleft | 148 |
| 152.—Unilateral facial cleft, Hasselmann | 149 |
| 153.—Bilateral facial cleft, Guersant | 149 |
| 154.—Buccal fissure with macrostoma | 150 |
| 155, 156, 157.—Harelip correction, Nélaton method | 152 |
| 158, 159.—Harelip correction, Fillebrown method | 153 |
| 160, 161, 162.—Harelip correction, Von Langenbeck-Wolff-Sedillot method | 153 |
| 163, 164, 165.—Harelip correction, Malgaigne method | 154 |
| 166, 167.—Harelip correction, Gräfe method | 154 |
| 168, 169, 170.—Harelip correction, Mirault method | 155 |
| 171, 172, 173.—Harelip correction, Giralde method | 155 |
| 174, 175, 176.—Harelip correction, König method | 156 |
| 177, 178, 179.—Harelip correction, Maas method | 156 |
| 180, 181, 182.—Harelip correction, Haagedorn method | 157 |
| 183, 184, 185.—Harelip correction, Dieffenbach method | 157 |
| 186, 187.—Correction bilateral cleft, Von Esmarch method | 159 |
| 188, 189, 190.—Correction bilateral cleft, Maas method | 159 |
| 191, 192, 193.—Correction bilateral cleft, Haagedorn method | 160 |
| 194, 195, 196.—Correction bilateral cleft, Simon method | 160 |
| 197.—Hainsley cheek compressor | 161 |
| 198, 199.—Superior cheiloplasty, Bruns method | 164 |
| 200, 201.—Superior cheiloplasty, Sedillot method | 165 |
| 202.—Superior cheiloplasty, Buck method | 165 |
| 203, 204, 205.—Superior cheiloplasty, Estlander method | 166 |
| 206, 207.—Inferior cheiloplasty, Richerand method | 169 |
| 208, 209.—Extirpation of vermilion border | 169 |
| 210, 211.—Inferior cheiloplasty, Celsus method with additional incisions | 170 |
| 212, 213.—Inferior cheiloplasty, Estlander method | 171 |
| 214, 215.—Inferior cheiloplasty, Bruns method | 172[xvii] |
| 216, 217.—Inferior cheiloplasty, Buck method | 172 |
| 218, 219.—Inferior cheiloplasty, Dieffenbach method | 173 |
| 220, 221.—Inferior cheiloplasty, Jäsche method | 174 |
| 222, 223.—Inferior cheiloplasty, Trendelenburg method | 174 |
| 224, 225.—Inferior cheiloplasty, Bruns method | 175 |
| 226, 227.—Inferior cheiloplasty, Bruns bilateral method | 175 |
| 228, 229, 230.—Inferior cheiloplasty, Buchanan method | 176 |
| 231, 232.—Inferior cheiloplasty, Syme method | 177 |
| 233, 234.—Inferior cheiloplasty, Blasius method | 178 |
| 235, 236.—Inferior cheiloplasty, Bürow method | 178 |
| 237, 238.—Inferior cheiloplasty, von Langenbeck | 179 |
| 239, 240.—Inferior cheiloplasty, Morgan method | 180 |
| 241, 242.—Inferior cheiloplasty, Zeis method | 181 |
| 243, 244.—Inferior cheiloplasty, Delpech method | 182 |
| 245, 246.—Inferior cheiloplasty, Teale method | 185 |
| 247, 248.—Labial ectropion, author’s method | 187 |
| 249, 250.—Labial ectropion, author’s method | 188 |
| Stomatoplasty | |
| 251, 252.—Correction of Macrostoma, Dieffenbach-Von Langenbeck method | 193 |
| 253, 254.—Correction of Macrostoma, author’s method | 195 |
| 255, 256.—Correction of Microstoma, Dieffenbach method | 196 |
| 257.—Artificial mouth, Heuter | 196 |
| Meloplasty | |
| 258, 259.—Meloplasty, Serre method | 199 |
| 260, 261.—Correction of angle of mouth | 200 |
| 262, 263.—Correction of extensive angle of mouth | 200 |
| 264, 265.—Meloplasty, Kraske method | 201 |
| 266, 267, 268.—Meloplasty, Israel method | 202 |
| 269, 270.—Meloplasty, Bardenheuer | 202 |
| 271, 272, 273, 274.—Meloplasty, Bardenheuer | 203 |
| 275, 276, 277, 278.—Meloplasty, Bardenheuer | 204 |
| 279, 280.—Meloplasty, Staffel | 205 |
| 281.—Cheek prothesis after removal of sarcoma, Martin | 206 |
| 282.—Prothesis applied to face | 207 |
| Subcutaneous Hydrocarbon Protheses | |
| 283.—Circulation of the head (author) | Facing 210 |
| 284.—Eckstein insulated syringe | 232 |
| 285.—Quinlan paraffin heater | 232 |
| 286.—Author’s electrothermic paraffin heater | 244 |
| 287.—Smith paraffin heater | 246 |
| 288 a, 288 b.—Microphotograph, showing fibromatosis | Facing 258 |
| 289.—Author’s drop syringe | 265 |
| 290.—Author’s all-metal syringe | 266[xviii] |
| 291.—Smith’s all-metal syringe | 267 |
| 292, 293.—Anterior superior third nasal deficiency and correction thereof | 289 |
| 294, 295.—Anterior median third nasal deficiency and correction thereof | 292 |
| 296, 297.—Anterior inferior third nasal deficiency and correction thereof | 294 |
| 298 a, 298 b.—Anterior superior and inferior third nasal deficiency and correction thereof | 301 |
| 299, 300.—Anterior total nasal deficiency and corrections thereof | 303 |
| 301.—Untoward effect of paraffin injection about lobule and anterior nasal line | 311 |
| 302, 303.—Profile view, showing correction of antero-lateral deficiency about chin | 330 |
| 304, 305.—Frontal view, showing correction of antero-lateral deficiency about chin; also correction of deficiency of cheeks | 332 |
| Rhinoplasty | |
| 306.—Deficiency of superior and middle third of nose | 342 |
| 307.—Post-ulcerative deformity of superior third of nose | 342 |
| 308.—Loss of right ala, lobule and columna | 342 |
| 309.—Loss of lobule, inferior septum and columna | 342 |
| 310.—Ulcerative loss of right median lateral skin of nose | 343 |
| 311.—Loss of nasal bones, partial dorsum, lobule and septum | 343 |
| 312.—Destruction of nasal bones with dorsum and lobule intact | 343 |
| 313.—Total loss of nose | 343 |
| 314, 315, 316.—Koomas method of rhinoplasty | 353 |
| 317.—Graefe method of rhinoplasty | 353 |
| 318, 319, 320, 321.—Delpech method of rhinoplasty | 354 |
| 322, 323.—Lisfranc method of rhinoplasty | 355 |
| 324.—Labat method of rhinoplasty | 356 |
| 325.—Keegan method of rhinoplasty | 356 |
| 326.—Duberwitsky method of rhinoplasty | 357 |
| 327.—Dieffenbach method of rhinoplasty | 357 |
| 328.—Von Ammon method of rhinoplasty | 358 |
| 329.—Auvert method of rhinoplasty | 358 |
| 330.—Von Langenbeck method of rhinoplasty | 359 |
| 331, 332.—Petrali method of rhinoplasty | 360 |
| 333.—Forque method of rhinoplasty | 361 |
| 334.—D’Alguie method of rhinoplasty | 361 |
| 335.—Landreau method of rhinoplasty | 361 |
| 336.—Von Langenbeck method of rhinoplasty | 361 |
| 337.—Von Langenbeck method of rhinoplasty | 362 |
| 338.—Szymanowski method of rhinoplasty | 362 |
| 339.—Nélaton method of rhinoplasty | 365 |
| 340.—Heuter method of rhinoplasty | 365 |
| 341.—Bürow method of rhinoplasty | 365 |
| 342.—Szymanowski method of rhinoplasty | 366 |
| 343, 344.—Serre method of rhinoplasty | 367 |
| 345, 346.—Maisonneuve method of rhinoplasty | 369[xix] |
| 347, 348, 349.—Dieffenbach arm-flap method | 373 |
| 350.—Szymanowski arm-flap method | 375 |
| 351.—Fabrizi arm-flap method | 376 |
| 352, 353.—Steinthal thoracic flap method | 377 |
| 354, 355.—Volkman method of rhinoplasty | 379 |
| 356.—Keegan method of rhinoplasty | 380 |
| 357, 358.—Verneuil method of rhinoplasty | 380 |
| 359, 360.—Thiersch method of rhinoplasty | 381 |
| 361, 362.—Helferich method of rhinoplasty | 382 |
| 363, 364.—Sedillot method of rhinoplasty | 383 |
| 365.—Berger arm-flap method | 385 |
| 366.—Berger retention apparatus | 385 |
| 367, 368.—Szymanowski rhinoplasty method | 386 |
| 369.—König rhinoplasty method | 391 |
| 370.—Von Hacker rhinoplasty method, arrangement of frontal flap to allow chiseling | 392 |
| 371.—Von Hacker rhinoplasty method, making osteo-periostic support | 392 |
| 372.—Von Hacker rhinoplasty method, bone-lined flap in position | 392 |
| 373, 374.—Rotter rhinoplastic method | 394 |
| 375, 376.—Schimmelbusch frontal flap method | 395 |
| 377, 378.—Helferich rhinoplasty method | 397 |
| 379, 380, 381.—Krause rhinoplasty method | 399 |
| 382.—Nélaton rhinoplasty method | 400 |
| 383.—Nélaton rhinoplasty method, making bony support | 400 |
| 384.—Nélaton rhinoplasty method, cutting through bony plate | 401 |
| 385.—Nélaton rhinoplasty method, disposition of frontal flap | 401 |
| 386.—Israel method, forearm flap | 402 |
| 387.—Israel method, position of forearm to place flap | 403 |
| 388.—Nélaton method, outlining frontal flap | 407 |
| 389.—Nélaton method, locating cartilage strip | 408 |
| 390.—Nélaton method, excision of cartilage strip | 409 |
| 391.—Nélaton method, placing of cartilage strip | 410 |
| 392.—Nélaton method, bringing down frontal flap | 411 |
| 393.—Nélaton method, placing frontal flap | 411 |
| 394, 395.—Steinhausen partial rhinoplasty method | 412 |
| 396, 397.—Neumann partial rhinoplasty method | 413 |
| 398, 399, 400.—Later Neumann partial rhinoplasty method | 415 |
| 401.—Bardenheuer method, shape of flap | 416 |
| 402.—Bardenheuer method, disposition of flap | 416 |
| 403.—Ollier method first step | 417 |
| 404.—Ollier method, second step | 418 |
| 405.—Ollier method, position nasal bone occupies | 418 |
| 406.—Von Langenbeck method, first step | 419 |
| 407.—Von Langenbeck method, showing separation and elevation of nose flaps | 419 |
| 408.—Nélaton method, first step | 421 |
| 409.—Nélaton method, making lower nasal flap | 421 |
| 410.—Nélaton method, forming base of nose | 422[xx] |
| 411.—Nélaton method, ultimate disposition of flap | 422 |
| 412.—Bayer-Payr restoration of lobule, first step | 425 |
| 413.—Bayer-Payr restoration of lobule, disposition of flaps | 425 |
| 414.—Bayer-Payr restoration of lobule, placing of pedicles after division | 425 |
| 415.—Ch. Nélaton method, attachment of forearm flap | 426 |
| 416.—Ch. Nélaton method, forearm flap in position, lateral flaps | 426 |
| 417.—Ch. Nélaton method, disposition lateral flaps | 426 |
| 418.—Denonvillier method, making of flap for ala | 428 |
| 419.—Denonvillier method, disposition of flap for anterior pedicle ala | 428 |
| 420.—Denonvillier method, making of flap for ala, posterior pedicle | 428 |
| 421.—Denonvillier method, disposition of flap for ala, posterior pedicle | 428 |
| 422, 423.—Mutter method of restoration of ala | 429 |
| 424, 425.—Von Langenbeck method of restoration of ala | 430 |
| 426.—Busch method of restoration of ala | 430 |
| 427.—Dieffenbach method of restoration of ala | 431 |
| 428.—Dupuytren method of restoration of ala | 431 |
| 429.—Fritz-Reich method of restoration of ala | 431 |
| 430, 431, 432, 433.—Sedillot method of restoration of ala | 432 |
| 434, 435.—Nélaton method of restoration of ala | 433 |
| 436, 437.—Bonnet method of restoration of ala | 434 |
| 438, 439.—Weber method of restoration of ala | 434 |
| 440.—Thompson mucosa flap | 435 |
| 441, 442.—Thompson method of restoration of ala | 435 |
| 443, 444.—Blandin method of restoration of ala | 436 |
| 445, 446.—Von Hacker method of restoration of ala | 436 |
| 447, 448.—Kolle method of restoration of ala | 437 |
| 449.—Denonvillier method of restoration of ala | 438 |
| 450, 451, 452.—Von Hacker method of restoration of ala | 439 |
| 453.—König method of restoration of ala | 440 |
| 454, 455.—Kolle method of restoration of ala | 441 |
| 456, 457.—Kolle method of restoration of lobule | 442 |
| 458, 459.—Blandin method of restoration of subseptum | 444 |
| 460, 461.—Dupuytren method of restoration of subseptum | 445 |
| 462.—Serre method of restoration of subseptum | 445 |
| 463, 464.—Dieffenbach method of restoration of subseptum | 446 |
| 465.—Heuter method of restoration of subseptum | 446 |
| 466.—Szymanowski method of restoration of subseptum | 446 |
| 467, 468.—Szymanowski method of restoration of subseptum | 447 |
| Cosmetic Rhinoplasty | |
| 469 a, 469 b.—Monk method of correction of angular nose | 450 |
| 470, 471, 472.—Median nasal incision for angular nose | 451 |
| 473, 474.—Kolle method of lateral incision for angular nose | 452 |
| 475, 476.—Kolle chisel set | 453 |
| 477.—Kolle metal mallet | 453 |
| 478, 479.—Kolle method of correction of retroussé nose | 454 |
| 480, 481.—Kolle method of correction of broad lobule | 456[xxi] |
| 482, 483.—Kolle method of correction of elongated lobule | 458 |
| 484.—Kolle method of correction of elongated lobule and base of nose after excision | 460 |
| 485.—Kolle method of correction of elongated lobule base of alæ and lobule | 460 |
| 486, 487.—Kolle plaster cast of lobule operation | 461 |
| 488, 489.—Kolle plaster cast of lobule operation | 462 |
| 490, 491.—Kolle plaster cast of lobule operation | 463 |
| 492, 493.—Kolle plaster cast of lobule operation | 464 |
| 494, 495.—Gensoul method of correcting broad nasal base | 465 |
| 496, 497.—Kolle method of correction of broad nasal base | 465 |
| 498, 499.—Linhardt method of reduction of thickened alæ | 466 |
| 500, 501.—Dieffenbach method of reduction of thickened nose | 467 |
| Electrolysis in Dermatology | |
| 502.—Electric wet cell | 470 |
| 503.—Series connection of cells | 472 |
| 504.—Shunt rheostat connection | 473 |
| 505.—Cell selector | 474 |
| 506.—Cell selector and battery connection | 474 |
| 507.—Milliampèremeter | 475 |
| 508.—Direct current wall plate | 475 |
| 509.—Wall-plate connections | 475 |
| 510 a.—Portable wet cell apparatus | 476 |
| 510 b.—Portable dry cell apparatus | 477 |
| 511.—Sponge electrode | 478 |
| 512.—Arm electrode | 478 |
| 513, 514.—Electrolytic needle holders | 479 |
| 515.—Interrupting current needle holder | 479 |
| 516.—Needle holder with magnifying glass | 479 |
| 517.—Epilating forceps | 481 |
| 518.—Electrolysis method for destroying growths | 483 |
| 519.—Multiple needle electrode | 484 |
| 520.—Kolle electric apparatus for tattooing scars | 487 |
| Case Recording Methods | |
| 521.—Nose stencil | 492 |
| 522.—Method of making nose plaster cast | 494 |
It seems almost incredible that at this late day so little is generally known to the surgical profession of the beautiful and practical, not to say grateful, art of plastic or restorative surgery, successfully practiced even by the ancients.
The progress of the art has been much interrupted. It is only the later methods of antisepsis, which have so greatly added to general surgery, that have placed it firmly upon the basis of a distinct and separate art in surgical science.
To Aulus Cornelius Celsus, a Latin physician and philosopher, supposed to have lived in the time of Augustus, we owe the first authentic principles of the science. He was a most prolific writer and an urgent worker. After having introduced the Hippocratic system to the Romans he became known as the Roman Hippocrates. His best-known work handed down to us is the “De Medicina,” the first edition of which, divided into eight books, appeared in Florence in 1478. The seventh and eighth volumes, designated the “Surgical Bible,” contain much valuable data in reference to opinions and observations of the Alexandrian School of Medicine.
In considering plastic operations about the face (Curta in auribus, labrisque ac naribus) he writes, “Ratio curationis ejus modi est; id quod curtatum est, in quadratum redigere; ab interoribus ejus angulis lineas transversas incidere, quæ citeriorem partem ab ulteriore[2] ex toto diducant; deinda ea quæ resolvimus, in unum adducere. Si non satis junguntur, ultra lineas, quas ante fecimus, alias dua lunatas et ad plagam conversas immittere, quibus summa tantum cutis diducatur, sic enim fit, ut facilius quod adducitur, segui possit, quod non vi cogendum est, sed ita adducendum ut ex facili subsequatur; et dimissum non multum recedat.”
Centuries elapsed before a clear understanding of the above was deduced. Several analyses have been advanced, those of O. Weber and Malgaigne being the most generally accepted.
As shown in Fig. 1 the method advanced is one for the restoration or repair of an irregular defect about the face in which two transverse incisions forming angular skin flaps, dissected from the underlying tissue, are advanced, joining the denuded free ends.
Should there be a lack of tissue to accomplish perfect coaptation a semilunar incision beyond either outer border is added, as shown in Fig. 2, which permits of greater traction, leaving two small quatrespheral areas to heal over by granulation:
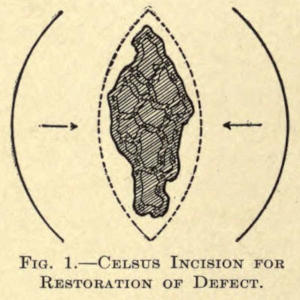
Fig. 1.—Celsus Incision for Restoration of Defect.
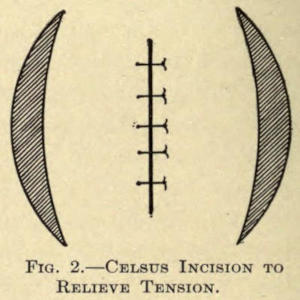
Fig. 2.—Celsus Incision to Relieve Tension.
This is the oldest known reference to plastic surgery of times remote.
From the Orient, however, Susrata in his Ayur-Veda, the exact period of which is unknown, discloses the use of rhinoplastic methods.
For centuries following, and throughout the middle ages, the art seems to have waned and remained practically unknown, as far as is shown in the literature of that period.
A revivalist first appeared about the middle of the fifteenth century in the person of Branca, of Catania, a Sicilian surgeon, who about 1442 established a reputation of building up noses from the skin of the face (exore). His son Antonius enlarged upon his methods and is said to have utilized the integument of the arm to accomplish the same result, thus overcoming the extensive scarring of the face following the elder’s mode. He seems to have been the first authority employing the so-called Italian rhinoplastic method. He is also known to have ventured, more or less, successfully in operations about the lips and ears.
Balthazar Pavoni and Mongitore repeated these methods of operative procedure with more or less success and the brothers Bojanis acquired great celebrity at Naples in the art of remodeling noses.
Vincent Vianeo followed the work of the above.
But, somehow, the heroic efforts of these men dropped so much into oblivion that Fabricius ab Aquapende, in writing of the rhinoplastic work of the brothers Bojani, of Calabria, says: “Primi qui modum reparandi nasum coluere, fuerunt calabri; deinde devenit ad medicos Bononienses.”
That Germany was interested at an early date is shown in the admirable work of a chevalier of the Teutonic Order, Brother Heinrich Von Pfohlspundt, who wrote a book on the subject entitled “Buch der Brundth Ertznei,” with a subtitle, “Eynem eine nawe nasse zu mache.” His volume appeared in 1460, about the time of Antonio Branca, of whose methods he was ignorant, claiming to have learned the art from an Italian who succored many by his skill.
Between the years of 1546 and 1599 Kaspar Tagliacozzi,[4] Professor at Bologna, followed the art of rhinoplasty. His pupils published a book at Venice, describing his work in 1597, entitled “De Corturum chirurgia per insitionem,” which established the first authentic volume in restorative surgery. His operation for restoring the entire nose from a double pedicle flap taken from the arm was declared famous and the operation he then advocated still bears his name.
The great Ambroise Pare knew little of rhinoplasty except what he learned from hearsay. As an instance, he relates in 1575 that “A gentleman named Cadet de Saint-Thoan, who had lost his nose, for a long time wore a nose made of silver and while being much hurt by the criticisms and taunts of his acquaintances heard of a master in Italy who restored noses. He went there and had his facial organ restored, and returned to the great surprise of his friends, who marveled at the change in their formerly silver-nosed friend.”
Now again came a century of forgetfulness, the scientific world taking no cognizance of the work done until, suddenly, in 1794, a message came from Poonah, India, to the effect that an East Indian peasant named Cowasjee, a cowherd following the English army, was captured by Tippo Sahib, who ordered the prisoner’s nose to be amputated. His wounds were dressed and healed by English surgeons. Shortly after this the victim of this odd mode of punishment was befriended by the Koomas, a colony of potters, or, as others claim, a religious sect, who knew how to restore the nose by means of a flap taken from the forehead. They operated on him and restored his nose much to the surprise of Pennant, who reported the case in England.
Shortly following this, and in the same year, cases of similar nature are described in the Gentlemen’s Magazine (England), and Pennant’s “Views of Hindoostan.”
In 1811 Lynn successfully accomplished the operation in a case in England, and in 1814 Carpue published his[5] results in two cases successfully operated by him by the so-called Hindoo method.
France now took up the art of rhinoplasty. Delpech introduced a modification of the method of the Koomas in 1820, while Lisfranc performed the first operation of this nature in Paris in 1826.
In 1816 Graefe, of Germany, took up the work of Tagliacozzi but modified his method by diminishing the number of operations.
Bünger, of Marburg, thereupon, in 1823, successfully made a man’s nose by taking the necessary tegument from the patient’s thigh.
A still later modification in the art of rhinoplasty was that of Larrey, who in 1830 overcame a large loss about the lobule of the nose by taking the flaps to restore the same from the cheeks.
Among the better advocates of reparative chirurgery were Dieffenbach, v. Langenbeck, Ricard, v. Graefe (1816), Alliot, Blandin, Zeis, Serre, and Joberi, while Thomas D. Mutter, in 1831, published the results he obtained in America—his co-workers being Warren and Pancoast.
Although Le Monier, a French dentist, as early as 1764 originally proposed closure of the cleft in the soft palate, no one attempted to carry out his suggestion until in 1819 the elder Roux, of Paris, performed the operation. The following year Warren, of Boston, independently decided upon and successfully did an improved operation to the same end.
During the years 1865-70 Joseph Lister distinguished himself in the discovery and meritorious employment of carbolic acid as a means of destroying, or at least arresting, infectious germ life, the principle of which, now so fully developed, has advanced the obtainable surgical possibilities inestimably.
The credit of first collecting data of plastic operations belongs to Szymanowski, of Russia. In his magnificent[6] volume of surgery (1867), he embodies a somewhat thorough treatise on restorative surgery, leaving the subject to be treated more fully and independently, as it should be, to some other enthusiastic surgeon specialist. His work is the result of careful study of such operations on the cadaver, a method much to be recommended to the prospective or operating plastic surgeon.
Several years later, 1871, Reverdin added a valuable method to the still incomplete art, by introducing the now well-known circular epidermal skin grafts for covering granulating surfaces. Thiersch improved this method in 1886 by showing that comparatively large pieces of skin could be transplanted. Wolfe, of Glasgow, had also been successful in utilizing fairly large skin grafts.
Krause, however, improved upon all of these methods by transplanting large flaps of skin without detaching the subcutaneous tissue, a procedure which causes more or less injury to the graft in other methods, and by his method overcoming the subsequent contraction, heretofore a bad feature when the skin-grafted area had healed.
“The results of most plastic operations have been as satisfactory as the most sanguine could hope for or the most critical expect,” says John Eric Erichsen.
Many important additions have been made in the past few years—the outcome of untiring attempt and skill. Czerny replaces part of an amputated breast with a fatty tumor taken from the region of the thigh. Glück successfully repairs a defect in the carotid artery with the aid of a piece of the jugular vein. Glück, Helferich, and others have advocated implanting muscular tissue taken from the dog into muscular deficiencies in the human, due to whatever cause.
The transplantation of a zoöneural section into a defect of a nerve in the human was successfully accomplished by Phillippeaux and Vulpian.
Glück, who later restored a sciatic nerve in a rabbit by the transplantation of the same nerve taken from a hen, went so far as to restore a 5-cm. defect of the radial nerve of a patient by the employment of a bundle of catgut fibers, fully establishing the function of the nerve within a year’s time.
Guthrie has successfully replaced the organs and limbs of animals and has actually transplanted the heads of two dogs.
The transplantation of a toe, to make up a part of a lost finger, is proposed by Nicoladoni. Van Lair hints at the possibility of removing a part or a whole organ immediately before death to repair other living organs.
Von Hippel has successfully implanted a zoöcorneal graft from a rabbit upon the human eye, and Copeland has taken the corneal graft from one human and transplanted it upon the cornea of another to overcome opacity.
The transplantation of pieces of bone to overcome a defect of like tissue has been fully investigated by Ollier, v. Bergman, J. Wolff, MacEwen, Jakimowitsch, Riedinger, and others. They discovered that a graft of bone, with or without its periosteum, can be made to heal into a defect when strict antisepsis is maintained.
Von Nussbaum was the first to introduce the closing of an osseous defect by the use of a pedunculated flap of periosteum.
Poncet and Ollier employed small tubular sections of bone, while Senn has obtained excellent results from the use of chips of aseptic decalcified bone.
Hahn succeeded in implanting the fibula into a defect of the tibia.
On the other hand, cavities in the bones have been successfully filled by Dreesmann and Heydenreich with a paste of plaster made with a five-per-cent carbolic-acid solution, and at a later period by the employment of[8] paraffin (Gersuny) and iodoform wax, as advocated by Mosetig-Moorhof.
The thyroid glands taken from the sheep, it is claimed, have been successfully implanted in the abdomen of individuals whose thyroid glands had been lost by disease or otherwise.
Protheses of celluloid compound or gutta-percha and painted to resemble the nose or ear have been introduced with grateful result. Metal and glass forms have been used to replace extirpated testicles or to take the place of the vitreous humor of the eye (Mule).
Sunken noses have been raised with metal wire, metal plates, amber, and caoutchouc. Metal plates have been skillfully fitted into the broken bony vault of the cranium.
Lastly comes Gersuny’s most valuable method of injecting paraffin compounds subcutaneously for the restoration of the contour of facial surfaces and limbs, which is rapidly taking the place of extensive plastic transplantory and the much-objected-to metal and bone-plate operations for building up depressed noses and other abnormal cavities.
And the end of possibilities is not yet reached. The successful plastic surgeon has become an imitator of nature’s beauty to-day.
His skill permits of many almost unbelievable corrections of defects that would otherwise evoke the pity and too often the aversion of the onlooker, especially if these occur in the faces of those that have become marred in birth or age, by accident or disease. Withal, it is a noble, generous art, worthy of far more extensive use than it now enjoys.
The above fragmentary references include a number of plastic possibilities. They are introduced only in the sense of general interest to the cosmetic surgeon, the special and detailed subject matter herein given under the various divisions have to do only with plastic and cosmetic operations about the face.
The ideal operating room for the plastic surgeon need not necessarily be large, since it requires less work to render it aseptic. Furniture and possibly amphitheater accommodation are always a means of infection unless scrupulously cleansed, a task of time, difficult at best.
The room should be provided with large windows, with facilities for the introduction of the air from without. Two doors, and those well fitted, are all the room should have—but one being used, if possible.
The Walls.—The walls should be of plaster, smoothly laid and well painted, so that they may be readily washed down with antiseptic solutions—a daily morning rule. Glass or tiled walls are much used now and add considerably to the appearance and safety of the room, as plaster in time will crack, while the paint, owing to the heat of sterilizers or steam, often creeps and blisters, exposing an absorbing surface which readily wears down, exposing parts inaccessible for even acute cleanliness.
The Floors.—The floors of these rooms are now usually laid with tile mosaic or marble or a composition resembling linoleum. The base should be curved and all corners sloped off to improve drainage and to keep off dust and dirt.
Skylight.—A skylight of metal and glass is a valuable accessory. It should be fixed or never permitted to be opened during an operation.
Disinfection.—Spraying the room with an antiseptic is hardly necessary, since all germ life descends to the floor and can best be removed by washing with a 1-1000 bichlorid solution.
Should it be necessary to perform an unusually extensive operation in a private house, the room must be cleared of all furniture, pictures, drapery, and carpet. After plugging up the crevices in the windows and doors it should be well fumigated either with sulphur candles, as now commonly furnished, or, better, with formaldehyd.
The superiority of formaldehyd as a disinfecting agent is now well established. An illustration of an apparatus, largely doing away with the difficulties and dangers encountered in the use of the older and ordinary styles of the pressure or nonpressure type, is shown in Fig. 3. The main difficulty with these has always been their almost inaccessibility for cleansing purposes, and in such where this is not the case, the size of the aperture has been made so small that the inside could not be reached. In the pressure apparatus the tops are bolted on, making them exceedingly difficult to remove, with the result that the necessary cleaning was not properly attended to. The corrosive action of formaldehyd gas is such that under these conditions any apparatus would soon become useless.
In the type shown a single clamp arrangement is used (a). By the turning of the hand screw (b) two planed metal faces (the upper surface of the boiler and under surface of the cover) are brought together and sealed. When the cover (c) is removed the entire inside of the boiler is in sight and can be thoroughly cleansed, which should be done each time the apparatus is used. The pipes through which the formaldehyd gas passes after generation are arranged so that they can be taken off and cleaned.
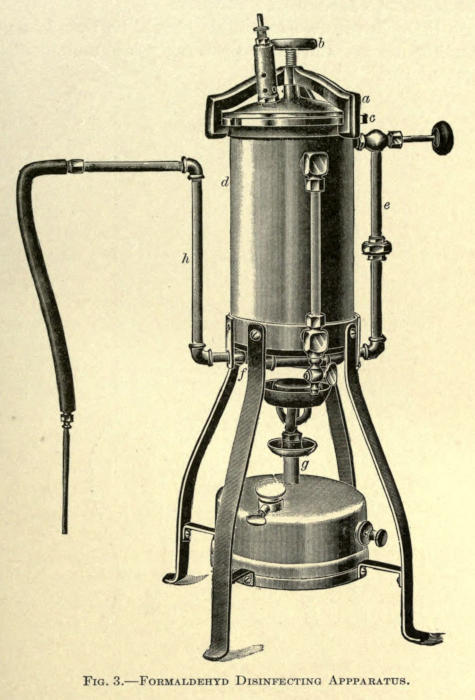
Fig. 3.—Formaldehyd Disinfecting Apparatus.
The gas is generated in the boiler (d) and passes out from the top, down through the pipe (e), and from thence through a series of pipes (f) underneath the boiler, which are subjected to direct heat from the lamp (g). By this means the gas becomes superheated, the polymerization of the formaldehyd is almost entirely prevented, and a dry gas is insured and given off at the pipe (h).
The room should be left closed overnight and thoroughly aired thereafter. The bare floor must then be scrubbed with hot water and soda and flushed with a three-per-cent carbolic-acid solution.
As little furniture as possible should be found in an operating room, and this preferably of undecorated enameled iron.
Instrument Cabinet.—For the instruments and dressings there should be a dust-proof cabinet of iron and glass, such as is shown in Fig. 4.
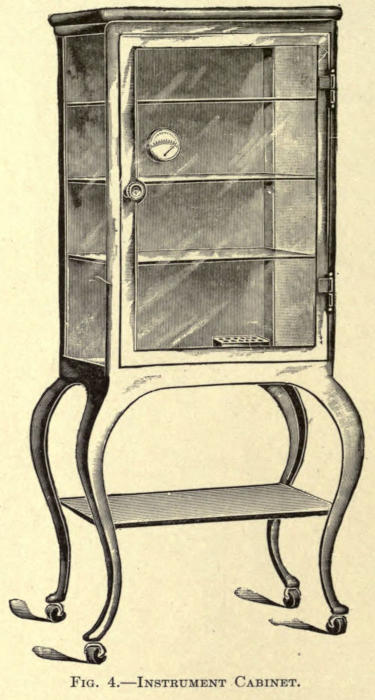
Fig. 4.—Instrument Cabinet.
Operating Table.—The operating table should be of like construction and as plain as possible. Its top can be padded with sterilized felt, protected from moisture by rubber sheets. A surgical chair of plain construction might suffice, inasmuch as most plastic operations cover but a small area and are usually about the head and often performed under local anesthesia. A chair with head rest is much more comfortable, adding much to the moral and physical comfort of the then conscious patient. A very desirable chair is shown in Fig. 5.
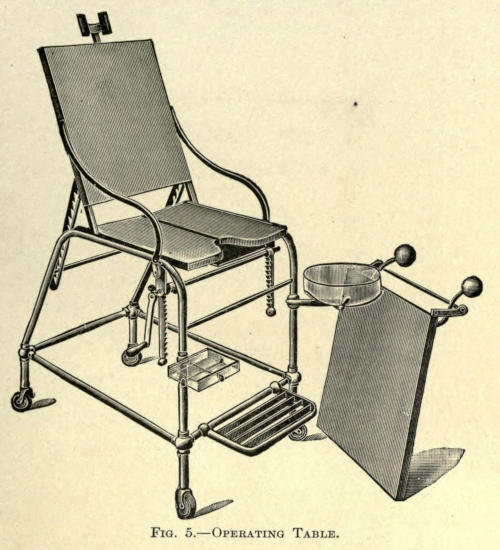
Fig. 5.—Operating Table.
Instrument Table.—An instrument table, such as is shown in the next illustration, is quite necessary, upon which dressings and instruments are laid during operation.[14] In this the frame is of white enameled iron and the top and shelf of plate glass.
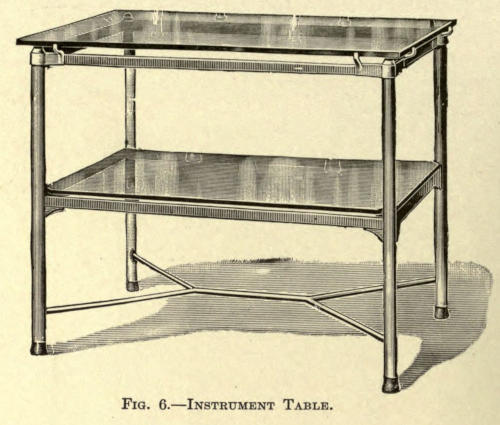
Fig. 6.—Instrument Table.
Irrigator.—An irrigator is often of service, especially in washing out the fine pieces of bone resulting from chiseling or drilling. In skin-grafting it may be used with sterilized three-per-cent salt solution as described later. The best irrigators are those of germ-proof or ground-glass stopper type. They are suspended from the wall by means of an iron bracket or pulley service or placed upon a movable enameled stand as shown in Fig. 7.
Irritating antiseptic solutions are to be avoided, their especial indication will be found under antiseptic care of wounds.
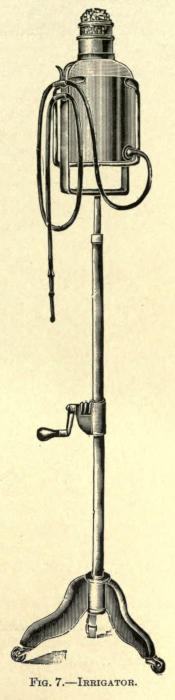
Fig. 7.—Irrigator.
All instruments should be of modern make, devoid of clefts or grooves, and having separating locks when possible. Wooden or ivory handles should be entirely discarded.[15] They should first be rendered free of dirt or dried blood by scrubbing briskly with a stiff nailbrush and hot water; then dried and placed in the sterilizer. The immersed instruments are boiled for five or ten minutes. There are many of such sterilizing apparatuses to be obtained, all made on the same plan, however, and consist of a copper or brass box and cover well nickel plated. Folding legs are placed beneath. A perforated tray is placed within for the immersion of instruments. An alcohol lamp with asbestos wick furnishes the heat.
One per cent of carbonate of soda added to the water prevents them from rusting. The simple subjection of instruments to carbolic-acid solutions or antiseptics of like nature is useless. (Gärtner, Kümmel, Gutch, Redard, and Davidsohn.)
From the sterilizer the instruments are placed in a glass tray containing a one-per-cent lysol solution. Knives, needles, and scissors should be immersed in a tray with alcohol, as a great number of antiseptics destroy their cutting edges. Glass or porcelain trays are best for this purpose. A sterilized towel being placed in the bottom of each for the better placing of instruments.
After operation all instruments should again be scrubbed with soap and hot water, immersed a moment in boiling water or a jet of live steam, dried with an aseptic cloth, and returned to the case.
A very effectual means of rendering instruments sterile is to place them in a metal box and bake them in the ordinary oven (200° F.) for one hour.
To preserve needles Dawbarn advises keeping them in a saturated solution of washing soda. Albolene has an unpleasant oiliness, but is otherwise good. Calcium chlorid in absolute alcohol is efficacious, but expensive. All rust accumulating on instruments must be carefully removed with fine emery cloth; this, however, is unnecessary if the soda solution is used as previously mentioned. It is well to occasionally dip the instruments (holding them with an artery forceps) into boiling water as they are used during operation.
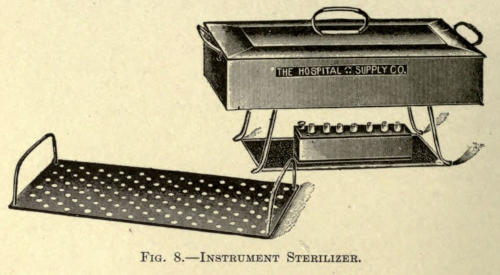
Fig. 8.—Instrument Sterilizer.
The hands of the surgeon and his assistants must always be thoroughly prepared before operation or dressing a wound. The mere immersion of the hands into an antiseptic solution is not sufficient to remove[17] germ life. The oily secretions of the skin and its folds, as well as the cleft about the nails and the nails themselves, are common carriers of infection and are cleansed only by the vigorous method of scrubbing with soap and water and then rendered aseptic by the use of proper media.
The aseptic hospital washstand, as shown in Fig. 9, will be found an ideal piece of furniture; it has a frame constructed of wrought iron, white enameled. The top is of one-inch polished plate glass, with two twelve-inch holes.
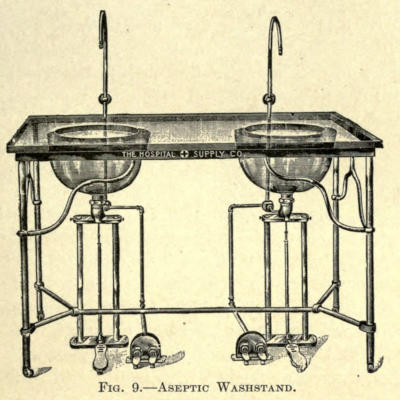
Fig. 9.—Aseptic Washstand.
The entire stand can be moved away from the wall, to permit of thorough cleaning of basins, supply pipes, etc. The basins are the best annealed glass, and are supported by nickel-plated traps, with connections for vent pipes. The water supply is controlled by foot valves, which enable the operator to draw either cold, medium, or hot water at will. The waste is also controlled by a foot valve, as shown.
The systematic law of cleansing the hands should be insisted upon at all times. Rules for the method followed might be displayed in abbreviated form in the operating room by glass or enameled signs hung on the wall over the basin and reading as follows:
YOUR HANDS
| I. | Clean nails. |
| II. | Scrub with very hot water and soap for five minutes. |
| III. | Wipe in sterile towel. |
| IV. | Brush with eighty per cent alcohol. |
| V. | Dip into antiseptic solution. |
Green soap is commonly used and is to be preferred to powdered or cake soap. The powder cakes and clogs the container in damp weather, while the latter collects impurities from the air. Synol soap, also liquid, is perhaps the most ideal, a two per cent solution of which forms an excellent lavage for cleaning instruments, as well as washing down furniture in the operating room.
The brushes to be used are of the common wooden-back, hard-bristle make, which can be boiled without injury. There should be several of these, marked on their backs as desired, so that one brush can be used for the one purpose only. In cleansing the hands, the forearms, and even the elbows, should be similarly treated. After scrubbing with soap, as directed, they are to be rinsed, dried with a sterilized towel, again scrubbed with alcohol, and then dipped or flushed with a bichlorid solution.
No woolen garments should be allowed to come in contact with the site of the operation, nor is it well to allow such material in the operating room while working.
Freshly laundered linen gowns of Von Bergman’s pattern, reaching to the shoes, should be worn. They[19] should contain half sleeves and be buttoned on the back. See Fig. 10. These may be sterilized in the steam sterilizer or washed in one-per-cent soda solution. When soiled or blood-stained they should be relaundered.
The operator may substitute the gown with a rubber apron of the Triffe pattern, reaching as high as the collar, but continuous washing quickly ruins them. See Fig. 11.

Fig. 10.—Von Bergman Operating Gown.
Fig. 11.—Triffe Rubber Apron.
The patient for all plastic operations should be carefully examined as to general health and past history. His healing powers should be at their best, as much depends on primary union. If he presents a syphilitic history,[20] it is well to place him under treatment, for a time, at least, before an operation is undertaken. The bowels should be regular. Sulphate of magnesium should be given each morning, before breakfast, for at least two days prior to operating, while his general condition may be improved by the employment of bitter and alterative tonics. Nux vomica with tinct. cinchonæ com., associated with essence of pepsin aromat., or lactopeptone, are very useful. This treatment is also carried on for several days, post operatio.
The success of an operation depends, first, upon the selection of the case; second, the selection of the method employed, and, third, upon the hygiene under which the patient undergoes convalescence. The patient must be given to understand, in many cases, that it is often necessary to reoperate, even to the extent of seven or eight operations, to bring about the desired result. The first result obtained with many cosmetic operations is not at all gratifying to the patient, and unless this is explained to him beforehand he may become discouraged awaiting the next operation and disappear, thus losing the opportunity of being pleased finally, while the surgeon is misunderstood and underestimated by narrow-minded judges and the ever-willing friendly advisers and critics—a consummation much to be avoided.
The part to be operated upon should first be closely shaven. The oily secretions of the area are next rubbed off with an absorbent cotton sponge saturated with alcohol or ether. Next, the skin is washed with hot water and soap or three-per-cent synol suds, then rinsed, and finally rendered aseptic with a bichlorid solution.
If the operation is to be done about the face a rubber cap is so adjusted as to cover the hair. If this is not obtainable sterilized bandages can be employed.
In operations about mucous membranes, as in the nose and mouth, the parts must be cleaned at short intervals with a solution of permanganate of potash or boric acid. The teeth must be cleansed with antiseptic soap, tartar is scraped off, and the mouth rinsed with a proper disinfectant. The corrosive sublimate, or carbolated solutions, owing to their toxic qualities, cannot be used. The preparation of wounds for reoperation, or where an operation is secondary to injury, is referred to later.
All clothing about the site of operation should be removed and rubber cloth placed to surround the field and cover the clothing. This should be covered again with sterilized towels. Everything that touches the patient after this has been done should be aseptic; indeed, hands employed during operation must be immersed from time to time in 1-500 bichlorid solution, and allowed to remain wet.
Natural or sea sponges are now little used in surgery, owing to their peculiar cellular construction. They invite and readily retain spores and germs, are difficult to clean, and require almost constant attention to be at all safe.
Many methods for rendering these sponges aseptic have been proposed, but at best the life of such a sponge is short and hardly pays for the labor and time expended. The absorbing power of a sponge is, of course, its essential quality. For plastic operations sterilized absorbent cotton made into small balls answers every purpose. These puffs of cotton are covered with gauze to prevent the fraying out of the fibers. To further improve them, their centers may be made up of cellulose or wood fiber. When an absorbent cotton sponge is moistened and squeezed out it does not answer as well, since its absorbing qualities are much reduced; the addition of the other material overcomes this.
A much-used and inexpensive sponge having great absorbing power is made in the form of a small compress of sterilized gauze held together with one or two stitches of thread. All of the above sponges are sterilized with the needed dressings and are burned after use. When removed from the sterilizer they are placed in a suitable basin containing six per cent sterilized salt water. It is well to place the receptacle close by the assistant who is[23] to sponge. An enameled iron basin rack, as shown in Fig. 12, answers the purpose best.
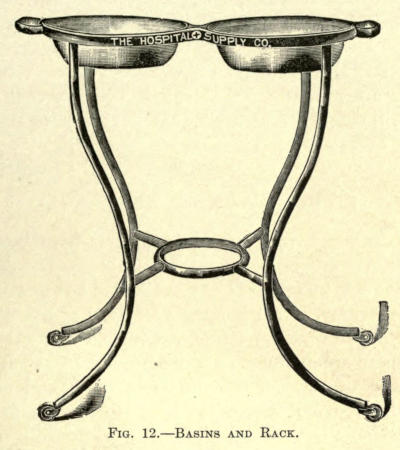
Fig. 12.—Basins and Rack.
The soiled sponges are thrown into a lower empty basin or one placed at the operator’s feet. As they are removed from the solution they are squeezed as dry as possible and pressed upon, rather than wiped across, the operative field. It must be remembered that the surgeon’s work must not be hampered by slow or inefficient sponging, and that this procedure must be quick and timely. It is well for the assistant to become accustomed to the habit of the operator.
The best assistant is one who has acquired a methodical and regular manipulation, a result dependent upon constant individual association; such a one is practically invaluable for the skillful performance of plastic surgery. He becomes not only familiar with the one thing, but cultivates a ready knowledge of the arrest of hemorrhage[24] by digital compression when hemostatic forceps would hinder the ease of work, besides cultivating a happy manner of holding retractors or spreading the edges of the incisions with the free hand. As in most of these operations hemorrhage cannot be controlled by the so-called bloodless method. The assistant must control the constant oozing by the gentle pressure of the sponge quickly applied at short intervals. When the sponges are squeezed out in salt solution, as hot as the hand will bear comfortably, capillary oozing is more readily overcome.
All dressings to be used in covering wounds, post operatio, or otherwise, must be as scrupulously clean and free from infection as the hands and the instruments of the operator. This is done by means of sterilization by dry heat or steam under pressure. For all minor cases, small apparatuses only are needed. They are usually made of copper, often nickel-plated, and so constructed as to contain a lower perforated instrument tray and another, placed above it, for dressings. The two are fitted into an outer copper receptacle with snugly fitting cover. A folding stand is furnished upon which this arrangement is placed, and an alcohol lamp with asbestos wick furnishes the heating power. The lower tray is covered with water which, by boiling, fills the upper compartment with steam evenly distributed and with sufficient pressure to accomplish sterilization in from thirty to sixty minutes. Metal hooks are provided with which the trays can be removed. A complete and compact outfit, as designed by Willy Meyer, is shown in Fig. 13.
In the above sterilizer, or in those of similar type, there is naturally more or less saturation of the dressings and the possibility, in the event of the entire conversion of the water contained therein into steam, of[25] injuring the instruments by excessive heat. To overcome this defect the Wallace sterilizer may be advantageously employed.
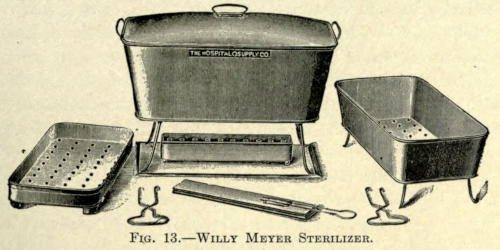
Fig. 13.—Willy Meyer Sterilizer.
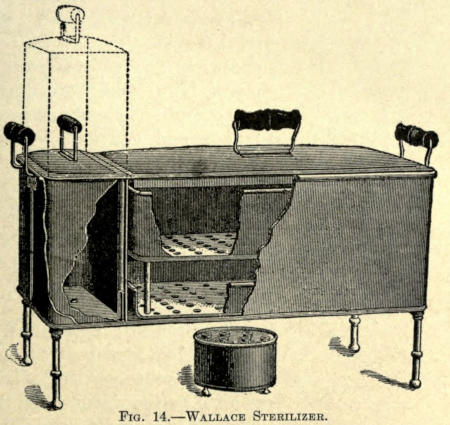
Fig. 14.—Wallace Sterilizer.
Wallace Sterilizer.—Its chief feature is the addition of a reservoir fitting with the separated sterilizer into the outer body. See Fig. 14. This reservoir automatically regulates the water and steam supply. It is filled with[26] water and inserted into the compartment provided for and adjoining the sterilizer. Through an opening in the bottom the water is permitted to escape into the sterilizer until the bottom of the latter is covered to a depth of ⅛ inch. As the heat is applied from the alcohol lamp this film of water is rapidly converted into steam.
The dressings arranged in the large tray are placed in the sterilizer and the supply of steam is maintained through the constant and steady flow of water from the reservoir, which compensates the evaporation in the sterilizer. In about twenty minutes the formation of steam in the top of the reservoir exerts sufficient pressure to force all the boiling water from the reservoir into the sterilizer to the depth of about 1½ inches. The tray of instruments is now inserted and the process continued for another ten minutes. Much less heat is required with this apparatus than with those of ordinary type, while sterilization can be continued uninterruptedly for one and one half hours, if need be.
Sprague Sterilizer.—The most perfect sterilizer is that of the Sprague type, in which a dry chamber is surrounded by steam under pressure. The apparatus is shown in Fig. 15.
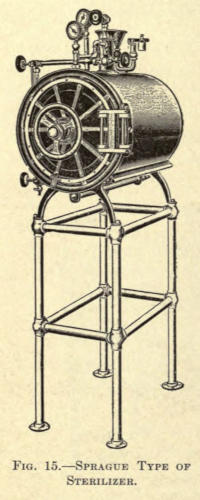
Fig. 15.—Sprague Type of Sterilizer.
Its cylindrical chamber is surrounded by two heavy copper shells, the space between which is occupied by the water. This compartment is entirely shut off from the sterilizing chamber, and as the steam is generated, the inner, or sterilizing, chamber becomes heated to a degree[27] nearly equal to that of the steam in the surrounding cylinder; this prevents any condensation of steam taking place in the dressings. By opening the lever-handled valve at the bottom of the sterilizer in the rear, and the valve to the right, on top of the sterilizer, and allowing them to remain open for a space of four or five minutes, a vacuum is formed in the sterilizing chamber. These two valves are then closed, the lower one first, and the steam from the outer cylinder is allowed to enter the chamber, by opening the left valve on top.
The contents should be allowed to sterilize for twenty or twenty-five minutes under a pressure of fifteen pounds. Then close the steam-supply valve; open the vacuum valve (right) and the lever-handled valve at the bottom; leave these open about the same time as in creating a vacuum at the beginning of the process; close both valves, then open the air-filter valve on the door, in order to break the vacuum; the door can then be opened and the dressings be taken out dry and absolutely sterile.
The steam-safety valve on this sterilizer is set at seventeen pounds, but it can easily be regulated should a higher or lower pressure be desired. The door used on this apparatus has no packing of rubber or other soft material which wears or shrinks in time, a steam-tight joint being formed by the bringing together of two plane metal faces on the door and sterilizer head. The door hinge is so made that these parts are bound to come together properly, without the use of excessive caution. Springs on such doors are liable to get out of order or need replacing, and are avoided in this apparatus. All that is necessary to lock or unlock the door is to turn the large hand wheel on the front; the locking levers then work automatically. These sterilizers are arranged for both gas and steam heat.
Sterilizing Plant.—For the ideal operating room the entire sterilizing plant can be had in combined form, as shown in Fig. 16. It consists of a dry-heat dressing apparatus,[28] just described, water and instrument sterilizers, all mounted on a white enameled, tubular, wrought-iron frame. The chamber of the dressing sterilizer is 8½ by 19 inches. The water sterilizer has a capacity of six gallons in each tank and is fitted with natural stone filters, thermometer, water gauge, safety valve, etc. The size of the instrument sterilizer is 8 by 15 inches and 6 inches deep, with two trays. Each apparatus in the above can be used independently of the other, all being arranged for gas-heating.
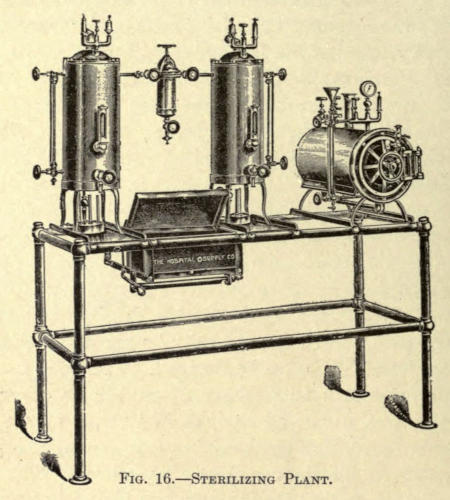
Fig. 16.—Sterilizing Plant.
Dressing Cases.—All dressings should be sterilized immediately before operation, and not laid away for later use, as often done. As the aseptic material is taken from the sterilizer it is to be placed in glass cases provided therefor, from which they are removed, as needed, during the operation.
A simple glass case, as shown in Fig. 17, may be[29] used, or, better still, the same can be obtained in combination with an instrument table, as shown in Fig. 18.
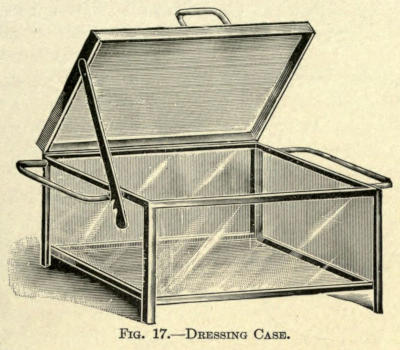
Fig. 17.—Dressing Case.
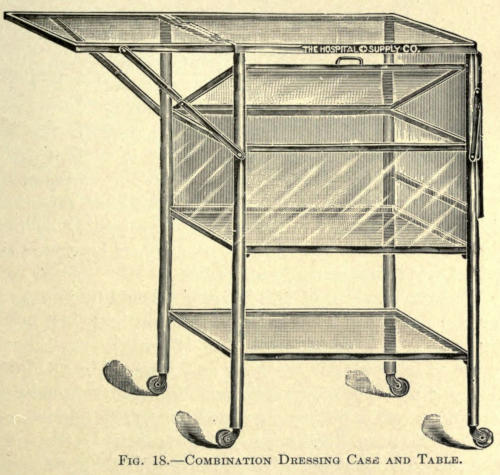
Fig. 18.—Combination Dressing Case and Table.
Waste Cans.—All soiled dressings and sponges should be immediately thrown into an enameled iron pail furnished for the purpose. At no time must soiled dressings or sponges be thrown upon the floor, where they are walked over, soiling the floor and, by drying, contaminating the air of the room. Cans for this purpose are made of steel, enameled, of the form shown in Fig. 19.
The contents of the can must be taken from the room after each operation and burned. The can should be flushed with carbolic solution, and returned to the operating room.
Fig. 19.—Waste Can.
(Ligatures)
Silkworm Gut and Silk.—In plastic surgery silkworm gut and silk are used extensively. Rarely is ordinary catgut resorted to, because it is absorbed before thorough union takes place, besides being a source of infection, either primarily from imperfect sterilization or by taking it up from the secretions of the deeper layer of skin not affected by external antiseptics.
The sterilization of silk is accomplished by boiling it for one hour in a 1-20 carbolic solution and then keeping it in a 1-50 similar solution (Czerny). Or it may be boiled in water for one hour and retained in a 1-1,000 alcoholic solution of corrosive sublimate. Ordinarily it may, however, be simply subjected to boiling and steamed in the autocleve. Silkworm gut is treated in the same manner. It has greater tensile strength than silk, and[31] for that reason the thinner varieties are to be preferred to ordinary silk.
Catgut.—It is far more difficult to prepare catgut, but, since it is necessary for ligation, the following methods may be considered best:
The commercial catgut as made from the intestines of sheep, is wound snugly upon a rod of glass and thoroughly brushed with soft soap and hot water. It is then rinsed free of soap, wound upon small glass spools, and placed for forty-eight hours in a one-per-cent alcoholic bichlorid solution, composed of bichlorid of mercury, 10 parts; alcohol, 800 parts; distilled water, 200 parts. The turbid fluid produced by first immersion is changed. Before using, the spools are placed in a glass vessel contain containing a 1-2,000 sublimate alcohol (Schaffer), made up as follows:
| Bichlorid of mercury | gr. vj; |
| Alcohol | ℥x; |
| Distilled water | ℥iiss. |
These glass cases are obtainable for the purpose and contain a second perforated compartment for the ligatures passing through rubber valves placed into the openings (Haagedorn).
Catgut is generally prepared by soaking in oil of juniper for one week and then retaining it in absolute alcohol (Kocher), or a 1-1,000 alcoholic sublimate solution.
Another method for strengthening catgut, as well as to prevent its too rapid absorption, is to chromatize it. This is done as follows:
The catgut is placed in sulphuric ether for forty-eight hours, then treated for another forty-eight hours in a ten-per-cent solution of carbolized glycerin, followed by a five-hour subjection to a five-per-cent aqueous solution of chromic acid (Lister). It is allowed to remain in the latter forty-eight hours, then placed in an antiseptic, dry,[32] tightly closed receptacle, and finally soaked in 1-20 carbolic solution before using.
The formaldehyd method of Kossman is to immerse the gut in formaldehyd for twenty-four hours, then washing with a solution of chlorid and carbonate of sodium and retaining it in the same solution. The catgut in this procedure swells and its strength is much impaired in this way.
Any of the above methods are not above criticism, however, rigid as they may seem, bacterial growths having been obtained with nearly all of them.
The dry-air method (Boeckman, Reverdin) is reliable, but the subjection of catgut to dry air at a temperature of 303° F. for two hours results in making it tender and less pliable.
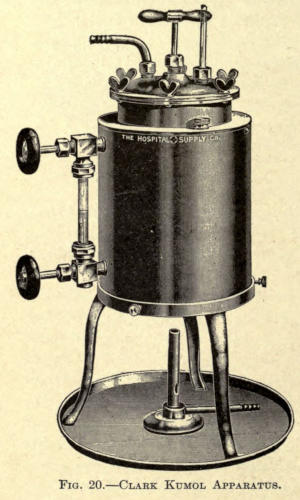
Fig. 20.—Clark Kumol Apparatus.
The Kumol method (Kronig) is considered the most reliable, even under the severest tests. This mode of sterilization is accomplished as follows: A specially devised apparatus of brass, with a cast-bronze top, both thoroughly nickel-plated, is used. The apparatus of J. G. Clark, as shown in Fig. 20, will be found excellent. The kumol is retained in a seamless cylinder, 8 by 8 inches, which is surrounded on the sides and bottom by a sand[33] bath; the flame, impinging on the bottom, heats the sand, thereby insuring an even heat to the inner or sterilizing cylinder. The catgut, in rings, is placed in a perforated basket hanging in the cylinder, which can be raised or lowered at will; after drying for two hours at 80° C., the basket is dropped, and the catgut immersed in the kumol, at 155° C., for one hour; the kumol is then drawn off through a long rubber tube, and the catgut dried at 100° C., for two hours; it is then transferred to sterile glass tubes plugged with cotton.
Prepared catgut of the various sizes can now, however, be purchased in the market, and that offered by the better firms of chemists is quite reliable and may be safely used for all plastic surgery about the face. It is supplied in glass tubes, either in given lengths, as in the Fowler type, in which the hermetically sealed tube is U-shaped or on glass spools placed in glass tubes, not sealed, but closed by a rubber cap, through which the desired length of ligature is drawn and then cut off.
These are solutions used for the destruction of and to arrest the progress of microörganisms that have found their way into wounds—the cause of sepsis, as exhibited by fever, suppuration, and putrefaction. These preparations are called antiseptics and are used to render parts aseptic. They vary much in their destructive power, effect on tissue, and toxic properties. The reader is referred to a work on bacteriology for the specific knowledge of such on germ life.
The antiseptic treatment of wounds was founded by Joseph Lister, 1865-70, then called Listerism. His one chemical agent to accomplish this was carbolic acid, but many such and more effective agents have been added since that time, all differing in their specific properties and each having, for the same reason, its particular use.
The following group of antiseptics has been chosen with a view of giving the best selection, to which the author has added a short description of each, so that the surgeon may choose one or the other, as the occasion may demand. As a rule, an operator cultivates the use of a certain line of antisepsis, especially in this branch of surgery, experience being the best guide; yet it is hoped he may find certain aid from those referred to, their particular use being pointed out from time to time, as the author has had occasion to prefer one or the other.
Alcohol (absolute).—This is a well-known antiseptic, but, because of its ready evaporation, is especially used for the hands, as described, and to cover sharp-edged instruments after sterilization.
Aluminum Acetate (Bürow, H. Maas).—A powerful, nontoxic antiseptic. Is used only in two- to five-per-cent solution. According to Primer, it arrests the development of schizomycetes, and in twenty-four hours destroys their propagation. It readily removes offensive odors of wounds; its great objections are that it injures the instruments, and, because of its astringent nature, roughens the skin of the hands. This, however, makes it particularly useful for sponging to arrest capillary oozing.
Boric Acid (Lister).—Not a powerful, but nonirritating, antiseptic. For this reason it is used extensively in cleansing mucous membranes, and, when associated with salicylic acid, as in the well-known Thiersch solutions, composed of salicylic acid, 2 gms.; boric acid, 12 gms.; water, 1,000 gms., is much used in skin-grafting operations. It is not very soluble in cold, but readily in hot, water and alcohol. The saturated solution is prepared by adding ℥j to the pint of boiling water.
Benzoic Acid.—Nonirritating, moderate antiseptic (Kraske); is prepared in 1-250 solutions. Soluble in hot water and alcohol, but sparingly in cold water.
Carbolic Acid (Phenylic Acid).—Not a powerful, but a much-used antiseptic. The purest acid should be used. It appears as a colorless crystalline solid, liquefied by the addition of five per cent water. If more water is added the solution becomes turbid, clearing when 1-2,000 is reached.
It is readily soluble in glycerin, alcohol, ether, and the fixed volatile oils. Solutions in alcohol and oils have no antiseptic effect (Koch). The 1-20 aqueous solution is recommended by Lister.
The aqueous solutions used in surgery are 1-20 and[36] 1-40. The weaker is used for the operator’s hands, to cover instruments, as already mentioned, and to impregnate sponges. The stronger solution is used for the carbolic spray, to cleanse the unbroken skin about the site of operation, and to disinfect wounds. Either solution, when applied to an open wound, whitens the raw surface, coagulates the albumen, and causes considerable irritation, which subsides quickly and is followed by numbness.
Such solutions, by virtue of their irritant nature, increase the serous discharge from a wound for about twenty-four hours, for which proper drainage must be provided, as by its collection it would add to the danger by increasing inflammation and suppuration, and, by absorption, even produce toxic effect generally.
When a cold solution is used it should be prepared by vigorous stirring to separate the globules of the acid. Hot water insures perfect distribution. After an infected wound is washed with it, the solution should not again be used, nor should any of the acid be permitted to remain in the spaces about the wound. It will be found that many patients cannot tolerate such dressings, and that others must be substituted.
Large surfaces should never be exposed to carbolic solutions, because the skin absorbs them readily, followed by untoward results. Dangerous symptoms have been known to result from the internal administration of seven drops of the acid, and fatal termination has followed its use as a surgical dressing (Bartley).
Mild acid poisoning is first noted in the urine, which turns olive green. If the agent is continued, the urine appears dark and turns almost black on standing. The coloring is due to the presence of indican. If the absorption is not prevented beyond this there is dull frontal aching, tinnitus aurium, dizziness, fainting, severe and uncontrollable vomiting. Untoward symptoms are noted by albuminuria, total absence of sulphates in the urine,[37] a contracted and inactive pupil, elevation of temperature, unconsciousness, muscular contraction, and death.
The treatment consists in immediately removing the cause and employing another antiseptic. Support the patient with stimulants, freely given. Cracked ice and brandy to allay the vomiting. Small doses of sodium sulphate, frequently repeated, as a means of converting the acid into nonpoisonous sulphocarbolate (Bauman). Albumen and milk internally. Magnesium sulphate, five per cent.
Chromic Anhydrid.—Improperly called chromic acid. Made by adding one and one half parts sulphuric acid, c. p., to one part of concentrated solution of dichromate of potash. Appears in saffron-colored crystals. It acts as a caustic upon tissue, and, although a splendid antiseptic, cannot be used for such purposes, but is well adapted for the preparation of catgut, as mentioned.
Creolin.—Is an antiseptic prepared from coal by dry distillation, and is used to stimulate granulations, being much more powerful than carbolic acid. It is nonirritant and practically nontoxic. Used in two-per-cent aqueous solutions, in which it appears as a turbid but effective mixture. It is well suited for cleansing the hands, a five-per-cent solution having none of the irritating or anesthetic effect of carbolic acid. Owing to the opacity of the aqueous solution, it is not suitable for the immersion of instruments for operation.
Eucalyptol (W. Schultz).—A nonpoisonous volatile oil of considerable antiseptic power. Soluble in alcohol, and used in three-per-cent solution. It is claimed to quickly reduce the temperature in a wound. It was much used by Lister on gauze dressings, the formula of which is given elsewhere.
Glycerin.—It is said to have certain antiseptic power, but is used principally as a staple solvent of carbolic and boric acid. Soluble in all proportions in water and alcohol.
Hydrargyrum Bichloratum Corrosivum (v. Bergman, Schede, Buchholz, Billroth, R. Koch).—The most valuable and effective, although the most toxic of all antiseptics. It appears as a white crystalline powder. A 1-50,000 watery solution is efficacious as a germicide (Koch; anthrax bacilli killed by 1-20,000 solution). Albumen decomposes the bichlorid, forming a white insoluble precipitate, albuminate of mercury. The same effect takes place in aqueous solutions allowed to stand for a time—the resultant being either calomel or metallic mercury. The addition of sodium or ammonium chlorid or a weak acid, such as tartaric, prevents this. As much sodium as of the sublimate, weight for weight, should be used (Koch). When tartaric acid is used for this purpose, five times the weight of the sublimate is employed.
For all surgical purposes, except in irrigation, solutions of 1-500 and 1-1,000 are used. For the sterilization of wounds and during operations a 1-3,000 is employed.
For the ready preparation of such solutions sublimate tablets can be obtained, properly mixed with one of the above-named salts. The dyed tablets are to be preferred, to prevent error on the part of the user. Tablets containing 1 gm. sublimate, 1 gm. sodium chlorid, and colored with eosin, are advocated by Angerer.
As metallic substances immediately decompose the bichlorid in solution, instruments cannot be placed in it, nor may it be kept in metallic vessels, glass being preferred.
Alcoholic solutions of sublimate are used to cover catgut, silk, and rubber drainage tubes.
Since sublimate is extremely toxic, great care must be used to prevent its absorption or retention in wounds. A strong solution must immediately be followed by a weaker one.
Toxic symptoms resemble arsenic poisoning very much, and are ushered in by an acute irritation of the wound, especially if moist sublimated gauze has been[39] used, vertigo, and vomiting. The mucous membrane of the mouth becomes affected, followed by salivation and bleeding from the gums. There may be intestinal hemorrhage and an inflammation of the entire intestinal tract and kidneys, increasing in severity and resulting in death.
The early symptoms must be at once met by removal of the cause. Albumen and milk should be given internally, with stimulants as needed. The mouth is to be rinsed out at frequent intervals with a saturated solution of chlorate of potash.
Hydrogen Peroxid (Love).—A powerful nontoxic antiseptic. It is used in five- to fifty-per-cent aqueous solutions, and is most efficacious in suppurating wounds, in which it destroys the microörganisms of pus. It foams actively when brought in contact with the latter, and is said to render a wound aseptic by one or two applications. A standard preparation of known strength must be obtained, however, to get good results.
Iodin.—A very powerful nonirritating antiseptic. Used especially for washing wounds. The proper solution is made by mixing two drams of the tincture (℥j iodin to ℥Oj alcohol) with one pint of warm water (Bryant). The one-per-cent solution of the trichlorid is equal in its effectiveness to a four-per-cent carbolic solution (Langenbuch).
Lysol.—Very similar to creolin, both in composition and effect. Is nontoxic, and employed in two-per-cent aqueous solution. Appears as a soapy liquid, and forms a clear solution with water.
Potassium Permanganate.—An active disinfectant, quickly destroying the odor of decomposition, and for that reason is splendid for the washing out of foul wounds. It is nonpoisonous, and has moderate antiseptic power—the five-per-cent solution killing resting spores. Its effect is limited to a short time only, as the secretions from a wound decompose and precipitate it into an inactive[40] form. It is employed in aqueous solution, differing in color from light ruby to dark brown; that is, 1-1,000 to 1-100. The solution, known as Condy’s Fluid, has a strength of 1-1,000.
Salicylic Acid.—A derivative of carbolic acid, and an effective nonirritating antiseptic. It is only slightly soluble in cold water, 1-300. When combined with boric acid, it becomes more soluble. This antiseptic cannot be used for instruments, however, as it corrodes them. Its other objections are that it evaporates quickly from dressings and that it is expensive.
Sodium Chlorid.—Is a common agent used for the irrigation of putrid wounds in two-per-cent solution. For irrigation during aseptic operation and for covering sterilized sponges it is used in eight-per-cent solution (v. Esmarch). This corresponding to the normal salt solution. Its use in connection with corrosive-sublimate solutions (Maas) has been referred to.
Thymol (Rancke, Bouillon, Paquel).—The aromatic principle of thyme. Efficient as an antiseptic in 1-1,000 aqueous solution. It has a pleasant odor, and is nonirritant and nontoxic. Exhibited in colorless crystals. An excellent solution is prepared as follows:
| ℞ | Thymol | 20 | parts |
| Alcohol | 10 | ” | |
| Glycerin | 20 | ” | |
| Aquæ | 1,000 | ” |
It is used especially in washing out cavities where carbolic acid cannot be employed, and for cleansing mucous membranes preparatory to operation.
Zinc Chlorid (Morgan, Bardeleben, Billroth).—Extensively used as an antiseptic, especially in the oral cavity, where, by sealing the lymph spaces with a plastic exudate, it hinders the absorption of septic matter. It is only slightly antiseptic, however, in ten-per-cent aqueous solution. Zinc chlorid represents the active agent in[41] Burnett’s fluid. May be effectively employed in the proportions of from twenty to forty grains to the ounce of water. Care must be exercised to prevent its retention in alveolar tissue, since it may occasion serious sloughing. As a cleansing agent for infected wounds it is of great value, although the sulphocarbolate of zinc may be preferred, as it is less irritating and less toxic.
Peroxoles.—Beck has introduced a group of preparations, known as peroxoles; liquid antiseptics containing a solution of hydrogen peroxid in combination with other disinfectants. The preparations are composed of from thirty-three to thirty-eight per cent alcohol, about three per cent of hydrogen peroxid, and one per cent of thymol, menthol, or camphor, the name given them being according to the last ingredient—thymosol, menthosol, or camphorosol. The association with these disinfectants greatly increases the antiseptic power of hydrogen peroxid. Aqueous solutions containing ten per cent of the peroxoles are usually employed. These correspond to a one-per-cent solution of mercuric chlorid, and possess a more energetic action than five per cent carbolic acid.
Aristol (Dithymol Di-iodid) (Eichhoff).—Reddish-brown powder containing forty per cent iodin. Soluble in ether, chloroform, and fatty oils, sparingly in alcohol. Must be kept in dark glass bottles. Is incompatible with corrosive solutions. Used externally as iodoform.
Dermatol (Bismuth Subgallate).—An odorless yellow insoluble powder, containing fifty-three per cent Bi₂O₃.
Iodol (Tetraido Pyrol) (Kalle).—A light grayish-brown powder, containing eighty-nine per cent iodid. Slightly soluble in water, soluble in alcohol and chloroform. Its action is very similar to iodoform, and has taken its place to a great extent, first, because it is odorless, and secondly, because any quantity used exerts no[42] toxic effect (Wolfenden). It is dusted upon the wound. Its action is due to the liberation of iodin, which acts upon the albuminous elements, and the ozone set free oxidizes the products of decomposition. It has a slight escharotic effect, forming a thin crust over the surface to which it is applied, thus effectually remaining in constant contact with it. That it is quickly absorbed is shown by its presence in the saliva and the urine.
Orthoform (Methyl Ester of Meta-Amido-Para-Oxybenzoic Acid).—Nonpoisonous, white, odorless powder of moderate antiseptic power, and well suited for wounds involving mucous membranes. It has a decided anesthetic effect, lasting for several hours upon painful wound surfaces.
Iodoform (Formyl Iodid, Féréol).—A lemon-yellow crystalline powder of penetrating, saffronlike odor. Contains ninety-seven per cent iodin. Insoluble in water, but forms solution with alcohol, ether, chloroform, and the fixed volatile oils. Has a decided stimulating effect on wounds by preventing putrefaction and deodorization (Mikulicz). Its antiseptic value has been much discussed, but practically it has found favor with the majority of surgeons. According to research, iodoform is a powerful antiseptic, from the fact that the product of its decomposition in the presence of germ life renders the ptomains in a wound inert, thus preventing suppuration, or at least checking the absorption of such, which is often a serious matter in infected wounds. It is not sterile, and may contain ptomains which in themselves would produce pus, but as associated with the iodoform do not occasion it.
The dressing or treatment of wounds, considered herein, embodies particularly that practiced by the surgeon in the performance of plastic operations.
The elasticity of the skin is especially serviceable in bringing about desirable restorative results, but, owing to its extreme vascularity and the infrequent supply of venous valves, as in the face, there is considerable danger of infection, with rapidly spreading septic inflammation.
Sutured Wounds.—Before the wound is closed all hemorrhage must be arrested, either by catgut ligature, in exceptional cases, and by torsion or pressure, as generally practiced. Gauze sponges dipped into hot sterilized solution are most suitable for the latter purpose.
The edges of the wound must be coapted perfectly by cutaneous sutures of sterilized silk of suitable thickness. Formaldehyd catgut is often used because of its limited absorption. Ordinary catgut should not be employed, as its early absorption interferes with obtaining the proper union, and by becoming softened invites sepsis.
The wound, if small, may be powdered over with any of the antiseptic powders, such as aristol or iodol. It must be remembered that such powders form a hard crust with the serous oozing of wounds, which, by reason of pressure from the dressing applied over it, is very liable to separate the edges of the wound, thus increasing the width of the scar, a very important factor in facial surgery.
Where perfect apposition has been made, the dusting powders may be used and a covering of Lister’s protective silk plaster placed over it. The edge of the strips of plaster must be incised at distances of about ⅛ inch, so as to snugly take on the curvature of the parts and at the same time thoroughly seal over the area to prevent subsequent contamination.
The plaster is made of taffeta silk, preferably of flesh color, coated on one side with copal varnish and a mixture prepared as follows:
| ℞ | Dextrin | ʒj; |
| Starch | ʒij; | |
| Carbolic acid | ℥ij. |
When applied, it should be moistened with an antiseptic solution only. This can be applied only to dry surfaces, however, and should be rarely used, since subsequent hemorrhage or oozing will raise the plasters, inviting sepsis.
It is better, however, in all cases to employ several layers of an antiseptic gauze, such as fifteen-per-cent iodoform or boric-acid gauze to cover the wound, and back it with absorbent cotton, over which a bandage or the silk protective is applied to retain it. The gauze absorbs the secretions, at the same time rendering them harmless.
At no time should cotton be placed next to the wound, as it forms a hard mass with the secretions, the removal of which requires enough force to injure or hazard the union of a new wound. Nor should a plaster dressing be pulled off without thoroughly moistening it first, withdrawing the various layers one by one. The gauze, when moistened, readily leaves the wound without injurious traction. An excellent dressing for small, dry wounds, and one that causes little tension, is collodium, or, better, iodoform-collodium painted over the surface. The latter may be prepared as follows;
| ℞ | Iodoformum | 5j; |
| Collodium | 5x. | |
| [Küster.] | ||
To this may be added oil of turpentine or castor oil, which permits of greater flexibility. Boric lint, applied wet, is also good. It must be moistened thoroughly before removal. Larger wounds should be dusted over with one of the powders mentioned and covered with folds of gauze and absorbent cotton, held in place with gauze bandages.
Such dressings are allowed to remain until the sutures are taken out, unless there is sign of soiling. As these secretions readily decompose, it is best to remove the cotton and upper layers of gauze and renew them every day, or as often as is necessary. The wound, in this way, is not disturbed whatever, and the antiseptic properties of the lower fold of gauze is sufficient to keep the wound surface clean.
In most superficial wounds it is best to remove the sutures at the end of forty-eight hours, unless there are reasons for retaining them longer, as the coapted surfaces are then sufficiently united to permit of other dressings, such as aseptic plaster, now extensively used. Before these are applied the skin is washed with alcohol or ether to assure a dry surface to facilitate adhesion.
Sutures drawn as stated leave no possibility of stitch scars and reduce the occurrence of possible stitch abscess to a minimum. As there is always slight oozing following their removal, aristol or iodol may be powdered over them before applying the plasters. This brings us to the rather late question of sutureless coaptation of superficial incisions.
Sutureless Coaptation.—This method, first practically demonstrated by Bretz, may be used with considerable advantage in wounds about the face, and overcomes the strain of individual sutures, besides avoiding the possibilities of stitch infection.
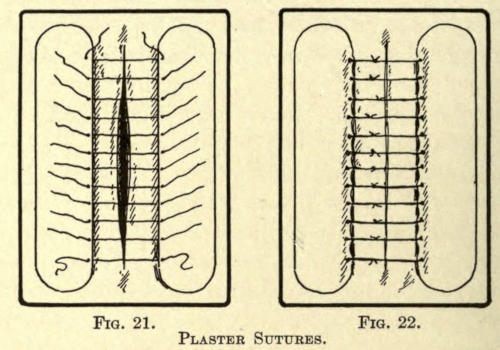
Fig. 21. Fig. 22.
Plaster Sutures.
The method involves the proper placing of strips of plaster at either or opposite ends of the wound. The distance between the incision and the edge of the plaster must not be less than ¼ inch or more, according to the length of the wound and its position. In place of the strips of rubber adhesive plaster, the aseptic Z. O. plaster should be substituted to overcome the objections of the infections therefrom.
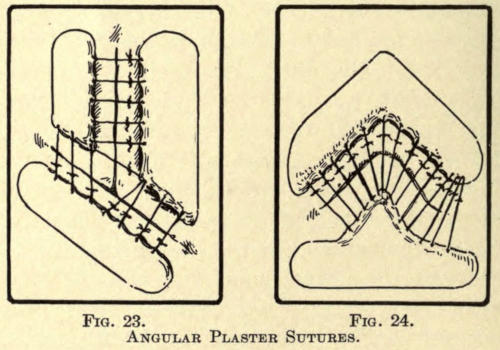
Fig. 23. Fig. 24.
Angular Plaster Sutures.
The inner edges of the plasters are raised slightly, and interrupted sutures are inserted through them instead[47] of the skin (see Fig. 21). They are then tied as shown in Fig. 22. In angular incisions the plasters are cut as desired to insure perfect coaptation, as in Figs. 23 and 24. The advantages of this method, besides those already mentioned, are that the wound is always open for inspection and permits of free drainage. If thought best, a small strip of iodoform gauze may be placed over the threads or even under them, if there is little tension.
Since the introduction of the aseptic Z. O. (Lilienthal) strips, the above method may be discarded as unnecessary and requiring too much time for their application. Strips of the antiseptic plaster are placed across the wound at right angles, or, if the surface be a curved one, obliquely to the wound. The plasters are furnished in strips of the width desired, packed in two germ-proof envelopes. They are extremely adhesive to dry surfaces. Besides being aseptic, they are slightly antiseptic and nonirritating. The strips are placed in position, leaving an open space between them while the assistant brings the edges of the wound into position.
Where there is tension of the parts this method is not to be employed. The wound may be dusted as when sutured and dressed in the same manner. The plasters are removed about the sixth day by drawing the ends of the strips toward the wound. Their second application is unnecessary, regular dressings being substituted.
From the above it must not be inferred that all plastic wounds are amenable to the above methods, because many require specific treatment, as later described.
Granulation.—Wounds left open for granulation should be dusted over with some stimulating antiseptic powder, such as aristol or boric acid, and then covered with iodoform or borated gauze. The granulating surface must be gently washed with a mild solution of peroxid.
Prolific hypertrophic granulations, that jut out over the surface, are touched with a lunar caustic point, avoiding the epithelial edge of the wound, where it causes considerable[48] pain. Pale and loose granular points should be scraped away with the sharp spoon curette to hasten better growth.
If the skin edges are thickened and curled upon themselves, it may be best to curette or to reduce them by cauterization, so stimulating epitheliar spreading. Sterile gauze is then loosely laid upon the surface, backed with a highly absorbing material, such at charpie cotton (Burns), wood wool, and poplar sawdust, retained in gauze bags (Porter). The absorbing layer should be light and pervious to the air, to facilitate not only free absorption, but ready evaporation of the secretions.
Changing Dressings.—All dressings must be absolutely sterile and all precautions, as primarily carried out, must be followed in changing them.
It is rather infrequent to use permanent dressings in plastic surgery, but where the wound appears aseptic, with a dry serous crust over the line of healing, it should not be disturbed except for mechanical reasons. The latter are caused by the coagulated mixture of the wound secretion and the antiseptic powder used, often aggravated by the median knotting of sutures or the careless disposition of the loose suture ends. Not too much can be said of carefully folding the free silk suture ends at right angles to the incisions. The ends, moistened subcutaneously, are very liable to take on septic infection and communicate it to the wound—crowded into the very wound. When becoming embodied in the coagula of serum and antiseptic powder it prevents, by pressure, perfect union, causing a wider scar at such point, as well as endangering the asepsis of the wound by being pulled off accidentally, thus tearing it open and bringing on hemorrhage.
The appearance of the resulting scar in facial surgery is often of as much importance to the patient as the operation itself, therefore, all care should be exercised in bringing about the very best result.
For this reason, a patient in poor health should not be operated upon, and any erosion of the skin about the seat of operation should be thoroughly healed before attempting plastic work. Aristol dusted on an abrasion will heal it quickly.
If hemorrhage follows the dressings of a wound, the dressing should be removed and the hemorrhage controlled by pressure, unless severe, and be redressed. Moist blood decomposes readily and is a source of early infection, unless careful drainage under antisepsis is established. At no time should any part of the wound be unnecessarily exposed directly to the air. For small wounds, silk protective plaster may be used to cover the gauze dressing, while sterile gauze bandages should keep dressings of large area in place.
Bandages, when changed, should be cut away with the aid of the Lazarewitch angular bandage scissors and not be unwound. It is quicker and the undue pulling of such, when glued by secretions, is liable to disturb the healing of wounds and even result in the tearing out of sutures.
The patient should never be intrusted to dress wounds himself. In cases where the dressings cannot be changed frequently proper precautions for drainage and comfort must be observed. The temperature of the patient should be taken twice daily; any elevation thereof may indicate septic infection and demand immediate attention.
When a portion of the ear, nose, or lip has been severed by injury, the part may be put back into place and held by sutures and aseptic Z. O. strips, powdered with aristol and properly dressed. Union usually takes place, even in the most unexpected cases. None but incised wounds of such nature should be covered hermetically with collodium or plaster, as bruised surfaces so often in this kind of injury require perfect drainage. The retention of secretions produces infection, generally resulting in the entire loss of the part.
Wounds of the Mucous Membrane.—Wounds of the mucous membrane should be carefully drained and cleansed freely at frequent intervals, especially those about the mouth. Wounds of the cheek, if including the mucous membrane, should be especially cared for, as there is here the increased danger of infections from the secretions of the mouth.
Pedunculated Flaps.—When pedunculated flaps are left free of other attachment, for reasons later mentioned, they must be dressed as granulating wounds. Here it becomes necessary to support the loose piece of skin in such a way as to overcome circulatory obliteration. Unnecessary handling is always to be avoided. The following method has been used with the best results by the author.
The flap is not dressed until all hemorrhage has ceased. A small pad of sterilized or borated absorbent cotton is covered lightly with ten-per-cent iodoform gauze—cigarette fashion. The surface of this roll drain is powdered well with aristol or iodol and it is gently placed beneath the flap so that it rests easily upon the same. A second and somewhat larger pad or roll of like construction is placed next to the skin surface of the flap. This is held in position by silk protective plaster or several layers of gauze bandage, gently, though snugly, applied.
The flap thus dressed should not be subjected to pressure, often requiring considerable care on the part of the patient, especially during the night. Undue pressure will induce sloughing and must be avoided, even at the expense of comfort to the patient.
This dressing may be changed the second day, when the flap will appear anemic. Signs of discoloration indicate gangrene, which is difficult to overcome. In a short time the skin takes on a pale pink color, which indicates a reëstablishment of circulation, and granulations begin to show themselves on the reverse side, which, as they[51] multiply, soon thicken the flap sufficiently for the purpose desired.
The dressings are continued, as begun, if there be no indication for interference, although the granulations may be stimulated if too inactive. Gently irritating the granular surface with a 1-3,000 sublimate solution, although rarely permitted by most surgeons, does no harm; in fact, it is to be recommended before reapplying the dry dressing.
In removing the dressings the edges of the flap will be found to adhere to the gauze; this may be gently lifted with the tenaculum, after previous softening with a weak solution of hydrogen peroxid.
Pus (laudable) is the natural secretion from these flaps. Whatever remains on the surface is easily removed by an antiseptic solution, whereupon the powder is again dusted upon the part. When the flap has thickened sufficiently it may be covered by skin grafts, but this is rarely done until it has been properly implanted into the area for which it was intended and only then when union between its sutured borders has taken place. Ofttimes one part of a flap is left unattached, as, for instance, the outer border of the ear, with the object of developing a greater thickness. This must be cauterized along the edge with the caustic pencil, keeping the granulations within the desired limit until the opposite layer of skin has either cicatrized with it or has been grafted near it for the same purpose. The surface is then antiseptically treated, as any granulating surface, except as otherwise indicated.
Foreign Bodies.—Especial care must be exercised with wounds into which foreign bodies have been implanted. Under favorable conditions many are kindly received by the tissues, but often these rebel and even with the greatest of care in dressing such wounds will often result in the necessity for removal of the substance. Individual cases of such nature are fully referred to later.
Symptoms.—After operations performed under the most thorough aseptic or antiseptic procedure, wound fever, more or less marked, may be expected. It develops a few hours after operation and subsides in twenty-four or forty-eight hours. If, however, the wound has not been properly rendered aseptic, or in which there is reason for irritation or tension, more serious symptoms may develop about the second or third day. These symptoms increase with the amount of infection in the wound and result in septicemia, or septic intoxication, the outcome of the absorption of ptomains—the product of tissue decomposition.
Inflammatory fever is marked by a sudden rise in temperature, 100° to 103° F., with a full, strong, and rapid pulse, headache, anorexia, coated tongue, constipation and diminished secretion. If the infection is severe delirium comes on.
If the symptoms are not relieved promptly the indications of septicemia assert themselves with an increasing temperature, between 102° and 104° F., with a rapid compressible pulse gradually becoming weaker. The respirations are rapid and shallow. The tongue becomes dry and discolored and the teeth are covered with sordes.
The restlessness disappears and apathy, somnolence, and a low type of delirium takes its place. Vomiting occurs.[53] There may be a profuse diarrhea and the urine is passed involuntarily. In other words, septicemia is but an aggravated continuance of inflammatory fever; untoward symptoms may come on early, and death may result within forty-eight hours.
On inspection, the infected wound appears highly inflamed, there is increasing swelling, with more or less pain in the part. The edges of the wound appear pale and everted. Serous oozing comes from the wound. If sloughing is to occur from tension or low vitality of the parts the area becomes discolored, assuming at first a pale green color, which turns into bluish brown—and, lastly, brown.
Treatment.—The treatment of such wounds is to immediately relieve all tension by withdrawing the sutures. Flush the wound with peroxid solution and irrigate thoroughly with a 1-3,000 bichlorid solution, leaving the wound open for a free drainage.
Then apply iodoform gauze over the wound and change the dressings as often as is deemed necessary—two or three times a day. In severe cases open the wound thoroughly, even by further incision, clean out the contents of the wound, such as foreign matter, bloodclots, exudate, or perhaps pieces of bone that may have been overlooked, using a small, sharp spoon curette for the purpose. See that the deeper recesses of the wound, especially in those about the nasal bones, are thoroughly gone over.
Next irrigate the wound with a 1-1,000 bichlorid solution. Carbolic solutions to be of use in the severer cases, are too irritating and cause an increase of the secretions, hence they are not to be used. Furthermore, their toxic property is not desirable and ofttimes are not well borne by the patient.
The wound is now loosely filled (not packed) with iodoform gauze to permit of perfect drainage. Aseptic absorbent cotton may be placed over this.
It is not advisable to bring the edges of the wound together; the main object is to overcome the spread of infection and the toxic absorption of the wound product.
When the symptoms are severe moist dressings, in the form of compresses dipped into 1-3,000 bichlorid, are to be preferred, changing them every hour.
Internally it becomes necessary to reduce the temperature and to overcome the toxemia.
For the temperature quinin is the best agent. In milder cases it can be given in tonic doses, associated with antifebrin, with or without morphin, to quiet the patient. In severe forms quinin must be pushed, giving as much as twenty grains at a dose, to be repeated as necessary. A saline purge, magnesium sulphate in full doses, is useful to eliminate the ptomains.
The strength of the patient must be supported by the free use of stimulants and frequent small quantities of nutritious food. Milk with whisky is excellent. Peptonoids and beef juice are given several times in the day.
Favorable symptoms are heralded by the lowering of the temperature, the abatement of toxic symptoms, the reduction of the edema, and the deep redness, as well as the softening of the hard and painful edematous walls of the wound, followed by the breaking down of more or less tissue with the production of pus.
Gangrene in these cases is often due to undue bruising or pressure on the parts during operation, and otherwise to the tension of sutures. It is best to allow the gangrenous mass to remain, keeping it aseptic by antiseptic measures, as it is often found that only the superficial layer and the edge or edges of the wound have suffered.
As demarcation is well established the gangrenous portions may be removed with the dressing or small seizing[55] forceps. Walcher’s pattern of a dressing forceps is shown in Fig. 25, a toothed seizing forceps being represented in Fig. 26.

Fig. 25.—Walcher Dressing Forceps.

Fig. 26.—Toothed Seizing Forceps.
The wound from now on may be at first subjected to a rather strong aqueous solution of hydrogen peroxid, fifty per cent, followed by the same sublimate solution used throughout.
Iodoform gauze dressing, with or without dusting of iodoform or iodol, is continued with the purpose of draining the pus secretion thrown off by the granulating tissue which soon begins to fill the wound, as well as to exert its antiseptic and stimulating influence upon the granulations.
Lazy or glassy granulations are removed with the curette as they appear, or a cauterant, in the form of a nitrate-of-silver stick. Gradually the new tissue contracts, the epidermal edges begin to fold over the surface.
Dry dressing, in the form of aristol or boric acid, may then be used, to produce ultimate healing under an aseptic scab, or lint moistened with two-per-cent salicylic oil or boric vaselin is placed upon the wound. A formula of the latter is made up as follows:
| Boric acid | 3 | parts |
| Vaselin | 5 | ” |
| Paraffin | 10 | ” |
A desirable boric-acid oil for the same purpose is composed of:
| Boric acid | 3 | parts |
| Cera alba | 4 | ” |
| Ol. oliva | 20 | ” |
The latter must be changed daily until cicatrization has been established.
If it is more desirable to cover the granulating area by means of skin grafts it may be accomplished readily, as later described. This is usually resorted to when there has been loss of tissue from the result of sloughing, although a sliding-flap operation may overcome the defect to a nicety; this is especially true of wounds about the anterior nasal border.
If the resulting cicatrice is no larger than the gaping wound it may be excised, the skin at either side is undermined and the edges are brought together, as was originally intended.
It sometimes happens that a wound takes on erysipelatous infection. It is usually of the simple variety, although the cellulo-cutaneous variety is not rare.
Causes.—The predisposing causes are septic infection, lowered vitality, resulting from alcoholism, poor hygiene, and nephritis. The exciting cause has been accredited to the erysipelo-coccus of Fehleisen, which is found chiefly in the more superficial channels of the corium and appearing in chain groups as seen microscopically.
Symptoms.—The symptoms locally are the peculiar rosy rash, rapidly spreading out from the wound with well-defined margins. The affected part appears smooth and edematous and is slightly raised above the surface, the patient complains of stiffness and burning pain in the part. Often vesicles form on the affected part.
The temperature rises suddenly to 102° to 103° F., there is nausea and vomiting.
Treatment.—The wound in such cases must be treated as described in inflammatory fever. Internally the usual remedies are given. A local application of sixty-per-cent ichthyol ointment, covered with salicylated cotton, serves best. The skin may be incised in various places, washed with an antiseptic (sublimate solution 1-1,000) and the serous exudation pressed out with the sterilized hand, after which the above ointment is applied under absorbent cotton (Glück).
Antithermic remedies, as obtained by the application of certain alkaloids, such as cocain, spartein, solanin, helleborin, have been successfully used by Guimard and Geley.
Spartein is especially claimed to exert a happy influence.
Lately a product under the name of antiphlogistin has been used locally with excellent results and its use is to be commended even in local wound inflammation.
If the subcutaneous tissue is affected and the surface indicates the breaking down of tissue, hot antiseptic applications are advisable or the skin is incised down to the deep fascia at such places and iodoform gauze is packed into the wound for several hours. Constant antiseptic irrigation is then established by means of drainage tubes inserted into the various incised places, which are connected to an irrigating apparatus, so that the antiseptic may reach all parts of the infected area.
Nontoxic solutions are indicated in this event; of these, hydrogen dioxid, three per cent, and boric acid, nine per cent, are most suitable. The solution is allowed to trickle gently through the wound and is led off by open tubes, that may be connected in such way as to empty into a receptacle placed beneath the bed.
Anesthesia of the human may be accomplished in two ways: first, by the employment of a general anesthetic, and, secondly, by the local use of a narcotic agent.
It is not the intention of the writer to dilate upon the nature and use of anesthetics, as their value and indication has been fully exploited. A concise review of these agents, however, will meet with the approval of the special surgeon, inasmuch as they have their particular use in individual cases. Local anesthesia is undoubtedly the most extensively employed, in the performance of the average plastic operation, yet in certain cases it is contra-indicated, and it is to further the proper selection of such that the following may be of value.
It must be understood that general anesthesia has its many advantages and equally its disadvantages. It necessitates the early preparation of the patient and a thorough physical examination as to the state of lungs, heart, and kidneys. Patients having cardiac affections or serious lesions within the lungs should be given the safest anesthetic obtainable; in fact, if the operation can possibly be done by local administration, it should be.
It is to be remembered that in a majority of these cases the operation is undertaken to remedy a deformity, however caused, one that is not necessarily serious to health, and it would indeed be unwise to place such a[59] body in jeopardy or to take undue chances if they can be avoided. Ofttimes several operations, a few weeks apart, must be done and the frequent repetition of a general anesthetic might impair the health of the patient—a condition not associated with local anesthesia.
Neurotic subjects often insist upon the use of chloroform and the surgeon is frequently tempted to administer it, but little objection should be found with local narcosis, where it can be employed.
The patient must not be allowed food at least six hours prior to operation. In neurotic and anemic subjects a full dose of strong wine or whisky should be given half an hour before operation. Habitual drinkers should be given one quarter grain morphin sulphate. All movable artificial teeth, or other foreign bodies, must be removed from the mouth. Observe the laws of asepsis as heretofore described. Loosen the clothing of the patient about the neck and chest. Only a single garment should be worn during the time of operation—a loose, sterilized night robe, as it may be necessary to move the patient about, and too much or tight clothing might prove to be dangerous in the delay occasioned by its removal.
The operating room should never be cold enough to chill a patient so prepared. Hot-water bottles or a warm pack can be placed between or about the limbs to equalize the external circulation. This is especially necessary when chloroform is administered, as this lowers the temperature of the body. Have the bowels and bladder emptied. Choose the early part of the day for operations of some length, because the stomach is then empty and vomiting with resultant gastric disturbance will be lessened or entirely avoided. The anesthetizer should be experienced and attend to his duty implicitly. He must at all times watch the patient, take[60] note of the pulse, pupils, and respiration. Close by he must have a mouth-gag, tongue forceps, long-handled sponge holders, containing dry absorbent cotton sponges, and a basin in case of emesis.
He should quietly instruct the patient how to breathe and at first assure him, and as narcosis comes on command him to do what is necessary. No desultory or detracting conversation should be permitted. A small but efficient faradic apparatus must be within call of the administrator. Sterile vaselin should be smeared about the nose and mouth to prevent skin irritation.
(Guthrie) The pure product must be used. It is a colorless, mobile liquid, having an ethereal odor and sweet to the taste. It should not affect litmus or turn brown with sulphuric acid or give a precipitate with nitrate of silver. If there is emphysema of the lungs, bronchitis, or renal disease, chloroform is to be preferred to ether, also in operations about the oral cavity. Children bear chloroform narcosis better than adults.
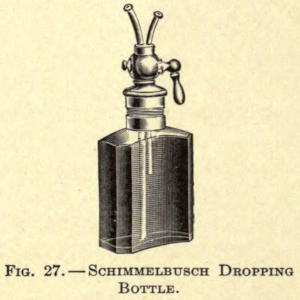
Fig. 27.—Schimmelbusch Dropping Bottle.
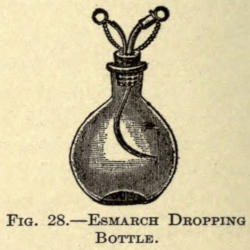
Fig. 28.—Esmarch Dropping Bottle.
Chloroform first affects the brain, then the sensory tract of the spinal cord, then the motor tract, followed by an involvement of the sensory path of the medulla, paralyzing the respiratory centers, while cardiac syncope[61] may come on at any time during narcosis. Death may be either due to respiratory or cardiac failure, often from both. To overcome this the anesthetic should not be crowded, nor should the apparatus be held too close to the mouth of the patient. The best method of giving it is by means of the dropping bottle of Schimmelbusch (Fig. 27) or that of Esmarch (Fig. 28) and a simple mask or apparatus.
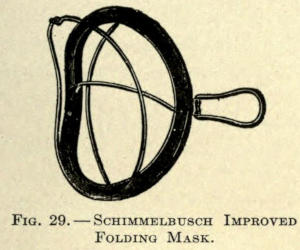
Fig. 29.—Schimmelbusch Improved Folding Mask.
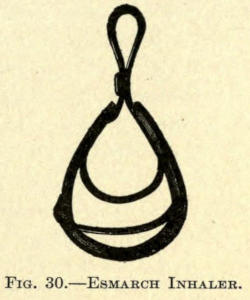
Fig. 30.—Esmarch Inhaler.
The wire frame affair, to be covered with a fold of muslin, designed by Schimmelbusch, is perhaps the best (Fig. 29). Another splendid inhaler is that of the Leiter improvement of the Esmarch folding frame (Fig. 30).
A folded towel, crumpled or pinned into a hollow oval form, may be substituted for the above.
Begin by pouring about thirty drops upon the inhaler, gradually bringing it nearer from a distance of six inches to the mouth and nostrils of the patient; then continue by letting one drop fall upon the apparatus every five or ten seconds until the patient is thoroughly anesthetized; then use one drop about every ten seconds, although it might be necessary to push this quantity at certain moments of the operation. To obtain complete anesthesia by this method takes about ten minutes. The vapor should be thoroughly mixed with air in the proportion of ninety-five per cent of air to five per cent of the[62] vapor. The amount administered during operation can rarely be determined, because of the uneven respiration of the patient, who takes more during frequent inspiration than during ordinary breathing. By all means do not let the chloroform trickle upon the skin or into the eyes, as it causes considerable irritation.
The respirations are at first full and deep, soon becoming shallow and rapid. At first the pulse is slightly stronger and fuller than the normal, but it soon loses its strength and volume and becomes more rapid. The pupils are at first dilated, and as narcosis is induced, contract. Should they contract after this, during operation, it is a danger signal not to be neglected. Death may come on suddenly.
If the patient struggles violently under early anesthesia, as is often seen in alcoholics and athletes, it is not advisable to push the chloroform nor should total muscular relaxation be effected. The arrest of reflex movement is all that is required.
As the reflex action of the cornea disappears last of all, the anesthetizer can use this as a guide during further administration to avoid all danger. This is accomplished by gently touching the cornea with the index finger, raising the eyelid with the third finger.
Chloroform lowers the body temperature, due undoubtedly to its aiding in the dissipation of heat and by reason of its effect on the nervous mechanism of heat production. It is rapidly eliminated by both the lungs and the kidneys, because of its high volatility, and as little is given, the irritation to these organs is not as great, volume for volume, as with ether.
In case of asphyxia the lower jaw must be pushed far forward, the tongue be drawn forward with forceps, and the head extended and lowered, by raising the feet off the table. Cold water should be dashed over the face and chest. Slapping the chest with a wet towel and vigorously rubbing with hot cloths or brushing the palms and[63] soles. Brandy and water, one to two parts, can be introduced into the rectum, or faradization of the nasal mucous membrane can be tried. These means failing, artificial respiration (Sylvester’s method) must be resorted to. This being of no avail, tracheotomy must be done.
If the patient is induced to vomit, he should immediately be turned on his side to prevent the indrawing of the ejected matter into the lungs. After it has ceased, thoroughly wipe out the mouth with a long-handled sponge. The anesthetic must now be crowded slightly to overcome the irritation of the mucous membrane of the stomach. Often during the early stage of anesthesia the patient stops breathing, which must be overcome by slapping the chest or by two or three forceful downward movements on the epigastrium.
If the face of the patient takes on a sudden change of color or breathes heavily the anesthetic should be withdrawn for a few moments, until the symptoms abate. If the mucus collects about the glottis it is liable to cause respiratory difficulty and must be swabbed out. If the inversion of the patient does not relieve syncope and the methods already mentioned fail to relieve, injections of normal salt solution into the median basilic vein must be employed as a last means.
(Jackson, Morton.) Sulphuric ether is used in the pure form, free from alcohol and water. It should be a colorless, volatile, mobile, and highly inflammable liquid, having a peculiar penetrating odor. As its vapor is much heavier than air, and owing to its combustible nature, lights about the room should always be placed above the patient. Often its vapor is ignited by the careless use of the electro-cautery.
Ether for anesthesia should not affect blue litmus. It should not give a blue color to ignited copper sulphate—the[64] test for the presence of water. Alcohol is indicated when it turns red by adding fuchsin.
Ether is less toxic than chloroform, therefore it requires a greater quantity to induce narcosis.
If properly administered it is by far safer than chloroform, Ollier, of Lyons, reporting only one fatality directly due to its employment in four thousand patients. If the anesthetic is crowded cyanosis with jugular pulsation is noted—the signs of inefficient oxygen and cardiac distention. In most recorded cases of death there were complications of a nephritic pulmonary nature. Ether should not be used where there is bronchitis, gastritis, or peritonitis, owing to its irritant effect on mucous membranes, nor in nephritis, aneurysm, or advanced atheroma. The movements of the diaphragm must be constantly watched as it is the first to become paralyzed when anesthesia is carried too far. The same care must be observed with the pupil for cerebral and the pulse for cardiac signs. Before giving this anesthetic the same preparations as for chloroform narcosis should be observed. The stomach should be empty, the nose and mouth smeared with vaselin, and the eyes protected with a towel.
At first the patient is given the ether with a considerable mixture of air, which should be lessened gradually. Coughing comes on quite often, which is overcome by increasing the ether. Soon there comes a state of respiratory forgetfulness. This is caused by the irritation of the trigeminal and vagal nerves (Hare). This is corrected by dashing ether upon the epigastrium or by sudden and repeated pressure at this point. There is also choking and struggling, the face becoming suffused and red and there is an injection of the conjunctiva. As the ether is pushed the patient becomes quiet, followed by a second seizure of struggling, so intense, that force must often be employed to hold him on the table. With this there are the various attacks of laughing, crying,[65] singing, or yelling—a semiconscious exhibition of the state of the mind of the individual.
As anesthesia progresses relaxation takes place and the time for operation is at hand. Often the throat fills with mucus, owing to the irritant effect of the vapor on the mucous membranes. This must be wiped out with the sponges.
If vomiting occurs the head of the patient is turned to one side until relieved. The mouth should be cleansed thoroughly thereafter to prevent the contents getting into the lungs and causing bronchial irritation and often broncho-pneumonia. If the patient gets too little air, shown by laryngeal stertor, frequent and feeble pulse, livid face or pallor, tonic spasm, thoracic breathing with fixed diaphragm, and drawing in of the abdominal walls with inspiration, the ether should be let up and the jaw pushed forward by placing the fingers under the rami. The tongue should be drawn forward, as already described, and such methods be used as have been mentioned in connection with asphyxia in chloroform narcosis. The pupils fixed in dilatation is indicative of immediate danger.
Strychnin and digitalis should be given hypodermically or the intravenous use of ammonia may be employed. If the stertorous breathing is due to mechanical causes, not to too much ether, the hypodermic use of ether will bring about reflex respiratory movement by reason of the local pain and irritation thus produced.
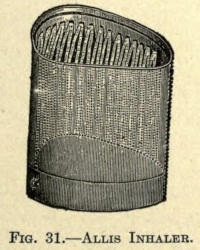
Fig. 31.—Allis Inhaler.
Fig. 32.—Fowler Inhaler.
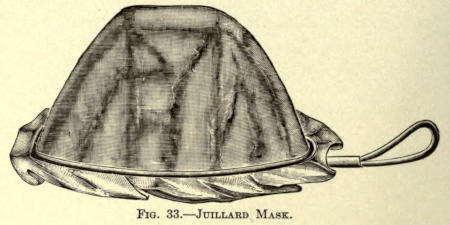
Fig. 33.—Juillard Mask.
The anesthetic may be administered with the aid of various masks or inhalers. Simplicity of construction is to be preferred to more complicated apparatuses. The aseptic metal inhaler of Allis (Fig. 31) or the folding form of the same modified by Fowler (Fig. 32), are much used in the United States, while the Juillard mask—a metal frame covered with several thicknesses of gauze—is used abroad. (See Fig. 33.)
It is to be remembered that in operations about the face ether anesthesia is not practicable, owing to the repeated lifting of the mask which allows the patient too much air. It can only be given by specially constructed inhaling devices, which are more easily used with chloroform or the mixed anesthetics. Their specific use and construction will be referred to later.
It is often desirable to get the patient as quickly as possible under anesthesia and still overcome the depleting effects of chloroform narcosis. A common method to accomplish this is to give chloroform to the point of relaxation and with a change of inhaler continue with ether. In this way anesthesia can be kept up safely a long time with a minimum amount of ether. There are, however, a number of mixtures used in place of this interchange[67] of anesthesia, all having their particular merit. Some of the best known are:
Alcohol-Chloroform-Ether (A. C. E. Mixture, English Formula, 1:2:3).—This induces rapid anesthesia without the danger of syncope or the other objections to chloroform or ether when used alone.
Chloroform-Ether-Alcohol, in the proportion of 3:1:1, and known as Billroth’s mixture, is extensively used in the same way.
Chloroform-Ether.—This mixture, in equal proportions, is known as Tillman’s mixture, and has been employed by many well-known surgeons.
Nitrous oxid, as advocated by Sir Humphrey Davy, is a safe product, but the anesthesia produced thereby is of too short duration to be of practical value in plastic surgery. Its employment is resorted to only for such operations as the opening of abscesses or the removal of small cysts, etc.
While ethyl bromid is a product that cannot be said to be absolutely safe, Terrier, of Paris, has used it largely to induce anesthesia, following it up with chloroform. It should be given freely with deep inspiration, the sixth inhalation producing total loss of consciousness. A moment after complete muscular relaxation is attained, with congestion of the face and dilated pupil. The average time necessary to accomplish this is about one minute, in which about three to five grams are used. In this way the stage of excitement is overcome and immediate narcosis is obtained. As the chloroform is substituted it must be given fairly strong, reducing it gradually. The facial congestion slowly diminishes and the pupillary dilation gives way to contraction. About sixteen[68] grams of chloroform are required to keep up anesthesia for fifteen minutes. The after-effects of chloroform are entirely overcome by the above method.
Hawley, in reviewing the use of ethyl chlorid as a general anesthetic in minor operations, states that after several years of more or less constant use of ethyl chlorid, both in clinical and private practice, he has still to see the first case in which it has caused him the slightest uneasiness. The following precautions in its administration should be observed: (1) The patient should be prepared as for chloroform or ether; (2) whatever mask is used, it should fit the face snugly; (3) a graduated tube with a large aperture should be used; (4) the anesthetic should be well supplied with air and as little given as possible; (5) care should be taken not to present it at first in too large a quantity; frequently a dram is quite sufficient for short operations; (6) the patient should rest a while after its administration, as faintness sometimes supervenes; (7) a mask should be used which does not receive the drug close to the patient’s face, otherwise one is liable to either freeze the face of the patient or to cause asphyxia by the moisture from the expired air freezing on the gauze in the mask, and thus preventing the free passage of air to the patient.
The use of ethyl chlorid has the following advantages: (1) Safety in administering; (2) ease of administration; (3) it rapidly produces surgical anesthesia; (4) it can be used where chloroform or ether would be contra-indicated; (5) the patient can be kept in any position during anesthesia, upright or prone; (6) no cyanosis need occur during administration; (7) the patient recovers promptly without after-effects; (8) it is inexpensive; (9) it can be used for a long or short operation with equal success; (10) it is especially useful as a preliminary[69] to other anesthetics, decreasing the time required for the production of anesthesia and avoiding shock and discomfort to the patient.
Ethyl chlorid is a colorless, mobile liquid, which boils at 52° F. This is furnished in thirty- and sixty-gram glass tubes, sealed with a metal screw cap or spraying device. As this cap is removed the liquid in the tube begins to boil, owing to the temperature of the room, or, better, the operator’s hand, and a fine vapor spray is ejected from the opening.
The tube end is held from six to eight inches from the part to be anesthetized. Immediately the skin is frosted over and the lanugo hairs become covered with snow. The skin turns white and becomes slightly elevated, appearing to be thickened; at the same time the patient feels a stinging pain in the area. This may be overcome greatly by first smearing the part with sterile vaselin. In a few moments the skin is frozen and rendered antalgic, and operations of short duration can be performed. The only disadvantage with this method is that the part to be operated on is frozen stiff, hence the skin cannot be neatly dissected away from the subcutaneous tissue as under other local anesthesia, nor can the tissues be moved about as readily, as in the case with flap operations, owing to this stiffness.
The parts thaw out quickly with a returning sensitiveness, and it may be necessary to apply the spray repeatedly until the operation has been completed. If elastic constriction can be employed, the antalgic effect is more quickly produced and more lasting.
As the parts thaw out there is considerable prickling, which can be mitigated by applying sponges soaked in[70] hot sterilized water. More or less redness of the skin will be noted even for some time after the operation.
(Methylbenzoylecgonin)
(Gädeke, Nieman, Bennett, Koller.) Cocain is the alkaloid derived from several varieties of Erythroxylon coca. It should appear as a permanent white crystalline powder in colorless prisms or flaky leaflets. The salt used for anesthetic purposes is the hydrochlorid; it is soluble in 0.4 part water, 2.6 parts alcohol, 18.5 parts of chloroform, and insoluble in ether.
Locally applied on mucous membranes and open wounds, it exerts an analgesic effect, but not of the unbroken skin. Punctures or abrasions are necessary to permit of absorption in this event. When locally applied it paralyzes the peripheral sensory nerves, and at first blanches the parts by reason of its active contraction on the arterioles, which is soon followed by marked congestion.
Krymoff has made extensive experiments to determine the anesthetic effects of cocain solutions sterilized in various ways. He claims that the best results in minor surgery are obtained with the one-per-cent solution pasteurized at 60° C. for three hours. The same solution pasteurized at 80° C. for two hours or at 120° C. for fifteen minutes gave results far less satisfactory.
While the pasteurized solutions accomplished an anesthesia lasting from one to two hours, sterilized solutions (boiled at 100° C.) overcame pain only for a period between twenty and thirty minutes.
Pasteurized solutions have the advantage of being sterile and do not decompose as the boiled solutions would. The pasteurization is accomplished as follows: The necessary amount of cocain is dissolved in sterilized water. The solution is put into a sterilized glass bulb,[71] which is sealed hermetically and subjected to a temperature of 60° C. for three hours.
Since cocain is a nerve poison, its systemic absorption must be avoided. The constitutional effects of a given amount injected about the head, face, and neck are more marked than when injected in other parts of the body or extremities. This is due to two causes: a more rapid absorption and the proximity to the brain (Ricketts). For this reason less cocain should be used and the blood vessels be avoided.
Idiosyncrasy influences greatly these toxic effects. In neurotic patients of irritable and impressionable type the hypodermic use of this agent has especially induced serious syncope. Very serious symptoms and even death have been caused by its local use (⅛ grain hypodermically).
Untoward effects are manifested by nausea, vertigo, emesis, syncope, followed by clonic convulsions, delirium, and death.
Cocain first stimulates, then paralyzes, the pneumogastric nerve; the respiration is first accelerated, and then paralyzed, death being due to failure of respiration.
Should these symptoms occur, the patient should be placed on his back with the head low. Amyl nitrate inhalations act as the antidote and reduce the cerebral anemia (Feinberg). Morphin or caffein is to be given hypodermically, or the former is associated with potassium bromid internally.
To overcome the toxic qualities of the anesthetic it may be combined with morphin in solution, Schleich’s solution being well known. It is composed as follows:
| Cocain murias | 0.1 |
| Morph. sulph. | 0.025 |
| Sodium chlor. | 0.2 |
| Aquæ sterilis. | 100.0 |
Gauthier suggests the addition of one drop of a one-per-cent solution of nitroglycerin to the quantity injected and repeated to prevent the unfavorable after effects.
Solutions of cocain are to be made up fresh each day, as they become moldy on standing. They cannot be sterilized, for the reason that a temperature of 213° F. renders them useless. The solution is most active at 50° F. (Costa).
For hypodermic purposes two- to ten-per-cent solutions are employed, the four per cent being more generally used, not more than 0.1 gram of the agent being introduced (Hänel, ano).

Fig. 34.—Simplex Syringe.
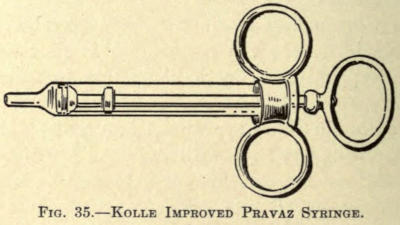
Fig. 35.—Kolle Improved Pravaz Syringe.
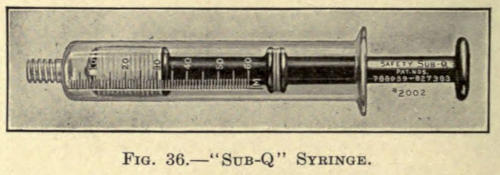
Fig. 36.—“Sub-Q” Syringe.
For the introduction of the solution the ordinary Pravaz syringe can be used, a modification of which being known as the “Simplex” (Fig. 34). It is a glass instrument, without screw threads within the needle base, and has a sterilizable fiber piston. The only disadvantage offered by this syringe is the lack of finger rests. The author has added a removable nickel-plated sleeve with[73] finger rings to slip over the glass barrel, as shown in Fig. 35. The advantage of this modification will be appreciated when injections are made into dense or cicatricial tissue where considerable pressure is necessary for the introduction of the solution.
Another excellent syringe for the purpose is the metal-cased instrument known as the “Sub-Q” (Fig. 36); the barrel and piston in this are of glass, an asbestos packing being wound over the piston head.
Metal needles with large thread or smooth ends are employed. As the asbestos packing contracts in drying, the piston should be removed from the barrel and cleansed immediately after use, and not be introduced into the barrel until both the asbestos windings and the inside of the barrel have been moistened with warm sterile water. This precaution prevents the cracking of the instrument through undue pressure exerted on the end of the piston rod at the time of use.
To render the primary introduction of the needle painless the area might be sprayed for a moment with ethyl chlorid. After carefully preparing the site of operation, the subcutaneous injections are made in a somewhat oval or circular manner, the first infiltration of the cocain rendering the succeeding points analgesic.
It will be noted that the skin becomes whitened and is raised in little tumors, with the point of puncture as a center. The various punctures are so placed that the borders of these tumors meet, the entire site becoming edematous. If by constriction the part can be rendered ischemic, the analgesic effect is prolonged, reducing the systemic absorption to a minimum.
The subsequent nausea often following may be promptly overcome by the use of a mixture of creosote, four drops in limewater. For mucous surfaces the anesthetic may be applied with absorbent cotton and allowed to remain about five minutes. In deeper wounds than those involving skin, deeper injections must be made.
The effect of the anesthetic as above employed is practically immediate, and the operation can proceed at once. Its duration is from fifteen to twenty minutes for subcutaneous surgery, but where the deeper structures are involved subsequent injections must be made to control the pain.
(Benzoylvinyldiacetonalkamin)
(Merling, Vinci.) White powder, soluble in 33 parts of water. While the effects of eucain are immediate and produce anesthesia as thoroughly as cocain, it has the objection of producing local hyperemia and increased edema of the parts injected. This often interferes with the successful outcome of the first operation, as will be later shown. The advantage over cocain, however, is that a solution of eucain can be sterilized by boiling without reducing its usefulness, which in itself is an item, since both are expensive, and if we must prepare a cocain solution fresh for each day we must discard all that has not been used, while with eucain the same preparation can be safely used over and over, after proper sterilization.
The two- and three-per-cent solutions are most employed to the extent of from 10 to 60 minims. Its subcutaneous effect is immediate, lasting from ten to twenty-five minutes. When applied locally to mucous membranes, the five-per-cent solutions are used.
Principally it may be said that eucain does not exhibit the toxic properties of cocain, the author having employed it in over 5,000 cases with no untoward effect.
Liquid air is suggested as a means of local anesthesia by A. C. White. He recommends its intermittent application instead of freezing the part as with ethyl[75] chlorid. It is sprayed on the parts and produces immediately anemia and insensitiveness. There is no hemorrhage during its use, so that dressings may be applied before the parts assume their circulatory function; an advantage of considerable value in plastic surgery. No untoward results follow its use.
(Benzoyl-ethyl-dimethylamin-opropanol hydrochlorid)
(Fourneau.) This is the latest preparation advocated for local anesthesia. It is a synthetic product, derived from tertiary amyl alcohol. It is less toxic than cocain, and has been used more or less in the past years experimentally, but the consensus of opinion seems to be against its use. Jennesco has used it extensively in conjunction with strychnin in spinal anesthesia, but the surgeon in general has not taken kindly to it. In plastic surgery, as used locally, it has been little employed, eucain being the most serviceable for the purpose.
Plastic surgery is resorted to in covering defects of the skin due to congenital or traumatic malformation, injuries, burns, the removal of neoplasms, or the ulcerative processes of disease. Furthermore, it can be employed cosmetically for the rebuilding of organs, whole or in part, or for their reduction when abnormally developed. This applies particularly to the nose, ears, and lips, wherein it may involve either the skin alone or the mucous membranes, or all the tissue making up the parts operated on.
Incisions.—The incisions in plastic surgery are to be made obliquely into the skin rather than at right angles to the surface, the former permitting of better apposition, and undoubtedly causing less epidermal scar. The incisions include the skin only, except when otherwise stated.
Sutures.—Sutures should be placed not more than ¼ of an inch apart and be made to include the skin only, unless it is deemed advisable to employ deeper ones to relieve undue traction, which often results in suture scars and ofttimes tissue loss, necessitating further operation. The latter may be obviated by placing every other stitch at greater distance from the free edge of the skin, that is, into the undissected border.
Intracutaneous sutures may also be employed, but these are rarely, if ever, necessary if the apposition has been properly accomplished. To relieve tension, harelip[77] pins are also used, as later described. Catgut of such size as would be suitable because of its ready absorption is not to be employed for skin suturing, fine twisted silk or selected horsehair being the best material.
Formaldehyd catgut can be used if it is desirable; its fine strands withstand absorption to a greater degree than the ordinary.
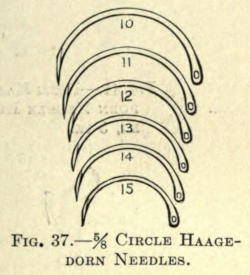
Fig. 37.—⅝ Circle Haagedorn Needles.
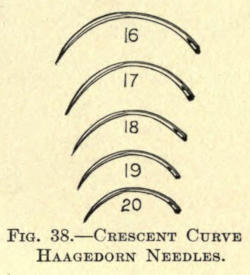
Fig. 38.—Crescent Curve Haagedorn Needles.
Needles.—Very fine, flat, round-eye needles, such as Haagedorn’s, Nos. 12 to 15, ½ or ⅝ circle, are the most serviceable in skin work, as they incise the skin in penetrating and leave an elongated slit, which heals readily, rarely leaving a needle scar. The selection of needles, however, must be left to the operator, many preferring the one variety to the other. Split-eye needles are quite convenient, but they break more readily, and while they work best with fine silk, this is more readily withdrawn from the eye at undesirable times. For very delicate work the needles mentioned are the best.
Needle Holders.—Inasmuch as the needles used in plastic operations are very small and fine, proper needle holders must be used. The requisitions are that the jaw be long, narrow, of soft copper, and that they have an automatic lock attachment. Plain needle holders may be used, but at times the locking device is very necessary and saves time. The most serviceable of this class are the Kersten modification of Mathieu, an uncomplicated holder of merit (Fig. 39), and the small Haagedorn, five-inch narrow-jaw holder (Fig. 40), or the holders taking similar needles, as shown in Figs. 41 and 42, known as Pozzi’s and Weber’s modifications, respectively.
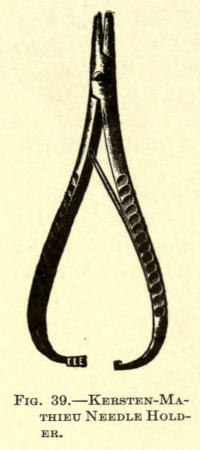
Fig. 39.—Kersten-Mathieu Needle Holder.

Fig. 40.—Haagedorn Needle Holder.
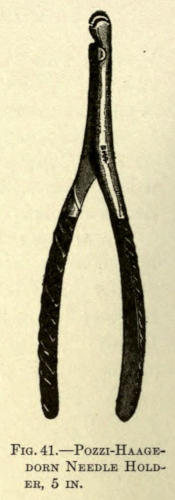
Fig. 41.—Pozzi-Haagedorn Needle Holder, 5 in.
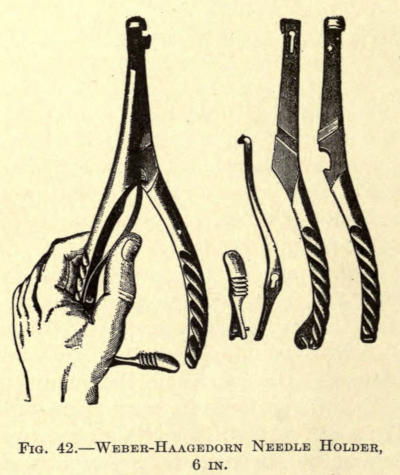
Fig. 42.—Weber-Haagedorn Needle Holder, 6 in.
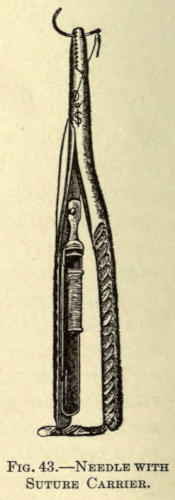
Fig. 43.—Needle with Suture Carrier.
Holders with cup jaws serrated at different angles are of no value, unless other needles are used with them, as they invariably break the flat ones.
To overcome the necessity of rethreading or the use of many needles, the very ingenious holder with ligature carrier can be used, especially where the surgeon does not care to sew with a long, free thread. The silk can be sterilized on the metal spool separately and inserted within the handle of the holder, as shown in Fig. 43.
There are five distinctive methods employed in performing plastic operations:
I. Stretching of the margins of the skin.
II. Sliding flaps of adjacent skin.
III. Twisting pedunculated flaps.
IV. Implantation of pedunculated flaps by bridging.
V. Transplantation of nonpedunculated flaps or skin grafting.
This classification differs from that heretofore generally given in the meager literature on the subject, but the author believes his arrangement to be more scientifically exact as well as simpler for recording and history purposes.
In the stretching method the defect is neatly excised, so as to freshen the margins to be brought together. It may be necessary, if the defect is too large for free apposition, to dissect the skin away from the underlying tissue to render it more movable and to overcome tension.[80] The shape of the incision depends largely upon the nature of the defect and must be made with a view of leaving as little scar as possible. Where the defect is somewhat linear, or elongated, an elliptical incision (A) is made, as in Fig. 44, and, if necessary because of too great tension, the skin is undermined sufficiently to allow the parts to come together; if this cannot be done readily, two semilunar incisions (b, b) must be added. This will allow of ready coaptation. The wound is then brought together with an interrupted suture, appearing as in Fig. 44a, the semilunar spaces being allowed to heal by granulation.
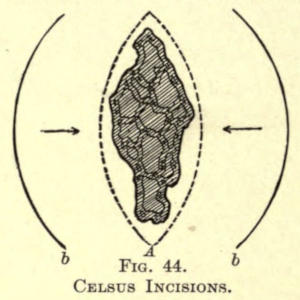
Fig. 44.
Celsus Incisions.
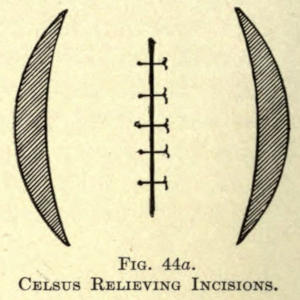
Fig. 44a.
Celsus Relieving Incisions.
In excisions in small rhomboidal form, the skin is merely dissected up and around the wound, the same as in Fig. 45, and the wound is sutured in linear form, as shown in Fig. 46.
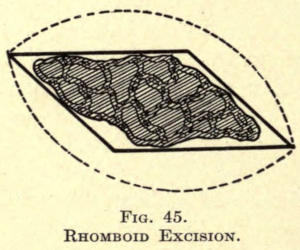
Fig. 45.
Rhomboid Excision.
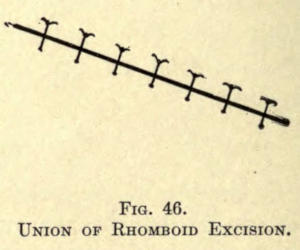
Fig. 46.
Union of Rhomboid Excision.
If the defect is oblong in form, the angles are brought together wholly, leaving a small surface to granulate, as in Fig. 47, or they are drawn toward the center, leaving the remainder of the parallel lines to be sutured, as shown in Fig. 48.
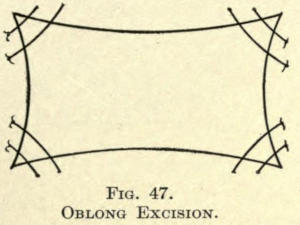
Fig. 47.
Oblong Excision.
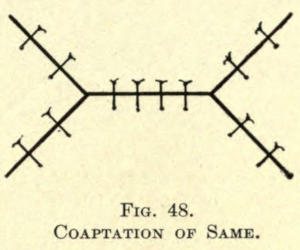
Fig. 48.
Coaptation of Same.
Another method of overcoming a smaller defect of similar form is to excise a small triangular portion of skin at either side of the oblong, as in Fig. 49, and then with or without dissection bringing the margins together in linear form, as in Fig. 50.
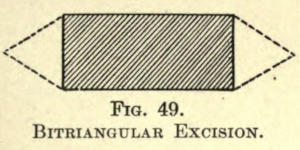
Fig. 49.
Bitriangular Excision.
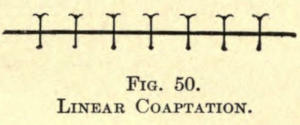
Fig. 50.
Linear Coaptation.
Likewise can a triangular fault be brought together by sewing in the greater angles and making a linear wound of the remaining part, as in Figs. 51 and 52.
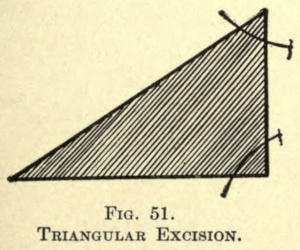
Fig. 51.
Triangular Excision.
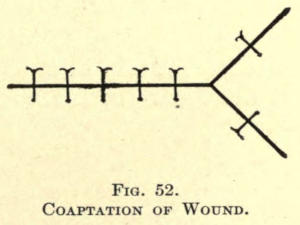
Fig. 52.
Coaptation of Wound.
Again, a triangular defect may be remedied by adding a smaller triangle at each end involving healthy skin, utilizing, if need be, the relieving incisions, as in Figs. 53 and 54.
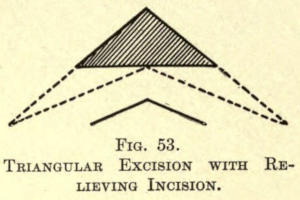
Fig. 53.
Triangular Excision with Relieving Incision.
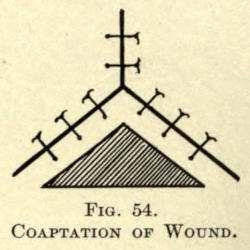
Fig. 54.
Coaptation of Wound.
Following the principle of Celsus, as mentioned on page 8, defects can be overcome in various ways. The incisions may be straight or curved, and one or more flaps of skin are raised, slid, and sutured over the part to be covered. The simplest form is the covering of a square, as shown in Figs. 55 and 56.
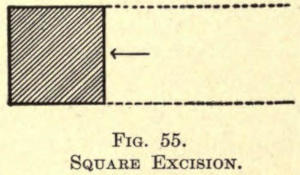
Fig. 55.
Square Excision.
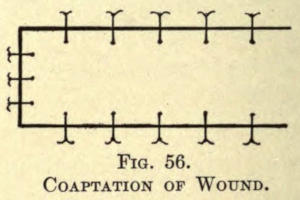
Fig. 56.
Coaptation of Wound.
If the square be too large for the above method, the[83] incisions can be carried to the other side and above or below the defect, as shown in Figs. 57 and 58.
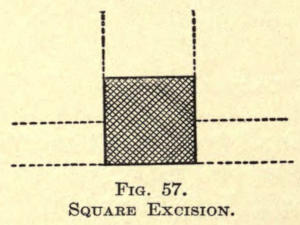
Fig. 57.
Square Excision.
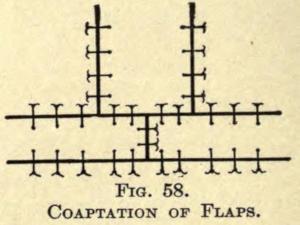
Fig. 58.
Coaptation of Flaps.
For triangular areas the curved incisions can be made, as in Fig. 59, rotating the flap into place, as shown in Fig. 60.
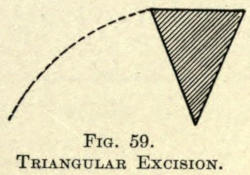
Fig. 59.
Triangular Excision.
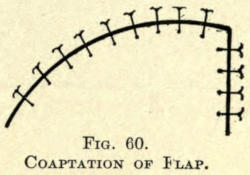
Fig. 60.
Coaptation of Flap.
Or bilateral flaps may be utilized by straight incisions, stretched and sewn, as in Figs. 61 and 62.
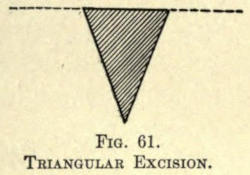
Fig. 61.
Triangular Excision.
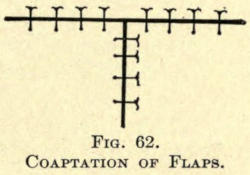
Fig. 62.
Coaptation of Flaps.
Again, two curved incisions are made to obtain rotating flaps, Fig. 63, and sewn, as shown in Fig. 64.
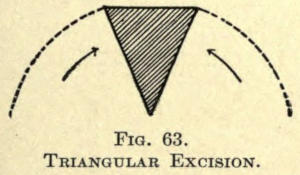
Fig. 63.
Triangular Excision.
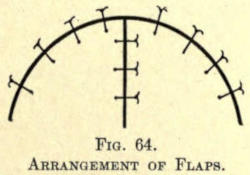
Fig. 64.
Arrangement of Flaps.
Bürow introduced a method for closing over defects by sliding flaps in which he utilized the mobility of skin obtained by the excision of triangles of healthy skin. The results are exceedingly good, but, unfortunately, the sacrifice of skin affects its general use, inasmuch as patients can afford but little loss of healthy skin; besides, there is the objection of added scarring. The closing of[84] a triangular defect by this method is shown in Figs. 65 and 66, in which a is the triangular defect and b the triangle of healthy skin excised. The skin about the incisions is dissected up and the flaps are sutured into position, as shown in Fig. 66.
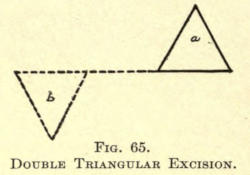
Fig. 65.
Double Triangular Excision.
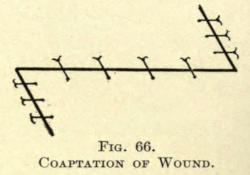
Fig. 66.
Coaptation of Wound.
Where the triangular defect has a wide base, bilateral triangular sections of skin are removed (Fig. 67), and the flaps are coapted, as in Fig. 68.
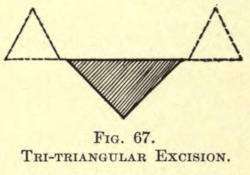
Fig. 67.
Tri-triangular Excision.
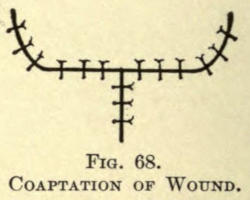
Fig. 68.
Coaptation of Wound.
Through the sacrifice of two triangles a large oblong or square defect may be covered, the excisions being shown in Fig. 69 and the suturing in Fig. 70.
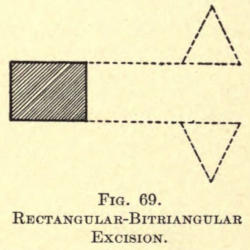
Fig. 69.
Rectangular-Bitriangular Excision.
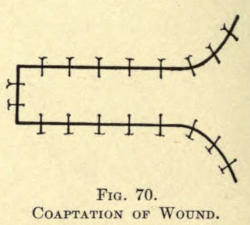
Fig. 70.
Coaptation of Wound.
Although in several of the above methods the flaps are rotated and slightly twisted, the following are only classified with those under this division.
Where an elliptical defect is to be obliterated the curved incision shown in Fig. 71 can be satisfactorily employed, leaving but a small area to granulate over. The suturing is depicted in Fig. 72.
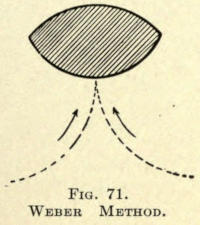
Fig. 71.
Weber Method.
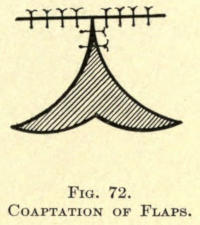
Fig. 72.
Coaptation of Flaps.
In this the twisting of the flaps is but little, while in the following, in which the defect is of similar shape, the twisting is more apparent; so much so, that a fold at the root of the flap may be induced to some extent. The excision and incisions are shown in Fig. 73, and the method of bringing the parts together in Fig. 74, leaving a small area for granulation.
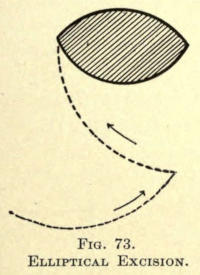
Fig. 73.
Elliptical Excision.
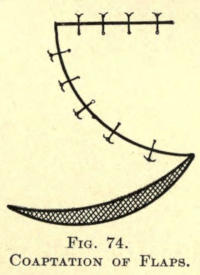
Fig. 74.
Coaptation of Flaps.
Considerable twisting of flaps is shown in covering triangular parts in Figs. 75 and 76.
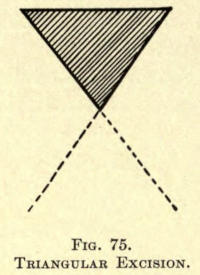
Fig. 75.
Triangular Excision.
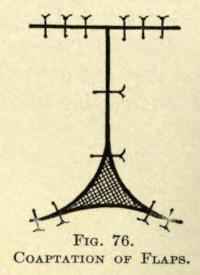
Fig. 76.
Coaptation of Flaps.
In this only a small surface is left to granulate over, while in the following the parts are entirely covered. The excision and incisions are shown in Fig. 77, and the method of approximation and suturing in Fig. 78.
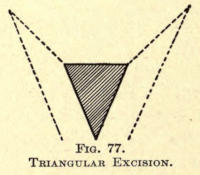
Fig. 77.
Triangular Excision.
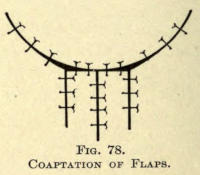
Fig. 78.
Coaptation of Flaps.
In covering a square area considerable twisting must be resorted to, as shown in Figs. 79 and 80, leaving a portion to granulate.
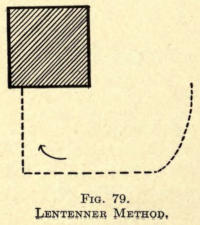
Fig. 79.
Lentenner Method.
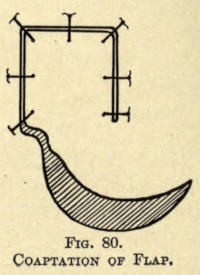
Fig. 80.
Coaptation of Flap.
Where the area is irregular and formed somewhat as in Fig. 81, bilateral incisions are made and the flaps twisted into place and sewn, as in Fig. 82.
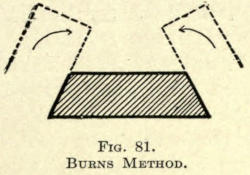
Fig. 81.
Burns Method.
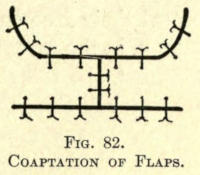
Fig. 82.
Coaptation of Flaps.
In this method the flap to be utilized in covering a defect is taken from a distant part of the body, as, for instance, from the arm. The flap thus taken at first remains attached at its distal end to the tissue of the arm by a pedicle, which is not severed until a circulation has been established between the flap and the part of the human economy to which its free end has been attached by suture, the arm being held in position in the meantime by a suitable contrivance, as shown in Fig. 83.
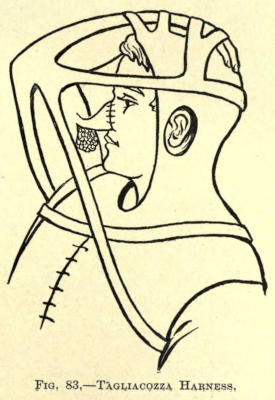
Fig. 83.—Tagliacozza Harness.
These pedunculated flaps, bridging over space, may likewise be taken from the forearm, the hand, or the thoracic region.
When thoracic flaps are used they may be directly sewn at their free ends to the part to be covered, as, for instance, in the forearm or arm, or they are stitched to the forearm to be later transferred to another part of the body after their circulation had become established.
The various methods of the employment of these bridging flaps will be taken up individually in their respective places farther on.
Where there is loss of skin due to injury or operative procedure the parts may heal by granulation, but as this requires much time, and the consequent cicatrice causes considerable deformity, the granulating or freshly made wounds are covered with so-called detached skin flaps or grafts, when the former methods of plastic surgery cannot be followed.
The methods employed in skin-grafting may be classified as: 1, autodermic; 2, heterodermic; 3, zoödermic.
1. Autodermic, when the grafts are taken from the tissue of the patient.
2. Heterodermic, when the grafts for the patient are taken from other persons.
3. Zoödermic, when the grafts for the patient are taken from the lower species.
The former two classes may for convenience be again subdivided into
1. (a) Auto-epidermic.
(b) Autodermic.
2. (c) Hetero-epidermic.
(d) Heterodermic.
The third class will permit of a great many subdivisions, too numerous to mention, each taking its name from the source of the graft.
a. Auto-epidermic Skin-grafting.—The method of covering granulation areas with small circular pieces of detached skin, pin grafts, was first advocated by J. Reverdin in 1870. The Reverdin method is applicable to healthy granulating surfaces only. The small lentil-form skin grafts are obtained from the arm or other suitable part of the body by raising the superficial layer of the skin with a tenaculum hook and cutting the conelike elevation off with delicate scissors. The grafts thus obtained contain the epiderm and corium and a slight base of the Malpighian layer. They are immediately transferred, without handling, to the granulating surface and fixed by the gentle pressure of the hook point.
The skin may be transfixed with an ordinary sewing needle and the graft cut away with a delicate flat knife or razor blade, or scissors especially designed for the purpose may be used. (See Fig. 84.)
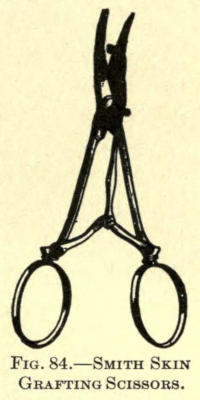
Fig. 84.—Smith Skin Grafting Scissors.
A number of these grafts are often needed to cover a defect, in which case they are placed side by side upon the surface with a little space between their borders. Several such operations may be necessary, as many of the grafts are liable to die from malnutrition, pressure, or defective cutting.
The granulating surface to be covered in this manner must first be cleansed with a weak sublimate solution, followed by a sterilized normal salt solution. When an ulcerated[90] or denuded surface requires skin-grafting, the best time to begin is as soon as there is evidence of the formation of new skin at the edges of the wound; in other words, when reparative action is becoming established. This does not apply to surfaces just denuded over healthy areas for plastic purposes, which should be grafted immediately.
The grafts, having been placed, are covered with a layer of very thin protective silk, or gutta percha, over which a soft gauze or cotton dressing may be applied, borated absorbent cotton being most suitable.
Thiersch recommends the use of gauze compresses saturated in the normal salt solution, which are changed each day.
Another method of covering the grafts is to use perforated silk or small strips of the same material, which permit the dressings to absorb the excretions from the wound and also allow of the free use of either weak antiseptic or sterile salt solutions.
The use of silk or rubber prevents the adhesion of the grafts, which would otherwise be torn away by the removal of dressings, although iodoform gauze answers the purpose very well. It can be safely lifted by first thoroughly wetting it with the normal salt solution.
Strips of tinfoil, first rendered aseptic by immersion in a 1-1,000 sublimate solution and then dipped into sterilized oil or two-per-cent salicylized oil, have been recommended by Socin. Goldbeaters’ skin has also been advocated.
A method that has proved of great value in America is that of skin-grafting in blood. In this method the grafted site is covered with perforated protective silk or rubber tissue, covered with a thin layer of absorbent cotton, or, better, several folds of sterilized gauze, which is kept wet constantly with bovinine. The latter undoubtedly is the means of keeping life in the grafts by supplying the necessary nutrition until the grafts have formed[91] vascular connection, have become firmly adherent, and begin to spread or grow out at their edges.
The living grafts remain as pale islets of skin, which throw out thin epidermal films that meet and grow thicker, until finally the interjoined grafts assume all the functions of normal skin.
It is often necessary to reduce or scarify the edges of the healthy skin that has become thickened where the grafts meet it. This is permissible only when the grafts have become firm and thrive, and may be accomplished by the careful and intelligent use of pure carbolic acid applied with a wooden pick, or by the employment of a stick of fused nitrate of silver, care being taken not to come in contact or to allow the cauterant to touch directly or in solution the new skin.
b. Autodermic Skin-grafting.—Larger pieces of skin may be excised from selected parts of the body, preferably the outer side of the arm, and utilized to cover the entire defect. The piece of skin is cut about one third larger than the size and shape of the area to be covered. This method was first introduced by R. Wolfe in 1876, and gives splendid results. He advises removing all subcutaneous adipose tissue from the graft by gently cutting it away with fine scissors or the razor, and then loosely suturing the flap to the skin surrounding the denuded defect.
Granulating surfaces must first be freed of their loose superficial layers with a sharp curette and the bleeding controlled by sponge-pressure before the flaps are placed. The edges of the wound made by the excision of the flap are simply sewn together, or one of the plastic methods may be used to accomplish the same. Unfortunately these flaps, if they thrive, contract, leaving uncovered spaces, which must be treated separately or allowed to granulate. The dressing in this case is the same as in the Reverdin process.
F. Krause, of Altoona (1896), advocates the use of[92] freed flaps from which the subcutaneous adipose tissue has not been removed, holding that in the healing of such there is less contraction to follow. The success in both of the above methods depends upon an early vascular connection, as considerable nutrition is necessary to supply their want. The blood dressing has aided much in bringing about a happy result. The latter is continued in the manner described for about ten or twelve days, when the grafts may be allowed to depend upon their own circulatory supply. The parts must, in the meantime, be kept at rest and all undue pressure is to be avoided.
These grafts, while becoming organized, change in color more or less from a light gray to a bluish gray and shed off their epitheliar layers, while the cutis vera remains, rebuilding its squamous covering eventually and leaving the surface quite normal.
At times small points of the flap, where subjected to undue pressure or interference, will turn dark and break down, sloughing away and leaving the granulating surface exposed. These areas are, however, soon recovered by skin cells being thrown out from the infral edges of the graft. Often the use of the nitrate-of-silver stick, applied gently at various tardy points, will hasten the process of repair.
The most satisfactory results in skin-grafting are those obtained by the method introduced by Ollier, of Lyons, in 1872, and perfected by Thiersch, of Leipzig, 1874. His method is now almost entirely used for covering large defects. The grafts can be applied over connective tissue, periosteum, bone, and even adipose tissue. The grafts consist of very thin strips of skin taken from the extensor surface of the arm or the anterior region of the thigh, after thorough antiseptic preparation. They should be taken from the patient in preference to those of other individuals or the new-dead or freshly amputated parts.
Granulating surfaces are scraped clean of their superficial or loose layer, while fresh wounds may be covered at once or a few days after having been made, antiseptic compresses being used in the meantime. Hemorrhage is controlled at the time of grafting by sponge-pressure or torsion of the small vessels.
In this, as in the former method, it is desirable that the surface to be covered be free from loose tissue and dry (Garre).
For the removal of the strips the Thiersch razor is to be used. It is concave on its upper side and plane below, the blade being bent at an angle to the handle (Fig. 85). Folding razors of the same type can be procured; their advantage lies in having a protecting case when not in use.

Fig. 85.—Thiersch Razor.
Slide fixation locks are a valuable addition to the latter, as they hold the blade in place when open. See Fig. 86.
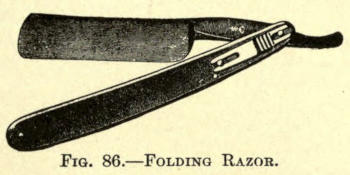
Fig. 86.—Folding Razor.
The site from which the graft is to be taken is first thoroughly scrubbed and washed, then cleansed with an antiseptic solution. The skin of the anterior surface of the arm or upper thigh is usually chosen. The skin of the part is made tense with the left hand, while the point of beginning is slightly raised by the assistant with the aid of a tenaculum hook. The razor, dipped into sterile salt solution, is now taken in the right hand and by quick[94] sawing movements, the plane side being placed next to the limb, a strip of skin is detached (Fig. 87), which, as it is cut, glides in folds upon the concave side of the razor.
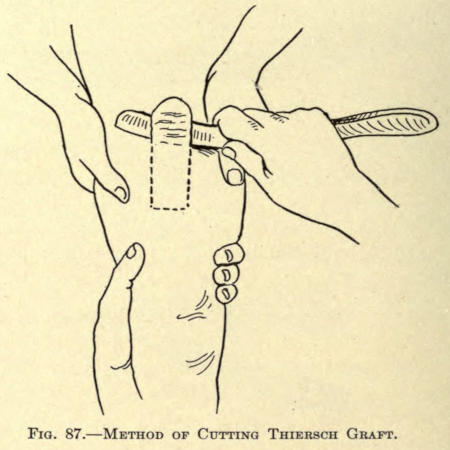
Fig. 87.—Method of Cutting Thiersch Graft.
The uppermost layer of the skin is removed, including epidermis, the Malpighian and papillary layers, as well as a small portion of the stroma. Hübscher includes only the epidermis and the upper portion of the papillary layer, with equal success.
The length and width of the strips so removed must be made according to the defect to be covered. Their width may be made as much as two inches and their length not to exceed four inches.
The collected strip of skin, still on the razor, is now brought to the place of grafting and, with the point of a needle placed at its farther end, is slid off upon the part to be covered and allowed to fall in place by the gentle backward withdrawal of the razor blade, as shown in Fig. 88.
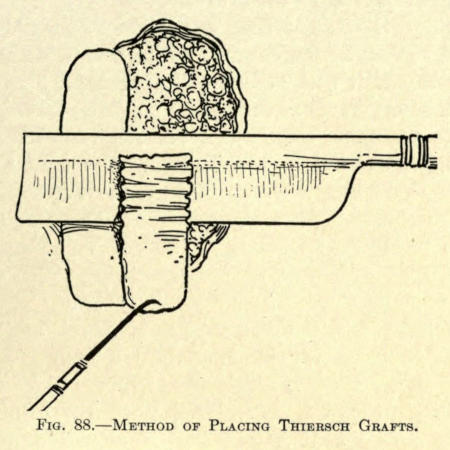
Fig. 88.—Method of Placing Thiersch Grafts.
The graft may be smoothed out with the needle held flatwise or be stroked down gently, so that its fresh surface makes contact with every portion of the part covered, a precaution the author considers important to obtain the best results.
If the defect is large, and where several grafts are needed, the second flap thus obtained is made to slightly overlap the one already placed, and so on. The free, or distal, ends of the flaps are made to slightly overlap the skin or that of a graft placed endwise to it. Every part of the wound should be covered.
As soon as this has been accomplished the strips are powdered over with iodol or aristol or protected with some antiseptic gauze (boric or iodoform), or covered with strips of lint smeared with borated petrolatum, over which light, teased-out pieces of sterilized cotton are placed. A gauze bandage may be utilized to hold all in place.
It is quite necessary to have the part kept at rest so as not to displace the skin-graft arrangement. If the[96] antiseptic powder has been used the dressings need not be disturbed for a week or ten days, but the petrolatum dressing must be changed every third day, care being observed not to disturb the grafts.
Perhaps the best success is obtained by the aid of perforated rubber tissue, covered with gauze dressing, constantly kept wet with bovinine for ten days.
In healing, parts of the grafts may die, leaving small areas to granulate over, but ordinarily the cicatrization resulting therefrom is indeed slight. From the observations of E. Fisher, it seems that the most successful results are obtained when the grafts are taken and transplanted under the bloodless method of Von Esmarch.
c. Hetero-epidermic Skin-grafting.—A novel method of covering wounds with skin is advocated by Z. J. Lusk, of Warsaw, N. Y., 1895, in which small squares of epithelium, previously prepared, are placed upon the granulating surface, over which a dressing of sterilized gauze is placed, saturated with a mixture of balsam of Peru, ʒj, and ol. Ricini, ℥j, and covered with several layers of sterilized absorbent cotton. The dressing is allowed to remain undisturbed until the tenth or twelfth day, unless there is an accumulation of pus.
The advantage of this method is that the epidermal layers can be collected at random from various patients who present themselves with blistered surfaces—the result of burns—or where the skin has been raised by some blistering process for counterirritative reasons.
This loose skin is collected and spread upon a glass plate and sterilized in warm boric-acid solution, then allowed to dry in this position to prevent curling, and, when dry, cut into desirable sizes and laid away for future use.
d. Heterodermic Skin-grafting.—In this mode of skin-grafting the pieces of skin are taken from freshly amputated[97] limbs of one patient or from any selected part of the body of the newly dead, and placed upon the defects to be covered in another patient. These grafts have been successfully employed even after ninety-six hours had elapsed between the time of amputation or the death of a person and the taking of the skin-grafts.
The method employed is as follows: The site of the amputated member or dead body from which the skin is to be taken is thoroughly cleansed, as in the Thiersch method. Pieces of the skin, including the subcutaneous tissue, but no fat, are cut from the cleansed parts. These sections are cut into smaller pieces, about one inch square (Hartman and Weirick), and placed upon the granulating surface to be covered, leaving one-half-inch wide interval between each piece.
The grafts are then covered with overlapping narrow strips of rubber tissue, over which a normal saline dressing is applied. The outer dressing is composed of gauze saturated with the same solution. These dressings are changed every twenty-four hours.
The grafts will soon be found to adhere, showing a pinkish color in about six days; those showing a tendency to undergo gangrene or a laziness of attachment at this time are removed.
In about two weeks the epitheliar surfaces of these grafts are thrown off, as with other grafts already mentioned, and shortly thereafter a new, deep-pink epithelium is formed, the ends of the grafts throw out epitheliar cells, which soon coalesce with those of the neighboring grafts, eventually taking on the normal appearance and vitality of skin.
The advantage of using zoödermic grafts is that the patient is saved the ordeal of general anesthesia and the secondary wound occasioned by the removal of the graft, which necessarily leaves more or less of a scar.
The grafts for this purpose may be taken from freshly killed animals, such as dogs, rabbits, frogs, kittens, etc.
The best results, in the estimation of the author, are obtained by the use of the skin taken from the abdominal region of dogs.
The method for preparing these grafts is to kill a healthy animal, thoroughly cleansing the skin of the abdomen, as already described in the taking of any graft.
The entire abdominal surface is neatly shaved under antiseptic precautions and the skin is dissected off in one piece, leaving the subcutaneous tissue. It is then placed in a warm boric-acid solution and cut into small pieces, say one or two inches square, according to the size of the defect to be covered.
These pieces are placed upon the granulating surface and firmly pressed into place, so that they are in close contact throughout their area. Other pieces are placed quite near or even in contact with the edge of the first, and so on, until the space is entirely covered. Boric-acid dressing of any desired form is placed over them and superimposed by loose gauze and bandage.
The dressing should be left undisturbed for at least forty-eight hours, and then be gently removed and renewed. The utmost care should be exercised with the dressings, since here lies the success of the whole result. The blood dressings have given excellent results in cases undertaken by the author, and should be resorted to whenever practicable. The method has already been fully described, and does not differ in the event of employing zoödermic grafts.
When boric-acid dressings are used, they should be changed every day after the first dressing has been removed, so that the behavior of the grafts can be closely watched.
Lazy grafts and those showing signs of sloughing should be removed at once, and granulations crowding[99] through the grafts should be snipped off with a fine scissors, as they are liable to destroy the life of a graft by pressure or by crowding it away from its bed of nourishment.
As in dermic grafts, the upper layers of these plaques will be thrown off, giving at times the appearance of total sloughing, yet on interference the deeper layers will be found to be intact and healthy. The dressings should be continued until the grafts have not only established their circulation, but until their edges have firmly united and the surface has taken on a dull reddish color, which eventually fades to a shade somewhat paler than the normal skin. The hairs that have been carried over with the grafts at first seem to thrive, but eventually drop out, leaving the surface bare. Spots of color so often observed in the skin of the bellies of dogs also disappear from the grafts, leaving their color uniform.
Amat, in 1895, claims that good results in skin-grafting are obtained by substituting the epidermal pin grafts with the film or inner-shell lining membrane of the fresh hen’s egg. For this purpose as fresh an egg as can be obtained is used. It is broken along the horizontal axis. A delicate forceps is now made to grasp the free membrane found at the air chamber of the enlarged end of the egg. The inner lining is drawn away from the shell in pieces four or five millimeters long; these pieces are cut with a fine scissors into equal lengths and placed with the point of the scissors to the granulating surface to be covered, in the same way as the Reverdin grafts. Amat covered the grafts with tinfoil, over which were placed several lays of carbolized gauze. The dressings were changed every three or four days.
The skin of the frog has successfully been implanted upon granulating surfaces by Baratoux and Dobousquet-Laborderie. They observed that the peculiar pigmented mottling of the skin disappeared about the tenth day, and[100] that the grafts gradually took on the appearance of human skin thereafter.
The best results in this method are obtained with the skin taken from the back of the frog in preference to that of the belly or legs. This skin is cut into pieces about one fourth inch square, which are placed upon the granulating surface in rows, each graft being separate from its neighbor by a space of half an inch.
At the end of forty-eight hours the plaques of skin will have adhered to the granulating surface. At the end of five days they lose their original color and send out cells of epithelium to each neighboring square.
The dressing to be applied over the flaps should consist of borated vaselin, one dram to the ounce, which is smeared upon strips of sterile gauze, over which loose gauze is placed, held in place by a roller bandage.
The skin, once organized, is very thin, as a rule, and requires more or less care for some time after.
The skin of the grafted area will always present a different appearance from that of the healthy skin, both as to color, which is always paler, and in texture. The grafted portion is usually slightly elevated above the healthy skin, giving it an edematous look.
It has been found that skin grafts taken from the negro take more successfully than those from the white race. White skin flaps placed upon the negro do not meet with much success. In this event, however, the newly grafted skin soon takes on the color peculiar to the negro and vice versa (Thiersch).
The investigations of Karg seem to show that the pigmentation of skin is not secreted in the rete, but is carried to it by wandering cells arising from the deeper layer. Von Altmann has discovered certain cell granules, termed by him bioblasts, which he believes are responsible[101] for the production of the pigmentary deposits under peculiar influences of the blood.
The grafting of mucous membrane, both from the animal and man, has been accomplished by Wölfler. His methods are particularly applicable to the restoration of the conjunctiva, mucous membrane of the cheek, etc. Under certain circumstances pedunculated skin flaps have been folded inward to serve as the mucous membrane by Gersuny. When mucous-membrane flaps were taken from the animal, the conjunctiva of the rabbit has been preferred.
Under peculiar circumstances, though rarely, mucous-membrane flaps may be utilized to cover denuded skin areas. The mucous membrane, in such cases, in about ten days takes on the appearance of the skin.
Ofttimes, when it is impossible to obtain foreign mucous membrane, grafts may be taken from the inner surface of the lips of the patient. These grafts answer exceedingly well for conjunctival restorations, while the wound occasioned by their removal is closed by suture or allowed to heal by itself, if not too large, under boric-acid antisepsis.
Bone-grafting, as followed by MacEwen, Ollier, Poncet, and Adamkierwicz, has been more or less successful. Their methods have been often employed in plastic facial surgery, as will be shown later. Their methods were later improved by Senn, who advocated chips of decalcified bone in place of bone taken from young or new-born animals, from which the bones under ossification have been utilized.
Glück’s method of introducing pieces of ivory into bone defects may be of interest, but is applicable only to[102] long bone implantations. The success of his method has yet to be practically demonstrated. Zahn and Fisher have used various foreign substances to overcome bone defects, but these do not interest the cosmetic surgeon to any extent, since other methods have been proved to give better results. These, however, belong to the subject of subcutaneous prothesis, and must be considered separately thereunder.
It may be of interest to know that Schweininger and v. Nussbaum have attempted to graft hairs upon granulating tissue by sprinkling the hairs, with their attached roots, upon the surface to be covered. If any of these lived and attached themselves the root sheath formed a scar center, and the hair dropped out after several days.
Plastic operations about the eyelids are necessitated by and for:
I. Direct injury causing the loss of a part, one or both lids.
II. Loss of tissue following excision of tumor.
III. Loss of tissue, the result of gangrene or ulceration.
IV. Injuries due to burn or acid wounds.
V. The healing and cicatrization following lupus.
VI. The cicatrization following inflammatory lesions of the orbital borders, especially those of the supra-orbital ridge. Since the upper lid lies below the supra-orbital ridge, the above cause is rarely met with.
VII. For the removal of redundant tissue.
The result of the above causes leads to eversion of the lid (ectropion). There may be cicatricial contraction of the conjunctiva leading to ectropion, however, but its correction is not strictly of a plastic nature and belongs principally to the oculist surgeon, and will therefore not be referred to herein.
Ectropion is not uncommon, and involves the lower lid only in the great majority of cases. It may be partial[104] or complete, according to the extent of cicatricial changes in the skin.
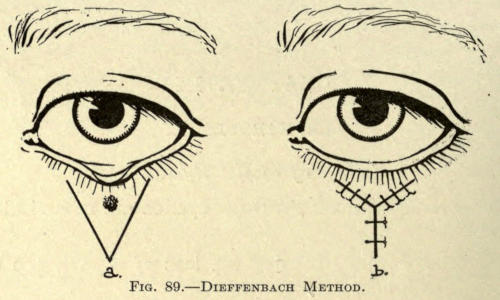
Fig. 89.—Dieffenbach Method.
For the correction of partial ectropion a V-shaped incision is made on the lid with the base of the triangle, including the maximum eversion, as in Fig. 89, a.

Fig. 90a.—Correction of Partial Ectropion. (Author’s case.)
The incisions are made downward from the tarsal border, just below the lashes, and converge to a point. The flap included therein is carefully dissected up, dividing all the scar adhesions, and is[105] pushed upward until the tarsal border at the seat of the defect is overcorrected in this position. The incisions are united with No. 1 twisted-silk structures to form the letter Y, as shown in Fig. 89, b.
As the lid has usually become elongated from prolonged eversion, a small, triangular piece of skin may be excised at the outer end of the lid, with its base turned upward. In bringing the two sides together in linear form, horizontal traction is made along the tarsal line, which aids much in bringing about the desired result.
In the case shown in Fig. 90a the ectropion was the result of the application of nitric acid or caustic potash for the removal of a nevus. It was corrected by the method just described, the result being shown in Fig. 90b.

Fig. 90b.—Correction of Partial Ectropion. (Author’s case.)
Dieffenbach Method.—In complete ectropion the entire lid between the canthi is included in the V-shaped incision just mentioned (Fig. 91) and the flap is sutured as shown in Fig. 92.
In crowding up the detached flap the palpebral border[106] must be overcorrected, since the contractions following union will reduce the effect even to the extent of necessitating later minor operations.
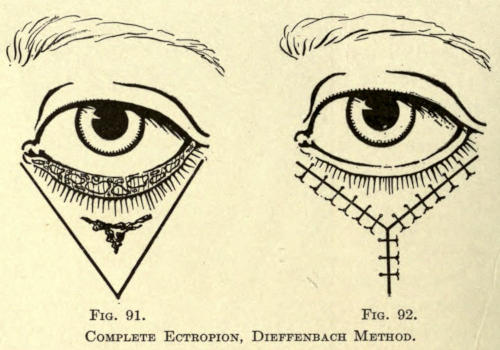
Fig. 91. Fig. 92.
Complete Ectropion, Dieffenbach Method.
To prevent this contraction the palpebral fissure may be united after the correction is made by fine sutures, which are removed in several weeks (Plessing). This is rather uncomfortable for the patient, but there is no question as to the efficacy of the method. A shield can be worn over the eye operated upon after the incisions have united until the lids are separated. This relieves the discomfort of the patient to some extent, while the constant conscious strain to open the eye is greatly overcome by the mere knowledge of the presence of the shield.
If the position, or the extent of the deformity, does not permit of the Dieffenbach method, the following may be employed:
Wolfe Method.—An incision is made parallel to the tarsal border just below the lashes. The scar tissue is then excised. The palpebral fissure is closed by several sutures, as already described, thus drawing up the everted portion and bringing the lids together and causing a large, open wound (Fig. 93).
After the hemorrhage has been controlled a piece of skin about one third larger than the defect is taken from the arm or temporal region of the patient. Next its reverse side is freed of all adipose tissue. It is then laid upon the freshly made open wound, covering it completely, and held in place by numerous fine silk sutures fixing it along the wound margin, as shown in Fig. 94.
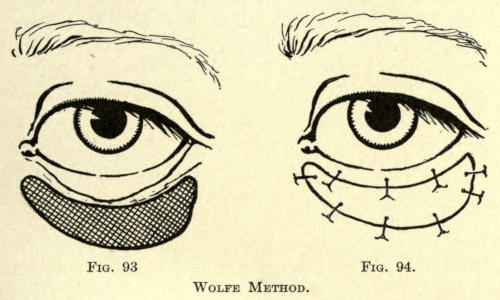
Fig. 93. Fig. 94.
Wolfe Method.
There is more or less contraction of the flap, although primary union takes place. Less contraction of the flap is obtained in the Wolfe method when the subcutaneous fat is not removed, as mentioned above (Hirschberg).
Thiersch Skin-grafting Method.—To somewhat overcome the contraction of the single-graft operation of Wolfe, the Thiersch skin-grafting method may be resorted to as already described. Better results have been obtained with this method. The graft should be placed parallel to the tarsal border. A number of Reverdin grafts can be taken from the temporal region, just below the hair line, and used to cover the wound. These small grafts must be placed quite close together to obtain the best result (Von Wecker). Immobility of the lid is, of course, necessary, and the temporary fixation of the lid must be accomplished as already described. Contraction in this,[108] as in any other skin-grafting methods, is to be looked for and remedied later by minor plastic operations.
Fricke’s Method.—The best results in blepharoplasty, after the extirpation of tumors, are undoubtedly obtained by Fricke’s method. A flap is obtained from the temporal region, with its base in line with the inferior border of the defect to be covered. The flap must be cut to about twice the size of the bared surface, because of the contraction that follows in healing, and also to permit of covering the defect in its longest diameter when twisted. The flap should be taken from the tissues at the outer angle of the eye and cut in the curved form depicted in Fig. 95 to overcome its distortion as much as possible in twisting. It is twisted upon its pedicle at an angle of 90° and sutured into the defect, as shown in Fig. 96.
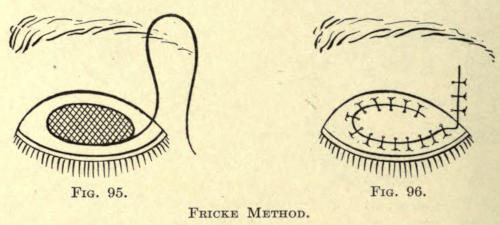
Fig. 95. Fig. 96.
Fricke Method.
The lids are temporarily sewed together, thus stretching the defect fully into which the flap is to be sutured. The pedicle is severed after thorough circulation in the flap has been established.
Owing to the free movement of the skin over the temporal fascia, the wound formed by the incision of the flap can be entirely closed by a single line of interrupted sutures.
Ammon and Von Langenbeck Method.—A very similar method, especially devised for the correction of extensive ectropion of the lower lid, is that in which the pedunculated flap is taken from the latter aspect of the cheek.
A curved incision is made just below the tarsal border, freely loosening the attached conjunctiva in this manner. The cicatricial tissue or other cause of the defect is thoroughly excised and the lids fixed together by suture.
The wound is then fully exposed. A curved incision, as shown in Fig. 97, is now made, with its base in line with the superior line of the raw surface. It is carefully dissected up and twisted into position and held by suture (Fig. 98).
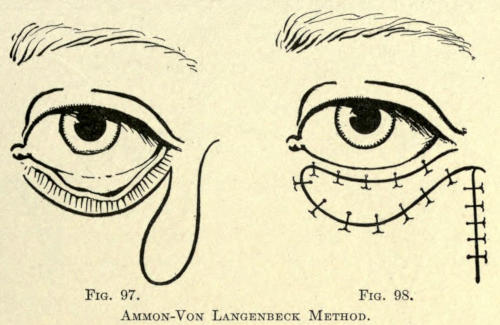
Fig. 97. Fig. 98.
Ammon-Von Langenbeck Method.
The sides of the wound made by the excision of the flap are brought together by an interrupted suture.
The skin of the cheek is liable to contract more readily than that from the temporal region, because it is thicker. Again, it is less suitable for grafting because of its subcutaneous layer of adipose tissue.
Dieffenbach-Serre Method.—Where the defect is too large to be covered with any of the preceding methods, as is often the case following the extirpation of carcinomata, a rhomboid flap can be utilized as shown in Fig. 99.
The extirpation incision is made in the form of a V. The faulty tissue or scar is removed, care being exercised to retain as much of the conjunctiva as possible.[110] A rhomboid flap is then taken from the lateral aspect of the cheek and slid over the defect and sutured into place, as shown in Fig. 100.
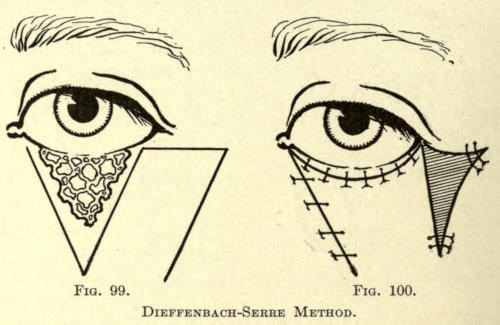
Fig. 99. Fig. 100.
Dieffenbach-Serre Method.
The objection to this method is that the extensive contraction following the healing of the wound made by the raising of the flap causes the lid to be drawn outward. This wound is usually allowed to heal by granulation, but it is better to place Thiersch grafts over the area which cannot be closed by suture, either immediately or as soon as a good granulating surface has been obtained and the sutured portions have become healed.
The outer or free margin of the conjunctiva is sutured to the upper free border of the rhomboid flap or enough of the flap should be at first provided by incision to warrant the turning in of its superior or palpebral border after it is slid into place.
In such case, however, it is best to provide mucous-membrane grafts from the lip of the patient to overcome the loss of conjunctiva (Wolfer).
Because of the splendid success obtained with temporal flaps it is better to follow the method of Fricke in the above operation, changing the shape of the flap to suit the form of the defect to be covered.
Tripier Method.—For the restoration of an entire lid the method of Tripier is to be advocated. A bridge flap with both ends attached is taken from the healthy eyelid (Fig. 101). It is obtained by making the curved inferior incision in a line with the superior border of the tarsal cartilage, and the superior incision parallel to the first at a distance depending upon the size of the defect to be covered. The flap thus formed should include some of the fibers of the orbicularis muscles detached from the tarsal cartilage, making it really musculo-cutaneous.
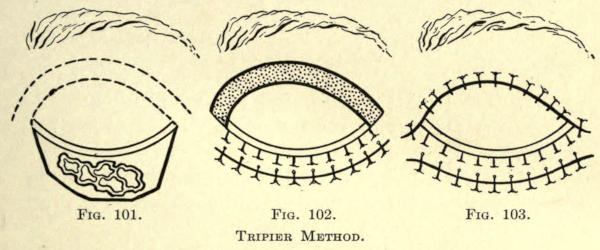
Fig. 101. Fig. 102. Fig. 103.
Tripier Method.
This bridge or musculo-cutaneous flap, attached at both ends, is then gently drawn forward with a tenaculum and slid downward over the upper lid upon the defect of the lower lid, and there retained by interrupted silk sutures (Fig. 102), the superior margin of the bridge flap being sutured to the conjunctival fold freed by the previous extirpation of the lower lid.
The retention of the fibers of the orbicularis palpebrarum in the flap covering the defects is intended to take the place of the part of muscle destroyed by the incision of the faulty tissue in the lower lid, and enables the patient to open and close the lid almost as well as in the normal state.
The margins of the wound made by the removal of the flap are snugly brought together and heal without[112] the least discomfort to the patient, inasmuch as the skin covering the lid is quite loose and elastic (Fig. 103).
Von Artha Method.—It sometimes happens that by the extirpation of tumors part of both eyelids has to be removed. To restore such defect the following method may be followed:
Two sickle-shaped flaps are raised from the skin bordering the outer margins of the primary incision, according to Von Artha, and sliding them about so as to reform the canthus of the palpebral fissure (Figs. 104 and 105).
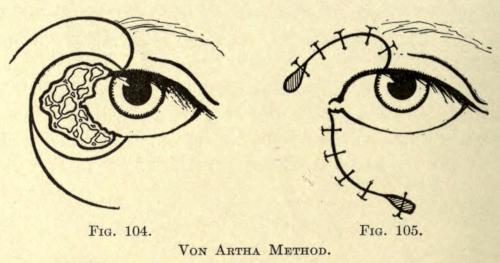
Fig. 104. Fig. 105.
Von Artha Method.
This method leaves little if any secondary effect, its immediate success depending upon the preservance of the conjunctiva at the time of extirpation.
As will be seen, the foregoing method only included operations about the lower lid. The majority of these operations are required only for the lower lid; where defects of the upper lid are to be corrected the flaps and incisions mentioned must be made to correspond to the defect, while in the V-Y method the incision must be inverted.
In the case of ectropion of both lids the palpebral tissue may be sutured for a period of several months with certain benefit, if no other operations can be decided upon.[113] Or the method may be combined with any other plastic operation deemed serviceable for its correction. In most defects of the upper lid, however, if they are not too extensive, the loose skin of the lid itself can be utilized by sliding flap methods to cover the defect (Kolle).
This condition, in which a fold of skin stretches across from the inner end of the brow to the side of the nose covering the inner canthus, is met with principally in children. It usually disappears later in life. It may remain, however, owing to nondevelopment of the nasal bridge and is often met with in the colored races.
Bull Method.—This defect may be corrected by the excision of an elliptical piece of skin from the anterior aspect of the bridge of the nose, and sewing the wound together with interrupted fine silk sutures, as shown in Figs. 106 and 107.
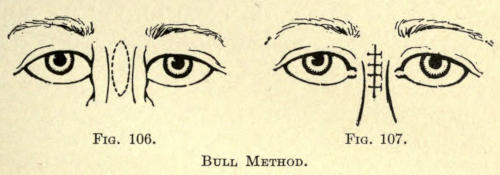
Fig. 106. Fig. 107.
Bull Method.
Paraffin Injection.—As the above operation leaves a linear scar on the anterior nasal line, the author has found it much better to correct the defect by building up the nasal bridge, or the entire anterior nasal line by the subcutaneous injection of one of the paraffin compounds, thus overcoming both the epicanthus and the nasal deformity. In fourteen cases, two Japanese and the rest negroes, the author has obtained excellent and permanent results.
The process herein referred to was first suggested in a general way by Gersuny, and has been extensively and[114] successfully utilized in many ways, especially in this country. A special chapter is given to the method elsewhere.
Following the injection of the substance employed there is slight swelling for a few days, which may or may not involve the eyelids. This disappears about the second or third day. The injected material becomes organized in two or three weeks’ time and gives no further trouble to the patient.
If the patient complains of a dull pain or soreness in the area thus operated upon, the application of cold extract of hamamelis is to be applied on little squares of sterilized gauze, which usually relieves the discomfort in a few hours.
Canthoplasty involves the lengthening of the palpebral fissure at the external canthus. The canthus is divided outward to the extent designed with a pair of angular scissors, probe pointed (Fig. 108), and to the extent as shown in Fig. 109.
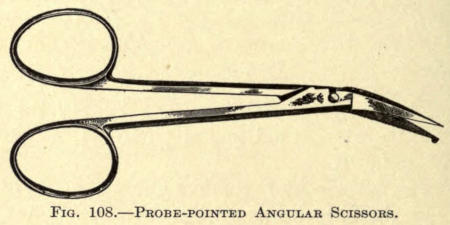
Fig. 108.—Probe-pointed Angular Scissors.
The contiguous ocular conjunctiva is dissected (Fig. 110) up and attached to the newly made skin margin with silk sutures to prevent its reunion, one suture uniting the angle of the wound with the raised tip of conjunctiva (Fig. 111).
The sutures are allowed to remain about five days.[115] Traction with the fingers should be made several times each day to thoroughly separate the wound and to prevent the contraction of the conjunctival triangle, which would offset entirely the object of the operation. As a rule the fine silk sutures heal out of the mucodermal margins owing to the softening of the tissue through the increased lachrymal secretion caused by the irritation of their presence and the resultant reaction following the operation.
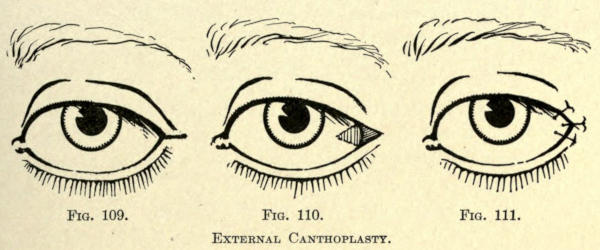
Fig. 109. Fig. 110. Fig. 111.
External Canthoplasty.
A slight regional conjunctivitis usually follows this operation, yielding readily to simple treatment, often requiring no special care but the hygiene of secondary-wound antisepsis.
This is a drooping of the upper eyelid, due to congenital or paralytic causes. It may be unilateral or bilateral.
Apart from internal and proper external electrical and other treatment the simplest surgical method to be employed is to remove an elliptical piece of skin from the eyelid and to suture the margins of the wound together. Care should be taken not to take out too much tissue, as this would involve inability to close the lid.
A condition in which the two lid margins are united by cicatricial adhesion. These should be removed and the margin of the lids be rebuilt by any of the methods suggested if possible. Mucous-membrane flaps are naturally to be preferred.
A common condition after middle life, when not due to other causes than normal changes in the skin and subcutaneous tissue. Edematous pressure due to disease is a common factor.
The wrinkling may be marked or slight.
To correct the condition is to remove the redundant or baggy tissue by excision, as massage in any form accomplishes little if any benefit. The shape of the incision should be made to include the loose tissue and varied somewhat, as shown in Figs. 112 and 113.
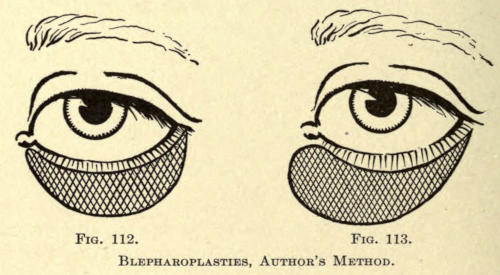
Fig. 112. Fig. 113.
Blepharoplasties, Author’s Method.
The superior line of incision in operations of the lower lid should be made as close to the tarsal line as is practical, so as to show as little of the resulting scar as possible. The best distance is about an eighth of an inch below the tarsal cartilage fold. Accuracy in making the[117] superior line of the incision is furthered by outlining the flap to be removed with a very fine bistoury.
In operations about the upper lid a somewhat widened elliptical piece of skin is excised with its inferior margin about one fourth to one half inch above the tarsal line, so as to allow the line of union to lie above it and within the curved fold when the eye is open.
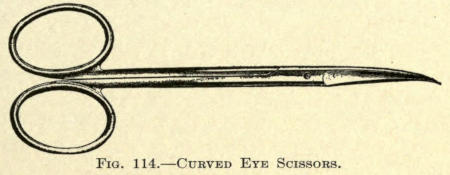
Fig. 114.—Curved Eye Scissors.
For the excision it will be found best to use a fine pair of curved eye scissors, beginning the incision by raising the skin at the outer canthus with a fixation forceps or tenaculum.
Another guide to outline the necessary amount of tissue to be removed is to mark the area, prior to operation, with India ink or an indelible pencil. The parts can then be snipped away readily without fear of causing ectropion. There is usually very little bleeding, and in most cases the tissue is exceedingly thin.
The margins of the wound are brought together with very fine twisted silk, using the continuous suture preferably on account of the ease with which it can be removed.
The wound is then powdered with a suitable antiseptic powder and covered with antiseptic adhesive silk plaster moistened with an antiseptic. The form of the plaster should be of suitable shape, not too wide, and nicked so as to permit of proper application.
There is more or less edema following the operation, associated with or without discoloration, which disappears usually without treatment in forty-eight hours. It is advisable to administer a saline laxative each morning[118] following the operation for several days. Small doses of magnesium sulphate answer the purpose very well.
The sutures are withdrawn in from twenty-four to forty-eight hours after having been carefully softened with warm boric-acid solution, or a ten-per-cent peroxid-of-hydrogen aqueous solution. The early removal of the sutures prevents stitch cicatrices. The part is again powdered as before and covered with the adhesive silk plaster, which answers both purposes of protection and splinting.
The resulting cicatrization is so surprisingly little as to be almost invisible in the great majority of cases. In patients of blond complexion the redness of the scar disappears as early as three weeks, but is more prolonged in persons of darker type. It is not advisable to do both upper and lower eyelids in one operation to avoid the discomfort of the edema which usually follows.
In rare instances there appears a hypertrophy of the scar line, which is best treated with strips of thiosinamin plaster mull, twenty per cent, applied nightly and removed the next morning. If irritation results the plasters should be discontinued for a day or two.
A yellow discoloration of irregular patchlike formation in the skin of the lids, usually about the region of the inner canthus.
The condition may involve both upper and lower lids symmetrically. The patches are generally slightly elevated and vary in size. They make their appearance usually late in life, and are due to the infiltration of the deeper layers of the skin with groups of cells overburdened with fat.
They are best removed by excision, following the method of the preceding operation. There may or may[119] not be a recurrence of the disease at an indefinite period, when the tissue must again be removed.
All of the above operations in blepharoplasty can be done under local anesthesia, using either the two- or three-per-cent cocain or, preferably, Beta-eucain solutions.
About ten minutes after each operation a sharp stinging sensation is experienced in the eyelid operated upon, which lasts for almost an hour or more, and indicates nothing alarming except the absorption of the anesthetic and a return to the normal state. A sponge dipped into cold sterile water relieves the parts considerably at the time.
It is advisable to inform the patients of this symptom beforehand to avoid unnecessary alarm on their part. Patients are easily frightened when cutting operations around the eye are undertaken, and should be apprised of what is to be done, and what to expect, especially when the operation has been done as a purely cosmetic one.
After the sutures are removed the patient is instructed to allow the plasters to remain until they fall off, which occurs usually in about two days, unless there be reasons for dressings for discharges due to infection, the result of carelessness in operating.
Should at any time, from carelessness or accident, the wound be torn open, the parts need only be brought together with adhesive silk plaster. Healing will go on, giving practically as good a result as with the suture. Bardeleben does not suture these wounds at all, yet the author believes it a safeguard and a psychological necessity in most cosmetic cases.
This branch of surgery has to do with the corrective and restorative operations of and about the external ear.
Traumatisms of the auricle, owing to the exposed position of that organ, are frequently met with and are commonly the result of stab wounds, direct blows, shot wounds, and human bites, especially in Spaniards and Italians, who follow this queer kind of revenge upon one another.
Such wounds of the ear may involve only part of or the whole of the auricle. Loss of auricular substance may also be the results of gangrene following freezing or the direct result of burns.
Fracture of the cartilage of the ear is exceedingly rare (Schwartze).
Where the injury is one of incision or laceration without loss of the part, the site should be cleansed gently but thoroughly with a boric-acid solution, and the free torn edges brought together with fine silk sutures. If the cartilage projects unduly into the line of union it should be trimmed away with a fine pair of scissors (Roser). Wounds of such character usually heal well, even if the pieces hang loosely by threads of skin, a linear indent of cicatricial tissue usually marking the traumatic separation of the cartilage.
In the negro where razor cuts about the ear are often seen, a hypertrophic scar or keloid is liable to result,[121] even to the extent of involving the punctures of the suturing needle.
It is advisable to save all that is left of the injured member, even if entirely severed, with the hope of obtaining union, since the rebuilding of even part of an ear is by no means an easy matter, owing to the complicated formation of the cartilaginous frame.
Wounds about the meatus are liable to result in stenosis, which should be guarded against by packing of small strips of gauze or in the case of loss of substance immediately about the orifice by the employment of a sliding flap taken from the skin of the vicinity or by the transplantation of a nonpedunculated skin flap taken from some other part of the body and sewn into place.
If a loss of substance of the auricle cannot be avoided, the surgeon must rely upon otoplastic means to make up the deficiency.
For the best cosmetic defects it is desirable to have as much of the cartilage remaining as possible. The stump of the ear is freshened at its outer margin with the bistoury and the frontal skin carefully dissected away from the cartilage to the extent of a quarter inch.
A flap, one third larger than the defect to be supplied, is now outlined on the skin back of the ear in such a way that the flap included therein will not be subjected to too much torsion.
This flap must necessarily vary in shape and size, according to the nature of the deformity to be corrected. It may even extend into the hair of the scalp over the squamoparietal region of the head or a part of the neck laterally and below the ear.
This flap, after careful estimation as to size, should be dissected up freely down to the periosteum, leaving a bridge of tissue at the point where the least resistance[122] will be caused after its free end has been sutured to the remains of the ear.
The free flap is stitched to the stump with several silk sutures. After bleeding has been controlled, a few layers of borated gauze are introduced under the flap to prevent its reattachment and to encourage its thickening, and the entire site of the operation dusted over with an antiseptic powder, and covered with loose folds of sterile gauze. A bandage can be lightly applied over the whole to keep the parts in place.
The success of union of the flap depends upon the immobility of the parts while healing is taking place. The patient is to rest at night in a semirecumbent position with the head held down firmly on the uninjured side with the aid of a tight-fitting linen cap made for the purpose and tied by attached tails of the same material to the bed in such a way that the head cannot be turned during sleep, yet allowing of more or less movement in either direction, never enough, however, to cause tension in the flap. During the day the patient should be on his feet as usual, since the operation is hardly severe enough to compel absolute rest.
As soon as the union of the flap to the ear has been established, which is about the eighth day, the sutures are carefully removed to avoid irritation, but the pedicle of the flap is not to be severed until the tenth or fifteenth day, when satisfactory circulation has been established.
The flap when severed will shrink more or less, but will be seen to be somewhat thicker than when dissected up in the primary operation.
Nothing should be done for a few days hereafter except to keep the granulating surfaces of the flap and back of the ear aseptically clean and healthy.
As soon as the flap loses its pale color and takes on a pinkish glow it may be deemed safe to cover the granulating or secondary wound on the head with grafts of skin, using whatever method most suitable for the purpose.[123] The transplantation of a single flap of skin taken from the anterior border of the arm is perhaps productive of the best result.
To assure of success the graft may be healed under the blood dressing; the methods for which have been fully described heretofore.
Once the secondary wound is healed the surgeon’s attention must be given to the flap attached to the stump. By the aid of the judicious use of the nitrate-of-silver pencil certain parts of this flap may be stimulated to become thickened.
The upper or outer border of the flap should be taken under operation first to form the new helix of the ear. This can be done by making several incisions along its free edge and gently turning backward these small flaps so that their raw surfaces face that of the flap.
This procedure, if neatly done, will eventually give a thickened border to the superior rim.
Should the flap have been cut large enough to permit of lining its entire back this can be done, but care must be exercised not to cause a too abrupt folding over of the same, as gangrene is likely to result. The more slowly this freshening is accomplished the better will the result be eventually.
If, however, this flap will not permit of autolining, and its raw surface presents a healthy granulated appearance, recourse may be had to the transplantation of a flap from the arm upon it and fastened to the denuded edges of the aural flap.
As soon as healing has been established a number of delicate, often complicated incisions are made in the newly formed part of the ear to give it proper shape and size.
Kuhnt has obtained excellent results in a case where he employed a flap from the back of the ear, combined with two pedunculated tongue-shaped flaps taken from the cheek above and the neck below, which he twisted[124] about back of the flap of the newly formed ear, so that their epidermal surfaces faced its raw surface with the object of giving greater thickness to the ear at that point.
At best, however, the restoration of an entire ear may be considered impracticable, and only in such cases where the greater part of the ear remains can cosmetic results be looked for.
In the illustration shown the author restored the upper third of the ear shown above the line drawn obliquely across the ear. Seventeen delicate operations were necessary to obtain the result (see Fig. 115).
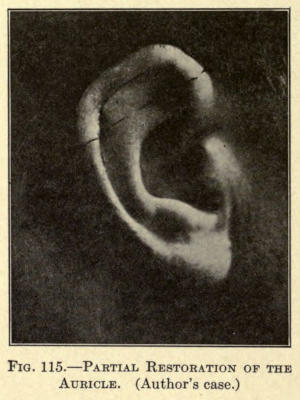
Fig. 115.—Partial Restoration of the Auricle. (Author’s case.)
Where the loss of substance is not too great and along the helix of the ear, a flap can be taken from the back of the ear, leaving it attached at its cicatrized union with the primary wound, and sliding this flap upward or outward until the defect of the helix is overcorrected to allow for contraction and suturing the flap in its new position.
The secondary wound if too large to permit of direct union with sutures may at once be covered with a flap taken from the anterior border of the arm, or, if preferred, from the inner aspect of the calf of the leg. The wound occasioned by the removal of the graft can easily be closed by suture, leaving simply a linear scar of little consequence. Usually such defects of the rim can be hidden by the combing of the hair, especially in women.
When the injury has resulted in complete loss of the organ or so much of it that its remaining stump will not permit of otoplasty, protheses or artificial ears or parts of ears may be employed to render the patient less unsightly. These protheses are usually made of aluminum, papier maché, or rubber, and painted to match the good ear. They are attached with a special kind of gum, termed zinc-leim, which makers of such protheses furnish, or are held by metal springs, which are inserted under strips or bridges of skin surgically created for the purpose. The esthetic effect is surprisingly good in most cases.
A very common injury observed in women is laceration of the lobule of the ear or ears, generally due to the wearing of heavy earrings, which gradually cut their way through the tissues. Coloboma may be occasioned by the forcible tearing out of the earrings; it has also been found to be congenital in rare cases.
The simplest method for correcting this deformity is to cut away both cicatrized edges of the defect by the aid of the angular scissors, exposing fully the width of the lobular tissue on both sides (Fig. 116), as the cicatricial edges are likely to be thinner than the lobule proper, and if brought together would leave a depression along the line of union. The freshened cut surfaces are brought together with fine silk sutures, an inferior one being taken in the outer border, so as to establish perfect coaptation at this point (Fig. 117).
The objection to the above operation is that invariably owing to the resultant contraction a notch is formed at the union of the angles of the freshened wound. To avoid this the operation shown in Fig. 118 is to be employed (Greene).
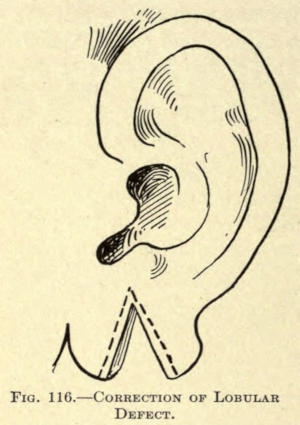
Fig. 116.—Correction of Lobular Defect.
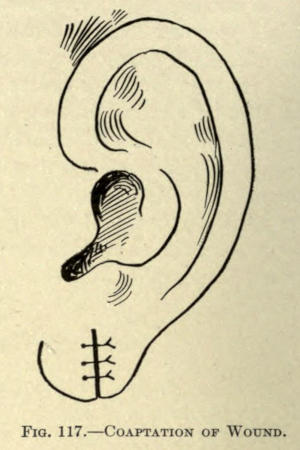
Fig. 117.—Coaptation of Wound.
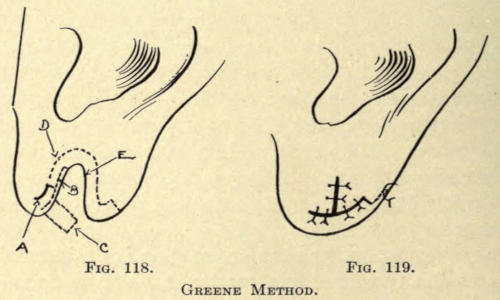
Fig. 118. Fig. 119.
Greene Method.
The bistoury is thrust through the lobule at the point A and an incision is made to follow at a little distance the defect along the line D. This frees the cicatrix except at the pedicle A. A transverse incision is now made above the point A corresponding to the curved exsection of the opposite side except for a thin strip of tissue B.[127] This delicate little flap is preserved and severed a short distance beyond.
The raw edges when now brought in apposition will assume the form in Fig. 119. The wound is sutured as in the simpler operation.
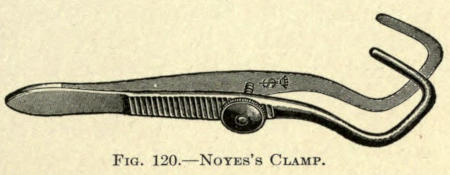
Fig. 120.—Noyes’s Clamp.
These operations are best performed under local anesthesia, the two-per-cent eucain being preferred. There is practically little bleeding, but even this may be avoided by applying a large Noyes’ compression clamp with its angular arms so placed as to include the entire lobule (Fig. 120).
There may be an enlargement of or an absence of the lobule.
In the enlargement of the lobule the operation last described may be resorted to, making the now supposed coloboma the triangular amount of tissue to be removed. It will be found that the upper curve of the incisions must be carried much higher in cases of this kind, furthermore, that they should define a sharper angle at this point.
The simple exsection of a triangular piece of the lobule and suturing is commonly practiced, with the objection of the notch previously referred to. This operation is very quickly done, and if care be taken in bringing the raw surfaces together neatly a splendid result is[128] attained, especially if the incisions are made obliquely to the plane of the skin.
There may be a shortening of the lobule, or, as is more frequently seen, the attachment of the inner lateral border of the lobe to the skin opposite.
This attachment of the lobe has been alleged by criminologists to be a mark of the degenerate. If this be so it can scarcely apply to the Japanese, in whom it is found as a racial fact.
As the defect is often objected to by patients its correction may be considered briefly.
An incision is made in the inferior auricle and in the skin below it, as shown by the dotted lines in Fig. 121, removing the triangular piece of tissue included therein.
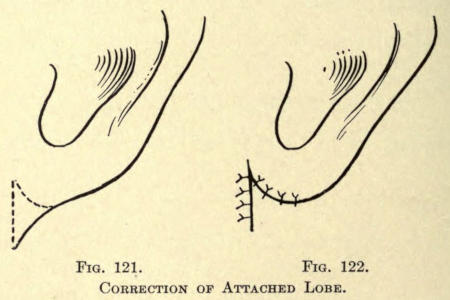
Fig. 121. Fig. 122.
Correction of Attached Lobe.
The wound is then sutured with fine silk, as shown in Fig. 122, and allowed to heal. The result is very gratifying in most cases.
Malformations of the ear are due to the arrest of development, termed microtia, excessive development, or macrotia, and malposition.
The total absence of the auricular appendage is quite rare. One or the other part of the ear is usually found, either partially or fully developed, giving to the ear an irregular rolled-up appearance. This defect may be unilateral or bilateral.
It may be associated with congenital fistula (Fistula auris congenita), varying in length from one fourth to one inch, and secreting a serouslike fluid. These fistulæ are usually found anteriorly and above the tragus, the lobule, or more rarely at the crus helix, or even behind the ear. Sometimes these fistulæ communicate with the middle ear or even the esophagus. They are due to imperfect development in utero. In microtia little can be done surgically, since the malformation is usually so pronounced as to exclude all methods of restoration.
Szymanowski advises making an ear from the skin immediately back of the auditory canal if present, making the incisions of the shape shown in Fig. 123.
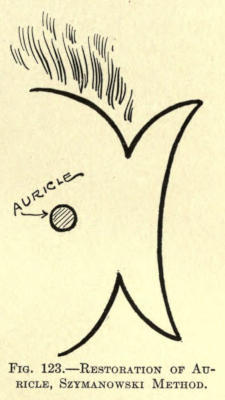
Fig. 123.—Restoration of Auricle, Szymanowski Method.
The flap included in these incisions is dissected up and doubled on itself posteriorly. The doubled flap thus formed is brought forward and placed as near into the linear position as the ear should have. The flap is then sutured through and through to make the raw surfaces heal together. The secondary wound and the treatment of the flap are carried out as already referred to under restoration of the auricle.
Several later delicate operations are done to add to the shape of the newly made organ, but at best the effect is far from even good.
In the case of Mr. B., illustrated in Fig. 124, an attempt was made to enlarge the somewhat elastic roll of tissue corresponding to the helix by several injections of paraffin. The result proved to be anything but satisfactory; in fact, the prominence of the malformed upper ear was made more evident, and painful when subjected to pressure, so that the patient was compelled to refrain from lying on that side of the head.
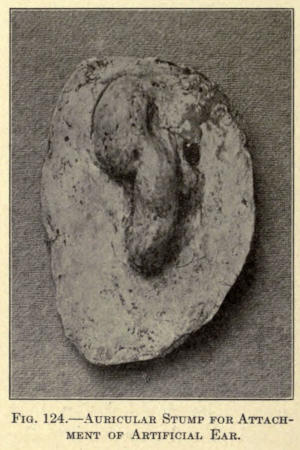
Fig. 124.—Auricular Stump for Attachment of Artificial Ear.
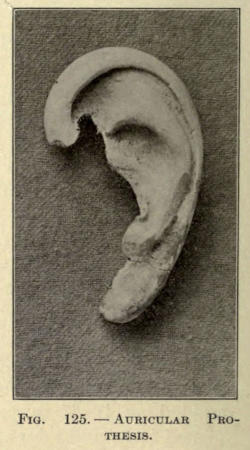
Fig. 125.—Auricular Prothesis.
There had been also congenital atresia of the auditory meatus, which had been operated for, leaving a hair-lined opening, leading down to a useless middle ear, a condition sometimes associated with microtia.
In presenting himself to the author for operation it was decided that the otoplastic methods for the restoration[131] of the ear were out of the question, as is usually the fact in these cases.
The hard mass of tissue referred to and corresponding to the helix was reduced considerably, so that the stump obtained was soft and pliable, with not only the object of overcoming the sensitiveness and inconvenience of the part, but to obtain as good a base for the attachment of an artificial ear as possible (see Fig. 124).
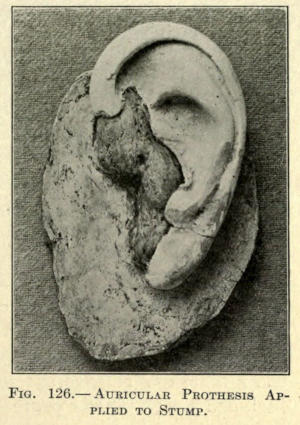
Fig. 126.—Auricular Prothesis Applied to Stump.
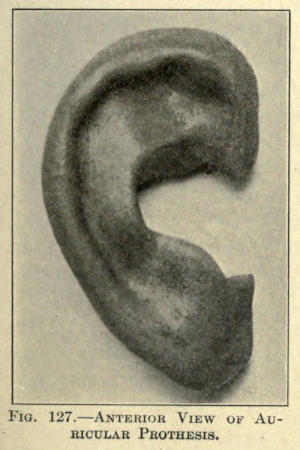
Fig. 127.—Anterior View of Auricular Prothesis.
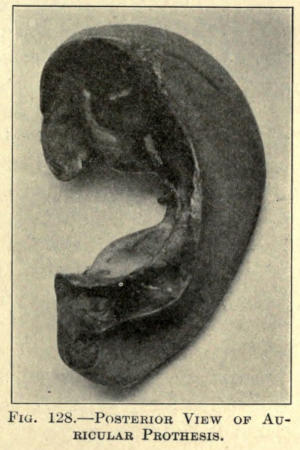
Fig. 128.—Posterior View of Auricular Prothesis.
The author advises a complete amputation of such underdeveloped ears, since a better and firmer seat of[132] attachment is offered thereby to the prothesis to be worn over it, at the same time giving the artificial organ a better position in reference to its normal relation to the face. An irregular stump makes this more or less difficult, as in the case just referred to, but even these patients are loath to part with an irregular ugly mass of tissue they consider themselves thankful to be born with.
The auricular prothesis used in this case is shown in Fig. 125, and its position and appearance when placed on the stump is shown in Fig. 126.
Another, showing both anterior and posterior surfaces, is given in Figs. 127 and 128.
The fistular conditions mentioned should be thoroughly dissected out and healed from the bottom when practical by antiseptic gauze packing. Those involving the middle ear require special treatment that cannot be included under plastic procedure.
Abnormal enlargement of the ear is often found in the idiot, but is commonly seen as a hereditary defect in many without having the least relation to the mental development of the person. These conditions occur more frequently in men than in women.
Enlargement always depends upon overdevelopment of the cartilaginous structure of the auricle, and may also be the result of direct violence, the result of blows upon the organ, as in prize fighters, football players, and other athletes.
Following violence the auricle undergoes either an acute or chronic hypertrophy of the chondrium, resulting in the condition known as the “cauliflower ear.”
Again, there may be hematoma occasioned by direct violence, termed othematoma traumaticum, or a spontaneous development of such hematoma without any appreciable injury, as found in the insane. In the latter form the disease appears suddenly without warning or[133] inflammatory manifestations, the hematoma reaching its full size in three or four days, after which a passive resolution in the form of absorption of the tumor takes place associated more or less with an organization of the blood mass, and leaving the auricular appendage unduly enlarged, distorted, and thickened, with here and there islands of seemingly detached or displaced cartilage firmly adherent to the overlying skin.
Early in these cases much can be done by the application of external medication, depletion, and pressure bandage, and the removal of the effusion producing the swelling and lying between the perichondrium and the cartilage, by the introduction of a trocar cannula or by incision, as may be required.
The union between cartilage and perichondrium is always slow, requiring about three weeks in the traumatic variety and often months in the noninflammatory form.
Be the enlargement due to whatever cause, the patient not infrequently presents himself for a correction of the deformity.
The slightest of such deformities is a tiplike enlargement of the outer and upper angle of the helix, most commonly unilateral. This has been termed “fox ear.”
In this condition there is more or less loss of the curl of the helix, with flattening beginning well down in the fossa, extending upward, and terminating in a triangular cartilaginous tip resembling the ear of an animal, hence the name.
The correction of this fault is quite simple. An incision somewhat larger than the base of the cartilaginous triangle is made under a local anesthetic about one fourth inch below and back of the line corresponding to the superior border of the helix. The cartilage is exposed through this incision and excised with a fine curved scissors without wounding the anterior skin of the helix, and the incision neatly sutured, leaving the now redundant skin to contract.
In this manner the fault is corrected without any appreciable scar.
The sutures can be removed in three or four days.
In the correction of macrotia various surgical methods may be employed, yet none can be emphasized, as exclusively indicated, inasmuch as the enlargements may involve one or the other part of the pinna.
The greatest fault with most of these ears lies in the overdevelopment of the triangular antihelix or that area lying posterior to the fossa of the antihelix and the fossa of the helix, although in many cases the greatest malformation is found in the concha itself.
The following methods for operation are therefore given not so much for their individual merit, but to act as a guide in the selection of an appropriate election or modification for specific cases.
Schwartze Method.—Schwartze advises and has obtained excellent results by removing a long elliptical piece of the entire thickness of the pinna, including both skin and cartilage, from the fossa of the helix, followed by the excision of a triangular section with its base corresponding to the outer border of the helix and its apex terminating well in the concavity of the concha. The scheme of[135] procedure is shown in Figs. 129 and 130. The raw edges are brought together by fine silk sutures, which are made to pass directly through the cartilage, and tied carefully to prevent any change of the transfixed parts, which would mar the result of the operation more or less and necessitate further interference. The arrangement of the sutures and the disposition of the parts are shown in Fig. 131.
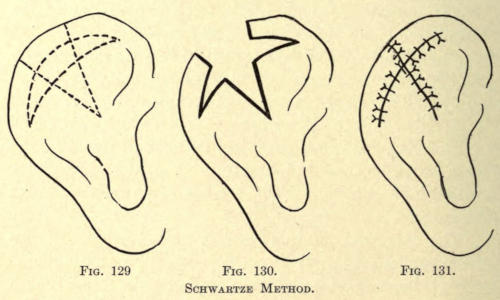
Fig. 129. Fig. 130. Fig. 131.
Schwartze Method.
Parkhill Method.—Parkhill advises a semilunar incision from the fossa of the helix with a rhomboidal exsection of the helix, as shown in Fig. 132, and suturing the parts, as shown in Fig. 133.
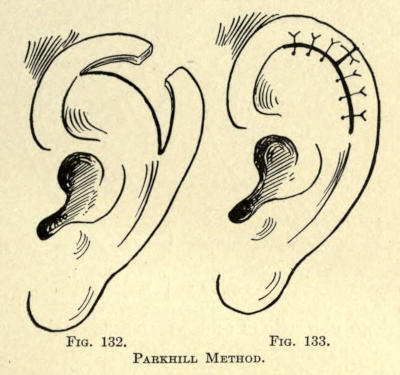
Fig. 132. Fig. 133.
Parkhill Method.
The tonguelike ends of the semilunar incisions must, of course, vary in length, according to the amount of tissue necessary to remove to facilitate accurate juxtaposition of the newly designed flaps.
Author’s Method.—The latter operation is most successful where the upper part of the pinna is unusually flat. It does not correct this flatness, however, which is often an objection, hence the author suggests excising a section of the entire thickness of the ear from the fossa[136] somewhat in the form shown in Fig. 134, curving the two deeper invading incisions, so that when the parts are brought together a concavity will be given the antihelix, as in the natural auricle.
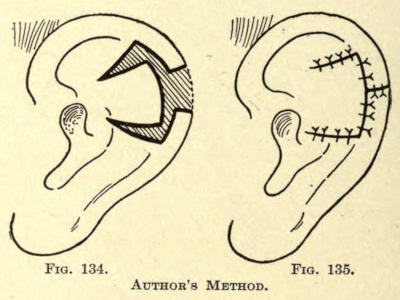
Fig. 134. Fig. 135.
Author’s Method.
The rearrangement of the parts in this event is shown in Fig. 135. The only objection to the above may be found in the two linear scars across the antihelix entirely overcome by the Parkhill operation, wherein the line of union falls just below the rim of the helix and into the groove commonly found there, yet any of these scars shows little in well-done operations and when union takes place by first intention.
There will always appear a notchlike depression where the newly cut ends of the helix are brought together, owing to the cicatrix involving the space between the cartilaginous borders.
Inasmuch as this notch necessarily shows the most prominent part of the ear, the author advocates the following method in which the notch is brought anterior to the fossa of the antihelix; in other words, near to the point of the union of the helix with the skin of the face about on a line with the superior border of the zygomatic process; a point where the hair is in close proximity with the ear and where the scar can be more easily covered.
The form of incision is somewhat sickle shaped, the upper curvature of the incision following the inferior border of the helix and extending well into the fossa of the helix, as shown in Fig. 136. Where the antihelix is particularly large a triangular section may be removed, as shown at A, with a corresponding shortening of the helix flap at B. The latter gives more contour to the ear as well.
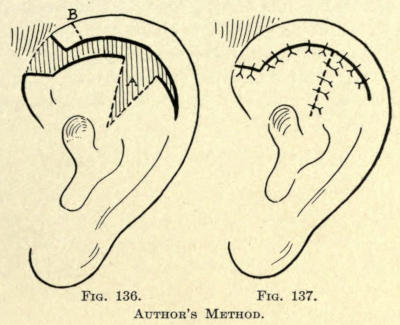
Fig. 136. Fig. 137.
Author’s Method.
The parts are brought together and sewn into position, as shown in Fig. 137.
Small nipplelike projections of skin or elongated tumefactions of connective tissue are sometimes found about the tragus, the lobule, or on the neck. They are easily removed by encompassing their bases with an elliptical incision and amputating them a little below the level of the skin and suturing the wound in linear form.
Auricular appendages may contain small pieces of cartilage or resemble crudely the auricle in miniature.[138] This condition is termed polyotia. One or more of these supernumerary ears may be found anterior or posterior to the true ear or even below it on the skin of the neck.
In the case reported by Wilde there were four ears, the two abnormal ones being situated on the neck at either side. Langer has reported a similar case. The condition may be unilateral or bilateral.
This congenital malformation is corrected by simple amputation, as described under minor auricular appendages.
The most common deformity met with in ears is undue prominence. The ears stand out from the head at an obtuse angle, often lopping forward and downward, giving the patient a stupid appearance. This condition is usually inherited, but may be acquired during childhood by the careless wearing of caps that crowd the pinnæ forward and away from the head. The habit of ear-pulling is also said to be a cause, also the faulty position of the head during sleep. The deformity is usually bilateral, but in the majority of cases one ear usually projects more than the other.
Where the deformity is recognized during infancy the ears should be simply bandaged to the head with a suitable bandage or ear cap, procurable for that purpose with the hope that the cartilages may thus be influenced during their period of hardening and growth.
Invariably these patients are seen too late, and operative procedures alone will restore the ears to their normal position.
The earlier in life such an operation is performed the more satisfactory is the result, inasmuch as the cartilage of the ear is more pliable, and hence more susceptible of readjustment; moreover, the operation when done early in life necessitates only the removal of an elliptical piece of skin from the back of the ear, according[139] to Monks, and suturing of the wound, as shown in Fig. 138.
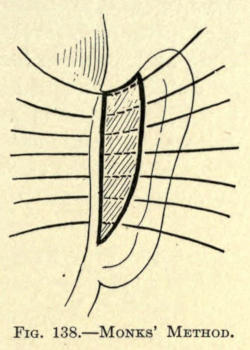
Fig. 138.—Monks’ Method.
The elliptical form of the incision must, however, be changed according to the varied prominence of various parts of the ear. When the ear lops forward, it should be broader above and narrower below, and vice versa in the event when the concha is overprominent.
When the patient is less than fourteen or fifteen years of age a general anesthetic should be employed, but in older patients the operation can be easily undertaken under local use of two-per-cent eucain solution.
Author’s Method.—The method followed by the author is to thoroughly anesthetize the back of the ear, the patient lying in a recumbent position with the head to one side, sufficient to place the ear to be operated upon in as convenient position for operation as is possible. A rubber cap is drawn over the head to cover the hair.
An incision is now made along the whole of the back of the ear as far down as the sulcus, where the retro-aural integument joins that of the neck.
The incision should involve the skin only, and vary from three fourths to one half an inch from the outer border.
At once the blood will ooze from the line of incision. The operator now presses the ear backward on the bare skin of the head, leaving an imprint of the bleeding line on the skin there.
A second incision is made along this line, giving the total outlining incision a heart-shaped form, as shown in Fig. 139.
The skin within this area is now dissected up quickly.[140] There will be more or less bleeding from the post-auricular vessels, which can easily be controlled by sponge pressure, or with one or two artery forceps of the mosquito-bill pattern. The wound should be large enough to overcorrect the fault, as the ear springs out more or less when healed.
Sutures are now introduced. When necessary one or two catgut sutures are taken through the concha, not going through the anterior skin, however, and the deeper tissue back of the ear and tied. These hold the cartilage in place.
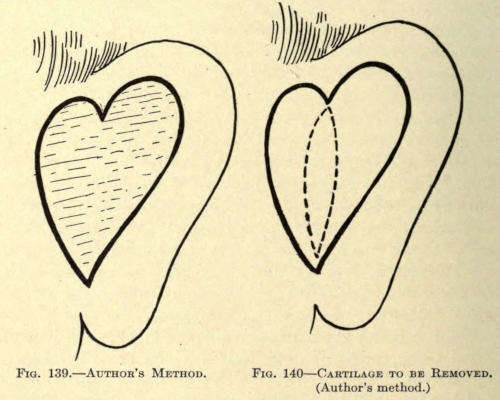
Fig. 139.—Author’s method.
Fig. 140.—Cartilage to be Removed. (Author’s method.)
For the coaptation of the skin the continuous suture is to be preferred, but when the cartilage suture is employed it will be found impracticable, owing to the close position of the ear to the head. In that event interrupted sutures must be placed, as shown in the Monks operation, and tied after the cartilage has been fixed as described.
Where it is deemed necessary to fix the cartilage in this way, the author advises to remove an elongated elliptical piece of the concha, as shown in Fig. 140.
This is neatly done by outlining the section with the scalpel, and excising it with the aid of a fine pair of scissors, half rounded; the operator holding the index finger of the left hand in the depression of the concha anteriorly as a guide to avoid injuring the skin.
After the elliptical exsection a linear incision with the scissors may be made both superiorly and inferiorly to further mobilize the springy shell of the ear, which will then be found to fall easily into place.
The bleeding in the latter method is more severe, since the posterior auricular arteries and the auricular branch of the occipital have to be severed, yet ligation is rarely necessary.
The interrupted suture may now be applied, varying the site of puncture as below or above its fellow puncture, as made necessary by the droop of the ear, with the object of shifting it into a normal position; or in other words, by raising or lowering it upon tightening the sutures.
The continuous suture is to be preferred, however, when the cartilage has been removed as described, since the ear has now become quite mobile and is easily placed in position.
When the removal of these sutures, which should be of Nos. 5 or 6 twisted silk, is considered, one can comprehend the advisability of this form of wound closure.
The ear will now appear to lie quite close to the head, compared with the original position, as shown in Figs. 141 and 142.
The patient is now turned so as to present the other ear, a pad of gauze and absorbent cotton being placed under the ear operated on for comfort’s sake.
The second ear is operated as was the first, the operator having taken note of the form and size of the incision of the ear just finished.
Both ears sutured, the wounds are cleansed thoroughly, though gently, with fifty-per-cent peroxid of hydrogen and dried and dusted over with aristol powder.
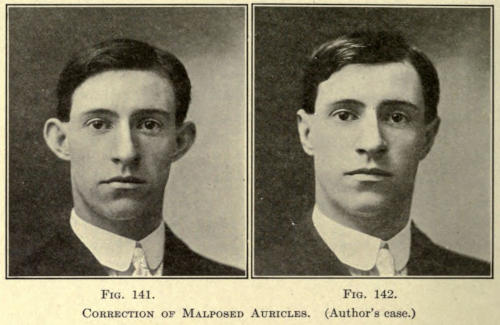
Fig. 141. Fig. 142.
Correction of Malposed Auricles. (Author’s case.)
A pad of gauze is placed over each ear and a bandage applied around the head to protect the wounds and retain the ears, care being taken not to tighten too tightly, as this occasions great pain and possible pressure erosion of the skin.
The dressing should be changed on the second day, as there is usually some soiling of the dressings at the lower angles of the wounds. They are again powdered, using the pulverflator preferably, and rebandaged.
The ears will be found to lie very close to the head at this time, if the operation has been properly done. Anteriorly in the skin of the concha and corresponding to the line of cartilage exsection will be found a crease more or less discolored, according to the severity of injury occasioned by the operation.
This should give the surgeon no concern, as the fold will accommodate itself in a few days. There may be a[143] persistence of the fold for some time, however, which, if desirable, can be corrected by a small secondary operation at a later date. The author has never experienced the need of such, however.
The patient at this time usually bemoans the position of his ears, and should be assured beforehand what was expected, and that the condition is only temporary.
The dressings after this can be repeated every second or third day, as may be required, although these wounds heal surprisingly well.
Moist dressings are to be avoided at all times, they soften the edges of the wound and prevent primary union.
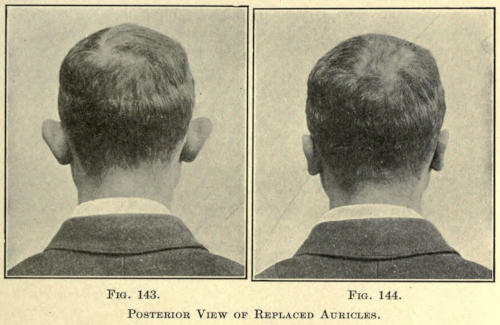
Fig. 143. Fig. 144.
Posterior View of Replaced Auricles.
The sutures are removed on the ninth or tenth day, whereafter the patient may be allowed to go without the head bandage, but is strictly instructed to replace it at night with a band of muslin three inches wide, snugly pinned around the head to prevent the ears from being injured or torn away from their new attachment by sudden movements during sleep. This bandage should be worn at night for at least a month.
When only a part of the ear is overprominent the operation undertaken should in the main be according to the methods just described, the incisions being changed in extent accordingly.
In the illustrations above, Figs. 143 and 144, are shown the posterior view of the ears before and after operation. At no time should the ears be placed too closely to the head, as is often peculiarly requested by the patient, as it gives an unnatural appearance and predisposes toward the collection of filth in the sulcuses that is hard to remove. The distance from the head to the outer rim of the ear should be about half an inch at its widest part.
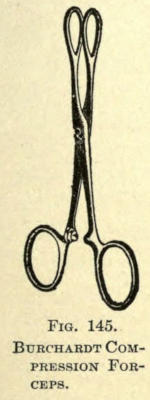
Fig. 145.
Burchardt Compression Forceps.
This branch of plastic surgery has to do with the correction of deformities of the lips. These deformities usually involve one lip only, and are dependent upon direct traumatism, operative interference in the extirpation of malignant growths, particularly carcinomata, the correction of cicatricial disfigurement following tubercular or syphilitic ulceration or congenital faults, commonly met with in harelip.
Operations for the latter condition have usually been considered under a separate heading, but since the restorative procedures involve methods purely plastic they are included under this their proper classification.
Owing to the great number of blood vessels in the lips, it is advisable to resort to the bloodless method, where the defect to be corrected involves more than the superficial structure. This is accomplished:
1. By compressing the coronary arteries at both angles of the mouth by digital pressure, suitable clamps or[146] compression forceps. The fenestrated oval forceps, illustrated in Fig. 145, and designed by Burchardt, or the harelip clamp of Beinl, Fig. 146, will be found to meet the purpose well, the latter having a sliding lock by which the pressure upon the tissue can be regulated to a nicety.
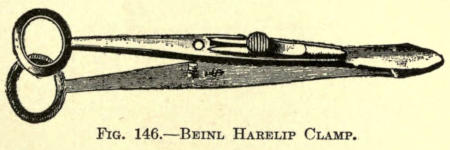
Fig. 146.—Beinl Harelip Clamp.
2. By clamping off the site of operation with specially made cutisector forceps. Its smooth parallel jaws should be curved outward, so that the diseased area can be fully excluded by their concavities.
3. By employing the indirect ligature of Langenbuch. This is accomplished by including the site of operation with several strong silk threads firmly tied in loops upon the skin surface, each loop including a given amount of tissue, the next encroaching upon it up to the center of this area, and so on until the entire site is rendered anemic. The advantage of this method is that with the anemia a certain amount of anesthesia is produced at the same time; a fact to be remembered when the patient is to be operated under local anesthesia, the anemia enhancing the efficacy of the latter.
A congenital defect of the upper lip caused by the lack of proper union of the maxillary, globular, and frontonasal processes in embryo. Treves states that from the buccal aspect of the maxillary process of either side the palatal processes arise, passing inward to combine with each other to form the soft palate and all of the hard palate, except the intermaxillary portion, and that from this same source are formed the cheeks, the outer or lateral parts of the upper lip, and the superior maxillary bones, while the external nose, the ethmoid, the vomer, the median portion of the upper lip, and the intermaxillary or os incisivum are derived from the frontonasal process.
The fact that these centers of development are concerned in the formation of the parts involving harelip accounts for the position of the cleft in the lip as being unilateral or bilateral, and rarely if ever median or intermaxillary.
Six varieties of harelip deformity are recognized by Rose, but herein only five classes of these will be considered, one of which, the first, is so rare that its occurrence is practically denied.
For all purposes in surgery of the face, in which cosmetic effects are sought, the author considers the following classification to answer fully:
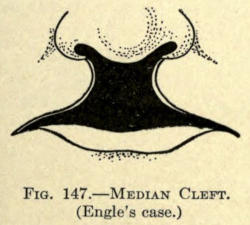
Fig. 147.—Median Cleft. (Engle’s case.)
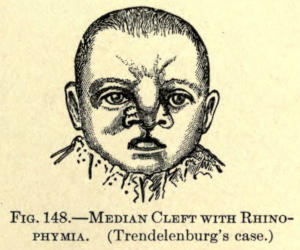
Fig. 148.—Median Cleft with Rhinophymia. (Trendelenburg’s case.)
1. Median or Intermaxillary Cleft.—As has been said, the first variety of this form of lip deformity is very rarely met with. It consists of a cleft in the median third of the upper lip, more rarely associated with the absence of the intermaxillary bone and total cleft of the hard and soft palate. In fact, the entire median section may be absent with or without absence of the intermaxillary and[148] vomer bones (Engle) (see Fig. 147). Commonly, however, the cleft involves only a part of the filtrum of the lip, although Witzel speaks of a case in which the lip assumed the form of a dog’s nose, the cleft extending upward, completely dividing the nares from one another, or the entire nose may be divided in its median line.
When the cleft involves the hard parts—that is, the intermaxillary bone and the hard palate—it is said to be total.
2. Single and Double Cleft.—The second variety in the above classification is by far the most common, and is often, therefore, termed ordinary. In this there exists either a unilateral or bilateral cleft of the lip of varying degree, depending upon the involvement of the tissue affected. It is not unusual to find fissures in these cases extending through the alveolar arch and the hard and soft palate.
This fissure or cleft is always found on one side of the median line, while in the soft palate it is median.
Most unilateral clefts of the lip will be found to be in the left outer third. They are more common in the male child.
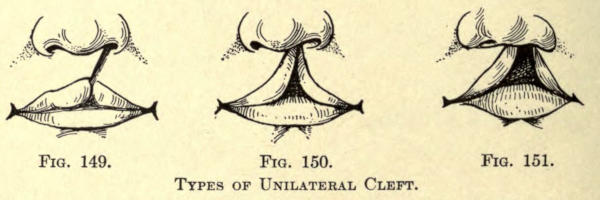
Fig. 149. Fig. 150. Fig. 151.
Types of Unilateral Cleft.
The degrees of deformity of the soft parts in the unilateral variety are shown in Figs. 149 to 151, respectively, representing the first, second, and third degrees of the cleft deformity, according to the involvement of the lip tissue. In first degree are included small notches in the prolabium only or extending upward somewhat above[149] its margin, but not involving the entire lip. In the second degree both the vermilion border and the lip are divided, while in the third degree the cleft extends into the nose with an absence of part of the lip structure itself.
Since the deformity in the division under discussion is so commonly met with it will be considered fully under its operative correction.
3. Facial Cleft.—The third class of deformity includes either unilateral or bilateral fissure of the face.
In the unilateral variety the cleft usually begins at the outer section of the upper lip, involving, as a rule, only the soft parts, extending upward and irregularly around the alæ of the nose to the inner canthus of the eye, or going even beyond the orbit and over the forehead as far as the hair line. An illustration of such a case is shown in Fig. 152.
The bilateral form of this facial defect is rarely met with. A case reported by von Guersant is shown in Fig. 153.
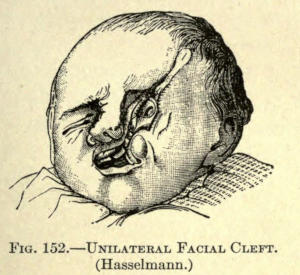
Fig. 152.—Unilateral Facial Cleft. (Hasselmann.)
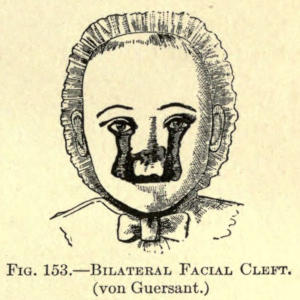
Fig. 153.—Bilateral Facial Cleft. (von Guersant.)
4. Buccal Cleft.—In the fourth variety the deformity involves the cheeks, the fissures extending from the angles of the mouth outward, causing an enlargement of this natural opening, and hence this defect is better known as macrostoma.
It may affect one or both cheeks. The latter is elucidated in Fig. 154.
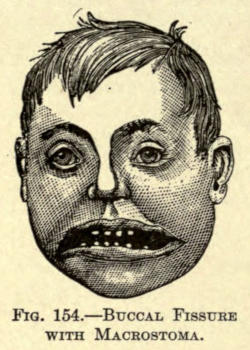
Fig. 154.—Buccal Fissure with Macrostoma.
On the other hand there may exist a congenital contraction of the mouth termed microstoma. This defect is rarely seen, and is due to a too free union of the maxillary and mandibular processes. When observed it is usually associated with improper development of the inferior maxillary bones.
5. Mandibular Cleft.—In the fifth class the cleft is to be found in the median line of the lower lip. This fissure, though extremely rare, may involve only the soft tissue or extend to the inferior maxillary (Thorndike) and even to the tongue (Wölfler).
From what has been said of the five varieties just mentioned it can be plainly seen that the defects of the second class are the most common. Since the correction of such involves methods of an extensive technique that can be followed more or less in the restoration of any of the above, this particular subdivision will be considered fully, but only to the extent of defects of the soft parts, leaving the osteoplastic and periosteoplastic operations to be studied elsewhere.
The defects that have to do with facial and buccal clefts will be more specifically mentioned later on under Melo- and Stomatoplasty.
The correction of a harelip should be undertaken as early as the first two weeks after birth in the healthy child. If, however, the infant is considered too delicate to undergo so early an ordeal, the operation should be deferred until the third or even the fifth month. At any[151] rate the operation should be undertaken as early as deemed advisable, since the closure of the cleft has a desirable effect upon the ofttime overprominent intermaxillary bone, helps to approximate its lateral borders, overcomes the later depression deformity of the upper lip, aids its natural development, and permits of the child suckling the breast—an important factor in the proper nourishment, since the defect allows only of feeding with the spoon, the child being unable to grasp the nipple of the breast in this state. Furthermore, the act of phonation is practically entirely perfected by an early operation, and rarely if ever overcome when faulty phonation has been established.
The restoration of an unilateral cleft is to be performed without the use of an anesthetic. The child’s arms are fastened to its sides with several turns of a wide roller bandage. It is then seated upon the lap of the assistant, who holds its head in position, compressing the coronary arteries with his fingers at the outer sections of the upper lip at the same time. If this is impractical, proper forceps can be employed, as already mentioned. It is rarely necessary to employ the direct-ligature method heretofore referred to in this class of operations. More or less bleeding always accompanies the operation, the child usually swallowing what enters the mouth if not sponged up repeatedly.
To facilitate matters the child can be anesthetized, chloroform being used. In this case the patient is to be placed on its side, the head being fixed in a dependent position (Rose).
This gives freer drainage of the bleeding surfaces, the blood being sponged up with gauze sponges as required, while the vessels that are cut can be tied off with catgut ligatures as fast as they are divided.
The anesthetic can be given upon a small sponge held[152] before the nostrils. Infants should not be anesthetized, yet in older children it is almost always necessary.
A simple freshening of the edges of the defect with the bistoury, followed by suture, does not give a desired cosmetic effect, hence it is advisable to resort to methods intended to restore the lip as far as possible to its normal state.
Nélaton Method.—The simplest operation for a cleft of moderate extent not involving the nare is that of Nélaton. He divides the lip above the angle parallel with the defect with a bistoury, cutting upward, including the upper angle which allows the prolabium surmounted by a thin strip of skin to droop downward in a point.
The lower angle of the wound is then drawn downward and united lengthwise with silkworm gut sutures, giving to the prolabium a protrusion or tip, which eventually retracts and causing the lip to assume a natural aspect.
The method is shown in Figs. 155-157.
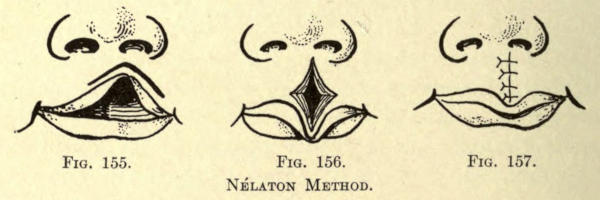
Fig. 155. Fig. 156. Fig. 157.
Nélaton Method.
Fillebrown Method.—Fillebrown has devised a method where the vermilion border of the lip is entirely preserved, as in the preceding operation. His method can only be employed where the cleft is not extensive. He commences his incision at the red border at the outer left line, cutting upward and inward toward the median line a short distance (see Fig. 158), then downward to the red border of the lip, then upward and outward to the right of the median line, corresponding to the incision just made to the left of the median line. The upper[153] angle of the cleft is now drawn down by its red border and the wound sutured, as shown in Fig. 159. This operation does not project a small triangle of the white skin into the vermilion border and gives excellent results.
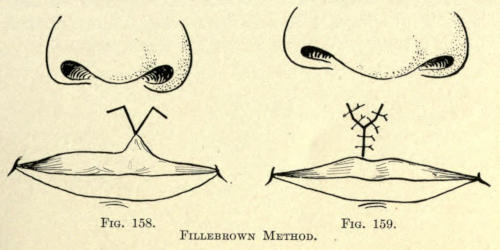
Fig. 158. Fig. 159.
Fillebrown Method.
Von Langenbeck, Wolff, and Sedillot Methods.—The methods of von Langenbeck, Wolff, and Sedillot are somewhat similar to that of Nélaton. An incision is made slightly above the prolabium, following the angle of distortion and reaching outward to either side of the median line almost to the angle of the mouth. The raw edges corresponding to the defect are brought together by suture and a section of the prolabium is removed to overcome its overprominence, but not enough to entirely flatten the vermilion border (see Figs. 160-161). The latter is sutured horizontally to such part of the angular defect as has not been utilized in the median line, and also[154] vertically as far down as its free border, as shown in Fig. 162.
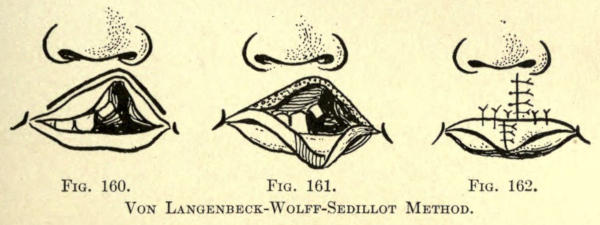
Fig. 160. Fig. 161. Fig. 162.
Von Langenbeck-Wolff-Sedillot Method.
Malgaigne Method.—The method of Malgaigne differs in technique in that he utilizes a semicircular incision, which is made to include the upper angle of the defect. Both ends of this incision are continued horizontally outward to a required extent (see Fig. 163). The freed prolabial flaps are drawn downward, as in Fig. 164, and sutured vertically, as shown in Fig. 165. Two retention sutures are shown in the latter figure to overcome the tension of the lips post operatio.
The semicircular incision should be preferred when the defect will permit it, since the unequal lengths of the two lip halves may thereby be more uniformly approximated, while the prolabium in being crowded downward overcomes the notchlike scar so common with the vertical-incision method.

Fig. 163. Fig. 164. Fig. 165.
Malgaigne Method.
Gräfe Method.—This method, as shown in Fig. 166, is, therefore, to be preferred when the defect is one of the first or second degree.
The first suture is to be placed at the margin of the vermilion border and the skin, so that the unequal sides are placed in normal apposition. The parts are sutured according to the method shown in Fig. 167.
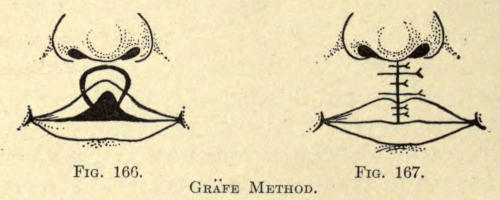
Fig. 166. Fig. 167.
Gräfe Method.
Mirault-Bruns Method.—An excellent method of this class is that of Mirault-Bruns. Their operation is indicated in defects of extensive degree, and usually gives excellent results. As in the former method a semicircular incision is made to include the superior angle, and two other incisions are made somewhat as shown in Fig. 168. The wound made thereby is shown in Fig. 169. The inferior triangular flap of one side is utilized to restore the prolabium, the whole being sutured, as shown in Fig. 170, care being taken to make this flap of sufficient size to give stability and volume to the lower margin of the lip.
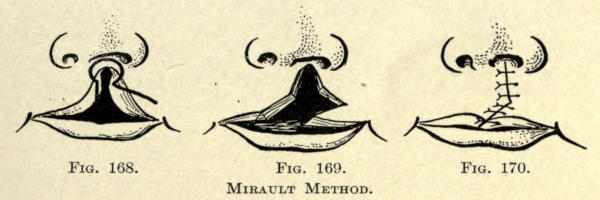
Fig. 168. Fig. 169. Fig. 170.
Mirault Method.
Giralde Method.—This method is intended for defects of the third degree. A vertical incision frees the vermilion border on one side, while an angular cut on the opposite side (see Fig. 171) allows of the bringing together the lip flaps above it. The wound is made to appear somewhat as in Fig. 172, and is sutured, as depicted in Fig. 173.

Fig. 171. Fig. 172. Fig. 173.
Giralde Method.
König Method.—König advocates two vertical incisions which dispose of the cicatrized borders of the defect. A slanting incision is added at both sides to free the prolabium (see Fig. 174), giving a wound when drawn in position, as shown in Fig. 175. In suturing the wound the vermilion border flaps are turned downward as much as possible to restore the contour of the prolabium. The sutures are placed as shown in Fig. 176.

Fig. 174. Fig. 175. Fig. 176.
König Method.
Maas Method.—Maas has deviated from the above method somewhat, as is shown in Fig. 177, by making one of the prolabial flaps much larger than the other. His operation is applicable to defects of maximum extent. The lip wounds are thereby made to appear as in Fig. 178, and the sutures are applied as in Fig. 179, with an advantage of leaving a smaller sutured wound to heal by primary union.
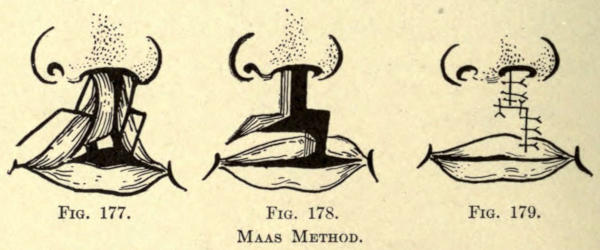
Fig. 177. Fig. 178. Fig. 179.
Maas Method.
Haagedorn Method.—Haagedorn’s method does not differ much from the above. The incisions are shown in Fig. 180, the appearance of the freed margins in Fig. 181, and[157] the sutured wound in Fig. 182. The prolabial flaps are somewhat alike in size in this operation, in which it differs only in the method just considered.

Fig. 180. Fig. 181. Fig. 182.
Haagedorn Method.
Geuzmer Method.—Geuzmer so incised the cicatrized defect that a small prolabial flap is formed from the median border and a larger one from the lateral, the very opposite of the Haagedorn technique.
Dieffenbach Method.—To facilitate the mobility of the lip flaps, Dieffenbach has added two additional incisions on either side of the nose, in circular fashion, encircling the alæ of the nose, as shown in Fig. 183. This procedure is hardly ever necessary in harelip, and truly applies to the restoration of a considerable loss of tissue of the upper lip occasioned by the extirpation of cancerous growths, although clefts of the median variety might be corrected thereby.
The wound thus formed appears as in Fig. 184. The sutures are placed as in Fig. 185.
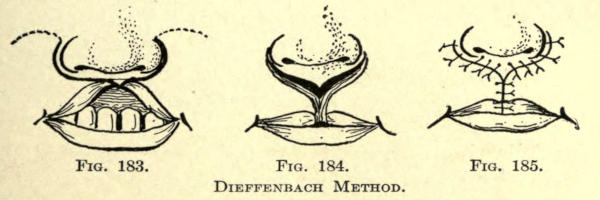
Fig. 183. Fig. 184. Fig. 185.
Dieffenbach Method.
Instead of the semicircular incisions a horizontal incision on either side of the cleft may be made just below[158] the nose with the same object in view, the wound being sutured in angular form similar to the method of Nélaton.
The occurrence of bilateral cleft of the lip is much rarer than the variety just described. According to Fahrenbach, out of 210 cases he found only 59 of some degree of the bilateral form.
The degrees of deformity have already been mentioned.
The correction of these types of fissure is very similar to that of the single cleft variety except that the operations for the latter are simply duplicated on the opposite side.
Particularly is this true in cases of the first degree, while in the severer forms, modifications of such methods as have been described must be resorted to, according to the nature and extent of the defect.
It must always be the object of the surgeon to save as much of the presenting tissues as is possible, to avoid traction on the tissues and to overcome the consequent thinning out of the entire upper lip or the flattening so often seen in the lips of these patients.
The correction of this flattening of the lip following operations for the restoration of the lip will be considered later.
The following operations for the correction of bilateral cleft may be regarded as fundamental:
Von Esmarch Method.—Von Esmarch advocates an incision circling the central peninsula just sufficient to remove the bordering cicatrix. Both lateral borders are vivified along the limit of the vermilion borders (see Fig. 186). He advises suturing the mucous-membrane flaps which he retroverts to form a basement membrane, upon this he slides the skin flaps, and sutures them as shown in Fig. 187.
The best results are obtained when the lip is sufficiently detached from the jaw by deep incisions beginning at the duplicature of the mucous membrane. This insures the necessary mobility, and is considered by him the most important step in the operation.
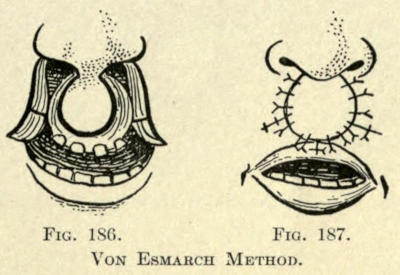
Fig. 186. Fig. 187.
Von Esmarch Method.
Maas and von Langenbeck Methods.—Maas and von Langenbeck vivify the median peninsula in square fashion, as shown in Fig. 188, and suture the fresh margins of the flaps, as shown in Fig. 189, according to Fig. 190.
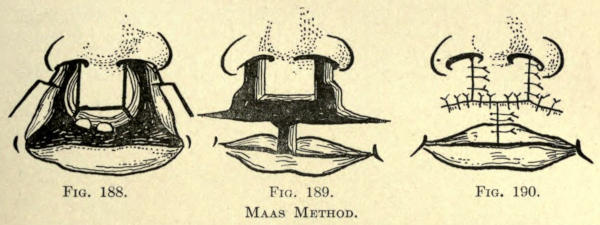
Fig. 188. Fig. 189. Fig. 190.
Maas Method.
Haagedorn Method.—Haagedorn’s method is very similar to the above except that in cutting square the inferior border of the median portion he fashions it into a triangular form, with the object of giving to the prolabium the tiplike prominence found in the normal lip, and also avoiding the cicatricial notch obtained with the direct suturing of the vermilion border on a line with its inferior limitation. The various steps of his method are shown in Figs. 191, 192, 193.
If there be considerable absence of lip tissue he advises making two lateral incisions sufficient to overcome the tension on the parts. These secondary wounds are allowed to heal by granulation.
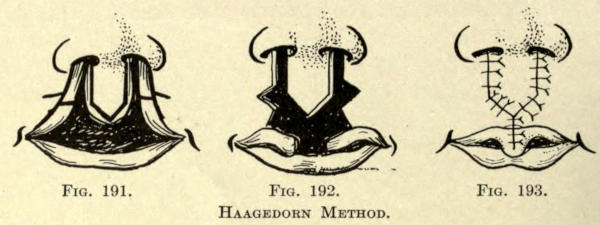
Fig. 191. Fig. 192. Fig. 193.
Haagedorn Method.
Simon Method.—Simon utilizes two curved lateral incisions encircling the alæ of the nose. This permits of a ready juxtaposition of the lateral flaps (see Fig. 194). The two flaps are sewn to the median flap (see Fig. 195) and are allowed to heal into place, the secondary wounds healing by granulation.
When this has been accomplished, a later operation is undertaken to correct the prolabial border, the incision for which and the disposition of the suture are shown in Fig. 196.
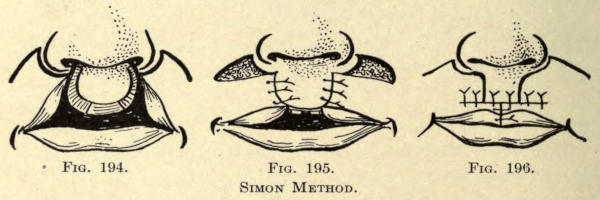
Fig. 194. Fig. 195. Fig. 196.
Simon Method.
This operation is useful only in older children, and has the disadvantage of requiring a secondary interference. The results are not as good as those obtained with the operations mentioned previously, leaving, besides, a disfiguring cicatrix at either border of the alæ, a serious objection, especially to the cosmetic surgeon.
When the operation has been performed in the infant the wound is simply kept clean by the local use of warm boric-acid solutions and the mouth is cleansed from time to time by wiping it out with a piece of gauze dipped into the solution.
Children do not bear dressings of any kind well, although Heath employs strips of adhesive plaster to draw the cheeks together to relieve tension on the sutures.
To keep the child from tearing or picking at the wound Littlewood advises fixing both elbows in the extended position with a few turns of a plaster-of-Paris bandage.
Everything should be done to keep the child quiet, as crying often results in separating the wounds. This is accomplished by giving it milk immediately after the operation. The mother must ply herself closely in soothing the child by carrying it about, rocking, and feeding it.
The feeding should be done with the spoon. Dark-colored stools containing swallowed blood will be passed in the first twenty-four hours; to facilitate this a mild laxative, such as sirup of rhei, can be given.
In older children a compressor can be applied to the head. That of Hainsley, shown in Fig. 197, answers very well, yet adhesive plaster dressings, if carefully removed later, are most commonly used.
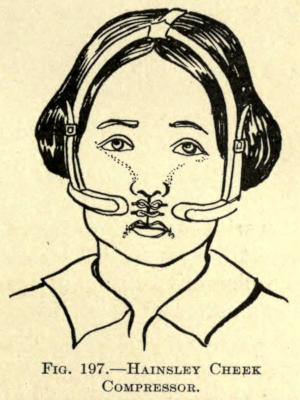
Fig. 197.—Hainsley Cheek Compressor.
The sutures may be removed as early as the sixth day,[162] but it is best to release the wound sutures about this time, and leave the tension sutures for two or three days later.
It often happens that the entire wound has not healed by primary union, if this occurs and sufficient union has taken place in part of the lip, the wound should be allowed to heal by granulation.
Should the entire wound separate on the removal of the sutures, the operator may attempt to secure healing of the wound by applying a secondary suture to bring the granulating surfaces together, although little is gained by this procedure as a rule.
If reoperation becomes necessary, it should not be undertaken before six weeks or more have elapsed. At any rate not before the lip tissues have returned to their normal state. Inflamed tissues do not retain sutures well.
It usually becomes necessary to perform small cosmetic operations after the healing of harelip wounds. Those should not be undertaken until the child is of such age as to insure a perfect result.
Plastic operations for the reconstruction of the upper lip are not met with often in surgery, except in connection with the various forms of harelip. When the latter is not the cause, deficiencies of the upper lip are due to the ulcerative forms of syphilis, and are occasioned by the ablation of epithelioma and carcinoma or the result of burns or lupus. Rarely the surgeon will meet with such a defect caused by dog bite or other traumatisms due to direct violence, as in railroad or automobile accidents.
Berger has classified three degrees of this deformity, according to its severity, to wit:
1. The skin only is destroyed and the mucosa remains.
2. The mucosa has been partially destroyed with the skin, but a part of the free border of the lip remains and is attached to the cicatrix.
3. All the parts which make up the lip have been destroyed, and there remains neither skin, mucosa, muscles, nor the prolabium.
The loss of substance of varying degree may involve either of the outer thirds or the median position of the lip, or its entire structure. For a more explicit classification the author divided these defects into:
(a) Unilateral defect of the first, second, or third degree.
(b) Bilateral defect of the first, second, or third degree.
(c) Median defect of the first, second, or third degree.
(d) Total loss of upper lip.
This same classification applies to the defects of the lower lip.
When the deformity is either of the first or second degree, one or the other of the operations for the restoration of congenital cleft just considered may be employed. When these are impracticable other methods must be resorted to.
Bruns Method.—Bruns advocates making two lateral flaps from the cheeks, as shown in Fig. 198. He preserves the inferior margin of these flaps, which contain a cicatricial border which must take the place of the prolabium. This border can, however, be made up of the vermilion border of the lower lip, as shown later in the performance of stomatoplasty, to establish a better cosmetic effect.
The rectangular cheek flaps are sutured, as in Fig. 199, leaving two small triangular wounds at either side of the alæ to heal by granulation.
The cheek flaps referred to must be dissected up from the bone, and be rendered as mobile as possible for a successful issue.
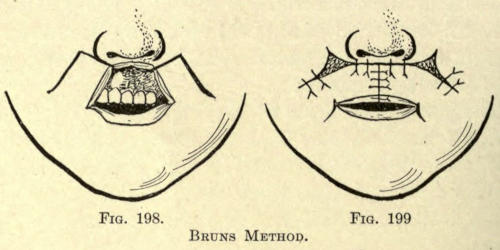
Fig. 198. Fig. 199.
Bruns Method.
Dieffenbach Method.—The method of Dieffenbach is very similar to the above. It has been described on page 157. In this the lateral flaps are made by two curved incisions encircling the alæ of the nose. Should these be insufficient, two other curved incisions are added, as shown by the dotted lines in Fig. 183.
Sedillot Method.—Sedillot also employs two rectangular flaps, but he cuts them from the region of the chin (see Fig. 200).
The advantage of this method lies in the fact that these flaps are lined throughout with mucous membrane, as the incisions are made entirely through the tissues involved, beginning at the angle of the mouth and extending[165] downward to the limitation of the buccal fold interiorly.
The flaps are twisted into position and sutured, as shown in Fig. 201. The mucous membrane of the inferior border is dissected up to a required extent and turned outward and stitched to the skin margin without to provide the prolabium. This is an important matter not only for cosmetic reasons, but especially because such mucous-membrane lining overcomes to a great degree the objectionable cicatricial contraction of this free border.
In certain cases the mucous-membrane grafts of Wölfler may be employed to cover the raw edge of these newly made lips, or the Thiersch method of skin-grafting might be employed with the same object.
Where the defect is unilateral, as is usually the case, a single cheek or chin flap need only be employed, and this lined with mucous membrane.
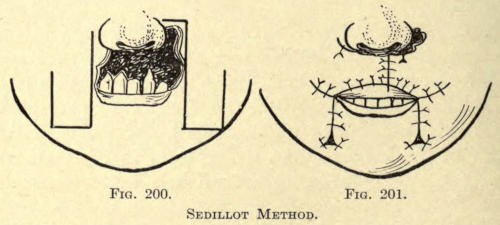
Fig. 200. Fig. 201.
Sedillot Method.
Buck Method.—Buck, in such unilateral defects, employs an interolateral rectangular flap. It contains a part of the lower lip and its vermilion border. This flap is twisted upward, so that its outer and free end comes in apposition at or near the median line as may be, with the remaining half of the upper lip.
This half of the lip is freely liberated by dividing the buccal mucous membrane along the reflecting fold. Should the vermilion border be contracted upward along the median cicatricial line it is carefully cut away from the lip proper down to its normal margin. This strip is retained until the flap taken from the under lip is brought into position, when it is neatly sutured to the prolabium thus brought into apposition. If there be a[166] redundancy of the freed prolabium after the median sutures have been applied it is cut away.
The secondary defect in the cheek caused by the rotation of the flap is closed by suturing the raw surfaces together.
The resulting mouth will be much smaller than normal, having a puckered appearance. A secondary operation, mentioned later, is employed to correct this.
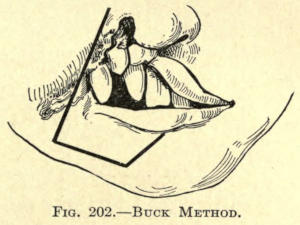
Fig. 202.—Buck Method.
Estlander-Abbé Method.—Estlander and Abbé employed a transplantation flap of triangular form taken from the lower lip to restore median defects of the upper lip, whether due to a deficiency of the latter following harelip operation or the extirpation of a malignant growth.
Where the tissues operated upon warrant such procedure this operation will give excellent results, leaving the mouth almost normal in shape and size.
The lower pedunculated flap is made by cutting directly through the entire thickness of the lip, including the prolabium at A (Fig. 203), and downward toward the median line to the point B, thence upward to the margin of the vermilion border at G, leaving the latter to form the pedicle of the flap F. The defect is freshened by either a median incision, D, E, or the ablation is made in triangular form.
The flap F is now rotated upward and sutured into the upper lip, as shown in Fig. 204. The triangular defect thus made in the lower lip is sutured along the median line.
The prolabial pedicle of the flap F is not divided until about the eighth day, when the vermilion borders of both the upper and lower lips are restored by the aid of the free stump ends, which are neatly sutured into position, as shown in Fig. 205.
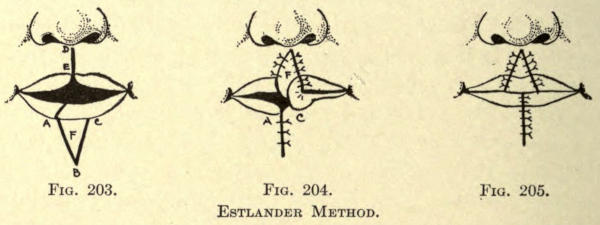
Fig. 203. Fig. 204. Fig. 205.
Estlander Method.
This operation may also be used in the unilateral type of defect. It will be described in the operation of the lower lip, where it is more frequently employed than in connection with faults of the upper lip.
Apart from harelip operation, those for the separation of the lower lip are the most common about the mouth. This is due in a great measure to the fact that malignant growths so frequently attack this part of the human economy and almost exclusively in the male. Out of sixty-one cases von Winiwarter found only one female thus affected. It has not been determined whether the habit of pipe smoking has been a factor in establishing this unequal proportion, yet it is acceded to be the fact, so much so that neoplasms of the lip in men have been commonly termed smoker’s cancer.
The ulcerative forms of syphilis and tuberculosis seem to be met with more in the lower than in the upper lip; likewise is this true of burns and acute traumatisms.
Defects in the lower lip are, therefore, due principally to the extirpation of carcinomata or other malignant growths and less frequently to the other causes mentioned.
The classification and extent of such involvement has already been referred to.
In operations intended to extirpate a growth of malignant nature the incisions should be made sufficiently distant from the neoplasm to insure of unaffected or uninvolved tissue to avoid a recurrence of the disease.
These growths appear at first in wartlike formation,[168] becoming thicker in time, and bleeding readily upon interference. They seem to develop horizontally, and invariably in a direction toward the angle of the mouth. There is more or less involvement of the lymphatic glands, especially of the submaxillary, quite early in the attack.
An early extirpation of such growths is to be recommended, and while it is true there may be a question of primary syphilitic induration instead of the malignant variety no harm is done if the diseased area be at once excised.
This is especially true of patients beyond the thirtieth year. When such indurations occur before that age the patient may be put under a proper course of treatment to determine the nature of the infiltration for a period of three or four weeks; if this does not resolve it operative measures should be resorted to. It is to be remembered that syphilitic induration may involve the upper as frequently as the lower lip, a fact not as likely referable to cancer.
In sixty-seven cases reported from Billroth’s Clinic there were sixty-five cases of carcinoma of the lower lip and only two of the upper. Yet this proportion hardly applies to the experience of most surgeons. The age factor is not to be overlooked.
The author does not mean to claim that the differential diagnosis of these diseases is at all difficult, yet in patients beyond the admissible age early and radical treatment should not be neglected, considering what great amount of misery and suffering, not to mention disfigurement, can be overcome by prompt action.
Usually these neoplasms, when superficial, are found directly in the prolabium, are unilateral, and occupy a place midway between the angle of the mouth and the median line of the lip.
Richerand Method.—Very small or superficial neoplasms may be removed by lifting up the growth with a fixation forceps and cutting away the convexity so established as[169] deeply as necessary with the half-round scissors, or the faulty area is neatly outlined in spindle form (Richerand) with the bistoury, as in Fig. 206, and then excised according to the method selected by the operator.
The wound is sutured horizontally, as shown in Fig. 207.
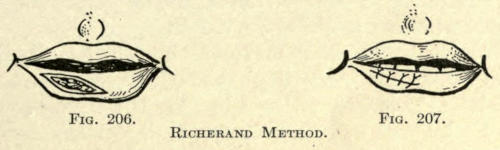
Fig. 206. Fig. 207.
Richerand Method.
If the neoplasm or defect is of a more extensive form, involving most or all of the prolabium, the entire area, including the necessary allowance of healthy structure, may be raised up by a clamp, as shown in Fig. 208, and excised. The mucous membrane from the anterior surface of the lip is then brought forward and sutured to the skin margin, as in Fig. 209. The disfigurement in this operation is surprisingly little, and the mucous membrane thus everted takes on the appearance of the vermilion border of the lip in a short time.
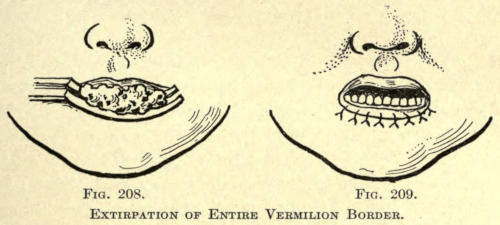
Fig. 208. Fig. 209.
Extirpation of Entire Vermilion Border.
Celsus Method.—When the neoplasm has become more than superficial, or the defect or deformity involves more than the prolabium, it must be ablated by a wedge-shaped incision, the base upward including the vermilion border[170] and the apex extending downward upon the anterior chin.
This is best performed by piercing the tissue with a sharp bistoury, the blade penetrating the mucosa, while an assistant compresses the coronary vessels with his fingers at either angle of the mouth.
The incision must be made well into the healthy tissue, or at least 1 cm. from the boundary of the defect. The incision is made, as outlined in Fig. 210, from below upward while the operator draws up the triangular mass to be removed with the fingers of his left hand. The same method is followed on the other side. The wound margins are then to be examined microscopically for any sign of malignant involvement. If there be any it should at once be removed, irrespective of the size of the wound occasioned thereby. For this reason the area excised may be so large as to prevent the ready apposition of the raw edges. Should this occur, the lip halves may be made more mobile by adding a horizontal incision continuous from the angle of the mouth outward and over the cheek, as shown in the line A, C.
A single incision for a unilateral defect and one on either side for a median excision, as shown by the lines A, C, and B, C, in the same figure.
This operation is known as the Celsus method. The parts are brought together and the sutures placed as in Fig. 211, beginning the first deeply and nearly to the mucous membrane, just below the prolabial margin,[171] which controls the bleeding. One or two of the sutures should be made deeply to overcome the tension of the parts as far as possible.
A few fine stitches are taken in the vermilion part of the lip and several in the mucous membrane to permit of close apposition and to insure primary union. Wounds of the lips heal very well, and the defects occasioned by even extension operations which involve as much as one half of the lip soon lose their acute hideous appearance.
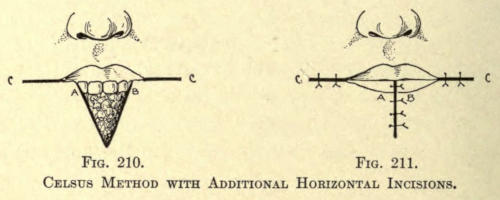
Fig. 210. Fig. 211.
Celsus Method with Additional Horizontal Incisions.
Estlander Method.—Estlander corrects a unilateral defect by excising the neoplasm in triangular fashion, and cutting out a triangular flap from the upper and outer third of the upper lip, leaving, however, the prolabium intact, which answers for the pedicle (see Fig. 212).
This triangular flap is rotated downward, and is sutured into the opening in the lower lip, as shown in Fig. 213.
Where this method can be employed it does very well, as it overcomes the secondary defect so common with most of these operations, while a small operation may be undertaken later to correct the mouth formation if necessary.
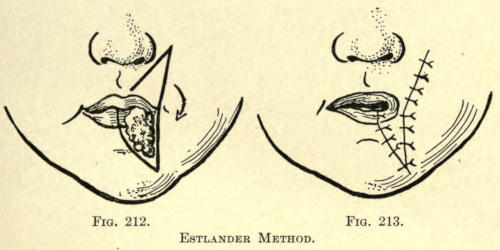
Fig. 212. Fig. 213.
Estlander Method.
Bruns Method.—Bruns removes the defect in quadrilateral form when the disease involves one half or more of[172] the lower lip, as shown in Fig. 214. He encircles the mouth by two curved incisions to aid in mobilizing the edges of the wound, which he sutures, as shown in Fig. 215, leaving two crescentic wounds at either side of the mouth, which are allowed to heal by granulation.
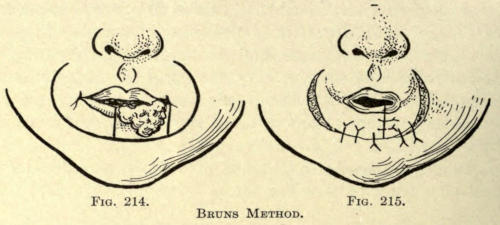
Fig. 214. Fig. 215.
Bruns Method.
Buck Method.—Buck has corrected a unilateral defect by employing the wedge-shaped incision, as shown by B, C, D in Fig. 216. After removing the triangular infected area he detaches the remaining half of the lip from the jaw as low down as its inferior border and as far back as the last molar tooth. A division of the buccal mucous membrane along the same line more readily permits of sliding the remains of the lip over to meet the raw surface opposite.
If the latter was not possible he obtained additional tissue by making a transverse incision from the angle of the mouth across the cheek to the point A, or within a fingers breadth of the muscle. A second incision is made downward from A and a little forward to the point E. This quadrilateral flap thus formed, with its upper half lined with mucous membrane is dissected up from the jaw except at its lower extremity. It is glided forward edgewise to meet the remaining half of the lip, where it is sutured into place, as shown in Fig. 217.
To cover the triangular raw space occasioned by the sliding forward of the flap A, B, C, E, another transverse incision is made through the skin continuing the line A, D, Fig. 217, to the extent of one inch. The skin is then dissected up as far as this incision will allow and is stretched forward until the edge meets the outer skin margin of the quadrilateral flap, to which it is sutured. A later operation for the restoration of the mouth has to be made.
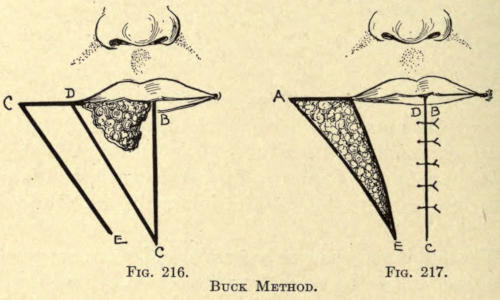
Fig. 216. Fig. 217.
Buck Method.
Dieffenbach Method.—Dieffenbach’s method is very similar to the above, but is applicable only to cases where the entire lower lip is involved and is extirpated (see Fig. 218). The wound is sutured as in Fig. 219. The secondary wounds are either sutured as in Buck’s method or they are covered immediately by Thiersch grafts (author’s method).
Dieffenbach allowed these secondary wounds to heal by granulation.
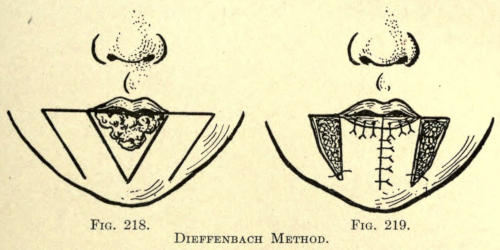
Fig. 218. Fig. 219.
Dieffenbach Method.
Jäsche Method.—Jäsche’s method is to be preferred to that of the foregoing author. After a cuneiform excision of the defect he adds two curved incisions extending downward at either side to insure mobility of the parts, as shown in Fig. 220.
In bringing the wound together, as shown in Fig. 221, he overcomes the large secondary defects of the operation last considered by suturing the skin margins.
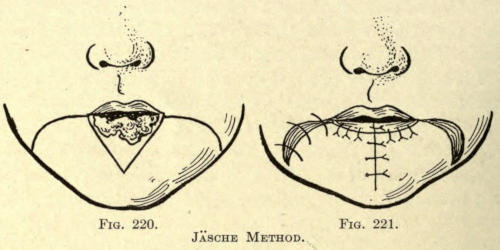
Fig. 220. Fig. 221.
Jäsche Method.
Trendelenburg Method.—Trendelenburg has modified the method of Jäsche by shortening the curve of the cheek incisions so that their outer borders were made to lie anterior to the facial artery (see Fig. 222), the[175] parts being approximated and sutured, as shown in Fig. 223.
To obtain sufficient mucous membrane to cover the superior margin of the two flaps when brought together he made the cheek incision only down to the mucosa, dissected up the latter a short distance from the upper part of the cheek, and divided it about one half centimetre above the line of the external incision. This flap of mucous membrane on either side was used to line the lip in place of the prolabium.
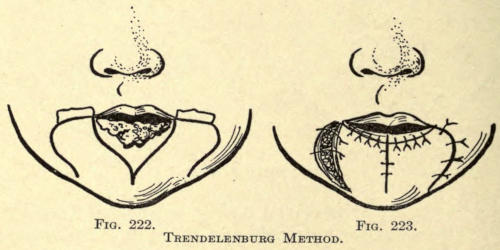
Fig. 222. Fig. 223.
Trendelenburg Method.
Bruns Method.—Bruns excises the defect when not involving the whole lip in quadrilateral form, and takes up a flap from the anterior region of the chin to cover it, as shown in Fig. 224.
This flap is rotated upward into the wound made, and is sutured in place, as shown in Fig. 225. The secondary wound is brought together by suture.
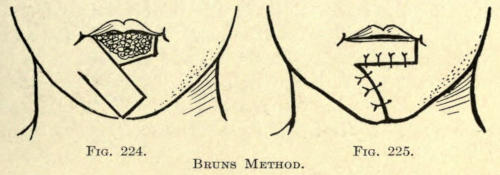
Fig. 224. Fig. 225.
Bruns Method.
In cases where the entire lip is removed he cuts two[176] square flaps from the upper anterior region of the cheeks extending as far upward as the alæ of the nose (see Fig. 226).
He rotates these flaps into the open wounds and sutures them into place, as shown in Fig. 227.
The border of the lip is lined with the mucous membrane of the cheek flaps then brought down. If the latter has become too stretched longitudinally, he relieves it at its base by transverse incisions.
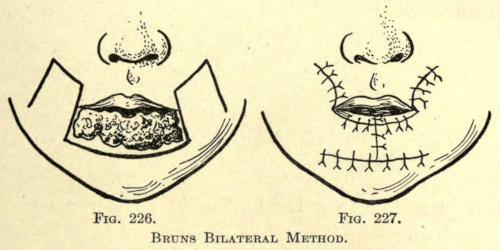
Fig. 226. Fig. 227.
Bruns Bilateral Method.
Buchanan Method.—Buchanan’s method consists of removing the diseased area by an elliptical incision A, B, A. A second oblique incision B, C, and a third of the same obliquity B, C, is made downward and outward upon the anterior chin. From the points C, C, two curved incisions parallel to the upper incision A, B, A, and equal to their lengths, are made to the points D, D, as shown in Fig. 228.
The latter incisions provide two flaps, as shown in Fig. 229. They are dissected off from their attachment to the lower jaw and raised upward so that their upper line B is raised on a level with the former margin of the lip A, A.
The oblique margins C, B, C are thus brought together vertically and sutured in the median line. The mucous membrane is brought from within outward and stitched to the skin margin.
The operation leaves two triangular wounds, which[177] are to be healed by granulation. The result of the rotation and apposition of the flaps is shown in Fig. 230.
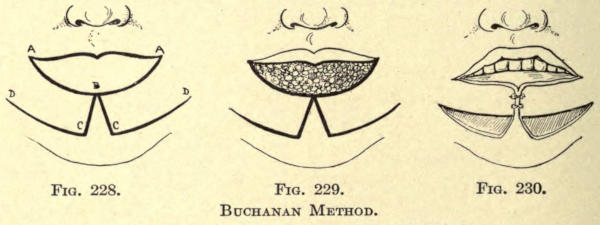
Fig. 228. Fig. 229. Fig. 230.
Buchanan Method.
Syme Method.—Syme removes the affected area in triangular fashion, and from the apex of the wounds carries two curved and sweeping incisions downward from the anterior chin and beneath, terminating at the angles of the jaw (see Fig. 231).
These two large flaps are dissected from their attachment to the jaw and are slid upward until the sides of the triangular wound are raised to a horizontal line corresponding to the superior border of the lower lip, when the flaps are sutured vertically upon the anterior chin and to the triangular island of undisturbed tissue underneath the chin, as shown in Fig. 232.
The advantage of this operation is that no secondary wounds are left to granulate, the whole healing by primary union.
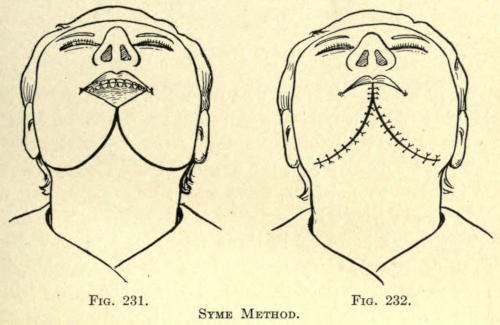
Fig. 231. Fig. 232.
Syme Method.
Blasius Method.—The method of Blasius is very similar to the foregoing, except that this author does not carry his two curved incisions as far downward and backward (see Fig. 233).
The two semilunar flaps are made from the tissue of[178] the anterior chin and slid upward, and sutured in the median line and to the intermedian spur of undisturbed tissue, as in Fig. 234.
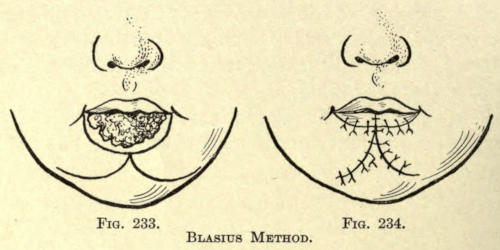
Fig. 233. Fig. 234.
Blasius Method.
Bürow Method.—Bürow, who favors the excisions of two triangles of healthy tissue in restoring an entire loss of the lower lip, proceeds by ablating the diseased area in triangular form. From the angles of the mouth he cuts two transverse incisions, upon which he outlines two triangles, as in Fig. 235.
The tissue included in these triangles is removed entirely, an unnecessary loss and one unwarrantable, but he saves the mucosa of these excised portions with which he lines the upper margin of the newly formed lip.
The freed lateral chin flaps he slides forward so that their oblique borders meet vertically in the median line, where they are sutured.
The triangular wounds in the cheeks are by this sliding process obliterated, and their raw edges are sutured vertically, as shown in Fig. 236.
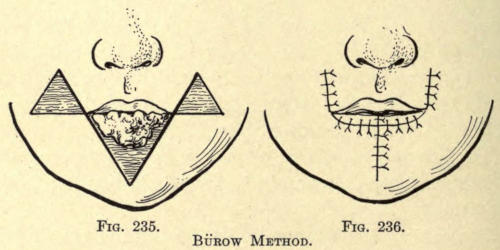
Fig. 235. Fig. 236.
Bürow Method.
Von Langenbeck Method.—Von Langenbeck, contrary to the double-flap methods, uses only one flap, with a lateral pedicle from the anterior chin.
After a semilunar excision of the diseased area, he cuts obliquely downward upon the anterior chin, then rounds his incision and continues it along, just above the margin of the chin, gradually cutting upward until its extremity is obliquely opposite to the angle of the mouth, as in Fig. 237.
The flap thus formed will be seen to have a pedicle at this point. It is dissected away from its mucous attachment and is rotated upward, jumping it over the triangular spur, which has also been mobilized by a sliding dissection.
The flap is sutured into position, as shown in Fig. 238. Unfortunately, the flap does not permit of lining the raw margin of the wound with mucous membrane turned outward from within, hence it is best to take sufficient of the mucous membrane from the cheeks to accomplish this, or the vermilion border of the upper lip may be carefully cut away from the lip at its outer sections just above the prolabial line, and elongated by stretching upon the raw surface of the under lip, to which it is sutured.
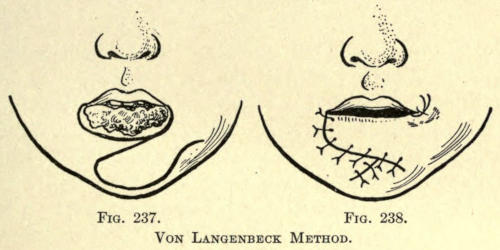
Fig. 237. Fig. 238.
Von Langenbeck Method.
Morgan Method.—For an extensive loss of the lower lip Morgan operates in the following manner:
After a thorough elliptical extirpation of the diseased area, he makes a curved incision in the tissue under the chin, conforming in its curvature to the incision made below the diseased area of the lip (see Fig. 239). The length of this incision is about twelve centimeters.
This bridging flap is carefully dissected up from its basement membrane. Any infected glandular tissue encountered in the meantime is removed thoroughly.
The whole bridge of tissue is now crowded upward, until it displaces the defect in the lip. It is sutured on either side, as shown in Fig. 240, to hold it in position.
Several sutures are introduced along its inferior margin, to tie it to the tissue of the anterior jaw border and to prevent its sliding downward.
Strips of borated gauze are laid into the fold between the raw surface of the flap and the jaw.
The secondary elliptical submental wound is drawn together by suture as far as possible; the remaining raw surface is either allowed to heal by granulation or is covered immediately with Thiersch grafts (Wölfler, Regnier).
The objection experienced with the method just considered is found in the difficulty with which the bridge[181] flap is carried upward over the prominence of the jawbone. It is very essential, therefore, to give as much freeness to this flap as possible, a fact necessitating considerable injury to the flap by handling and cutting, although the result of the operation, if carefully done, is excellent; the lip, owing to its solid form and undisturbed mucous membrane, does not contract as readily as with the average lip operation, and consequent ectropion is overcome to a great extent.
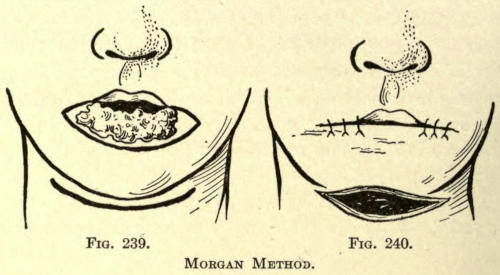
Fig. 239. Fig. 240.
Morgan Method.
Zeis Method.—To overcome the difficulty of sliding this bridgelike flap, Zeis advocates ablating the diseased area in quadrilateral form and forming the lip of unbroken tissue by making the flap two-tailed (see Fig. 241), each flap meeting anteriorly in a bridge of tissue sufficiently wide to permit of the formation of the required lower lip and extending obliquely downward and backward upon the submental surface, having their pedicles as far back and upon the neck as is necessary to allow the two-tailed flap to move forward into position.
The parts are slid into position and sutured, as shown in Fig. 242.
Unfortunately the tissue of the neck is not very thick, nor is it well nourished, factors that do not make it very satisfactory for cheiloplastic purposes.
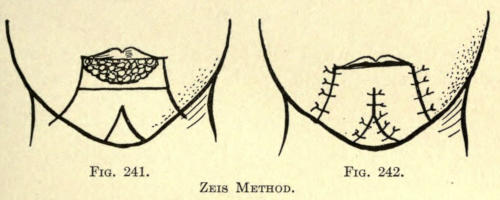
Fig. 241. Fig. 242.
Zeis Method.
Delpech Method.—Delpech has utilized the skin of the anterior neck region in the following manner: He ablates the extensive diseased area, as shown in Fig. 243, and dissects up an inverted triangular pedunculated flap of[182] skin from the hyoidean region of the neck, having its raw surfaces brought face to face at its distal extremity sufficiently to line the newly formed lip with skin which eventually would take on the function of mucous membrane.
The whole flap was now rotated upward on an arc of 180° and sutured into the labial defect, as shown in Fig. 244.
The large wound of the neck was readily drawn together by suture, leaving only a small triangular space to heal by granulation.
As has been mentioned, the skin of the neck is not adaptable for this purpose, not only because of its poor nourishment and extreme thinness, but because a flap made therefrom is devoid of muscular structure, contracts easily, and is devoid of a mucous-membrane prolabium, the greatest objection being in the resultant contraction of the lip so formed, which usually constitutes so high a degree of ectropion of the lip as to allow the saliva to escape from the mouth.
Apart from the ingenuity of the method it has no practical value, for the reasons given.
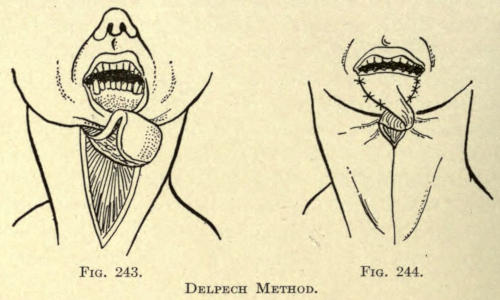
Fig. 243. Fig. 244.
Delpech Method.
Larger Method.—Larger restores two thirds of the lower lip after the ablation of an epithelioma, as follows:
1. An incision is made from the union of the left third[183] with the right two thirds of the upper lip, directed toward the alæ of the nose and including the entire thickness of the lip, the cul-de-sac, and the buccal mucous membrane.
2. A second incision is made from the upper extremity of the first incision downward from the nasolabial fold to a point on the cheek a little below and to the left of the left labial commissure. The flap being turned down, is sutured by its three edges to the lip of the quadrangular breach, after the lower edges of the flap has been freshened; this border being formed by the mucous membrane of the upper lip, the membrane is destroyed in order to permit of the edge being sutured to the horizontal branch of the loss of substance. The upper lip is then sutured vertically to the cheek.
Guinard Method.—Guinard modifies the above method by making the operation bilateral and symmetrical instead of unilateral, thus giving marked facial symmetry; the mucous membrane forming the free edge of the upper lip, instead of being destroyed, is dissected, turned over, and is sutured in a groove in front of the maxillary in such a way as to reconstitute the buccal vestibule; the mucous membrane of the deep surface of the lip is sutured to the skin by eversion in order to form a new mucous border.
With the above modification of the Larger method a considerable loss of substance can be restored, the new lip being constructed of normal tissue of the lip lined with mucous membrane retaining the saliva. Naturally the secondary deformity, while great, is one that only changes the physiognomy, leaving the face symmetrical with slight cicatrices.
Berger Method.—Berger advocates replacing a large loss of skin from the lower lip, the result of burns, lupus, or syphilitic ulceration, by employing a pedunculated flap made from the arm.
The free borders of the flap are sutured into the[184] defect and the arm is bandaged to the head in the proper position. The pedicle on the arm is not divided until the flap has become thoroughly reunited, which is at the end of eight to twelve days.
He dissects up and divides the free border of the mucosa until it is free from its attachments to fibers of the orbicularis muscle. This he utilizes in lining the flap.
The flap taken from the arm may be made large enough to cover the entire anterior aspect of the chin.
When the mucosa has been destroyed partially he advises releasing whatever remains of the mucous membrane, either as it may be, and loosening it so as to inclose the buccal orifice. He slides a flap taken from the subhyoid region to reconstruct the lip over this, or resorts to the Italian method just described.
Where the lip structure has become flattened and thinned as a result of tension following the exsection of a part of the lip, as in harelip, or the ablation of malignant growths, operations may be undertaken to give the tissue a better cosmetic appearance.
Estlander’s operation, described on page 171, gives, perhaps, the best results in these cases, but the objection to this procedure to make up the deficiency in the other, and often necessitating a later stomatoplasty to overcome the oval shortening occasioned by the rearrangement of the prolabium. This, of course, is a matter of little consequence where the primary fault is due to the ulcerative inroads of syphilis or the cicatricial contraction following burns. At any rate, the triangular flap implantation method is to be preferred to any other cutting procedure.
In simple cases where a triangular ablation has caused the flattening the defect can be overcome to a[185] great extent by employing the subcutaneous method of Gersuny.
Author’s Method.—The author recommends a subcutaneous division of the scar line in cases permitting such procedure prior to the injection of the tissues. This is accomplished with a fine tenotome, which requires only the making of a small opening in the skin through which the filling can be introduced. A single suture may be made through the lips of the wound, which is tied immediately after the filling has been introduced to avoid the displacement or pressing out of the injected mass at this point, which is sure to result if the suture be introduced after the injection.
A secondary filling may be found to be necessary subsequently to obtain the desired cosmetic result. The process of subcutaneous filling is fully considered in Chapter XIV.
When the lower lip is extremely flattened by the tension of cicatricial contraction of burn wounds of the mental region with more or less ectropion of the lip.
Teale Method.—Teale advocates the following method:
Two cheek flaps are formed by making a curved outward and upward incision upon either cheek, terminating at the second molar tooth of the upper jaw and corresponding to the lines A, A, in Fig. 245. These terminate anteriorly in two vertical incisions about three quarters of an inch long, made through the entire lip structure down to the bone on a line with the canine teeth.
The upper extremity of the two vertical incisions are united with a horizontal incision through the thinned-out or everted prolabium.
The two cheek flaps are dissected off from the bone, the mucous membrane uniting them to the alocoli being freely divided.
A base surface is made along the alocolar border of the median portion of the lip between the upper extremities of the two vertical incisions first made.
The flaps A, A are then brought together so that their vertical margins meet at the median line, where they are sutured. A few fine sutures are taken through the vermilion border.
A secondary wound, C, C, at either side is thus occasioned (Fig. 246), which can at once be covered with Thiersch grafts or is allowed to heal by granulation.
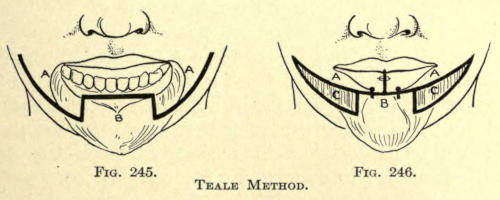
Fig. 245. Fig. 246.
Teale Method.
Where the deficiency is due to cicatricial contractions of the submental tissue the latter must be divided horizontally from one healthy border to the other, the parts freed well from all subcutaneous adhesions in the cellular structure. The head should be forcibly raised and a flap of skin be placed into the elliptical wound thus formed either by the rotation of a pedunculated neck or thorax skin flap or the implantation of Wölfler or Thiersch grafts.
Carefully keeping the head in an extended position during the healing in of these grafts will overcome the primary defect, unless the lip itself, too, has become tied down, when the bridge flap method of Morgan or Zeis can be undertaken in conjunction with the skin-grafting method to correct the fault.
Eversion of the lip may be due to cicatricial contraction of ulcerative wounds, burns, and traumatisms of the skin, or it may be hereditary. In the latter case the[187] entire lip structure is more or less overdeveloped, as in the negro, especially in the lower lip, so that the thickened lip droops forward and downward. This condition is termed macrocheila.
Ectropion of the lower lip is more common than in the upper lip. The defect may be slight and only of cosmetic importance or it may be so extensive as to permit an overflow of the saliva from the mouth.
When the cause of deformity is due to a cicatrix of the skin, as often met with in the lower lip, a flap should be neatly raised by a V incision, as with ectropium of the lower lid on page 104, and the wound sewed in the Y form (Dieffenbach).
In cases of severer form the cicatrix is removed by an elliptical incision, the lip returned to its natural position, and a pedunculated flap of skin is taken up from the chin or the cheek which is rotated into the wound, or a skin graft is implanted into the area by the Wölfler method and sutured to the free margins of the skin, or the Thiersch method may be employed.
In hereditary cases of mild form or partial ectropion the author advocates making two vertical incisions in the mucous membrane, half an inch long, one half inch distant from the median line of the lip, and suturing them horizontally, as shown in Figs. 247 and 248.
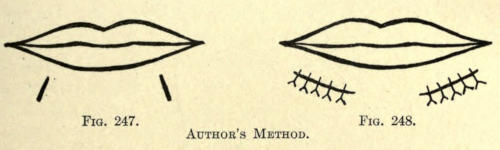
Fig. 247. Fig. 248.
Author’s Method.
In some cases the ectropion, whether partial or more or less general, is caused by protrusion of the teeth either of the upper or lower jaw; more commonly of the alveolar structure of the superior maxillary bone. In such cases a cosmetic operation on the mucosa will do[188] little to restore the deformity. Such cases should be corrected primarily by a surgeon dentist, the teeth being forced back into place by proper metal springs or splints—a tedious process requiring from six months to two years’ time.
If, after the teeth have been brought back to the normal bite, the lip still shows an abnormal contour, the surgeon may restore this by several small incisions in the mucosa, as above advised, at the various protruding points of the lip.
When the simple vertical-line incisions sutured horizontally will not accomplish the result, the excision of small triangles or elliptical pieces of the mucosa may be made, bringing the distal edges of the wounds together horizontally with silk sutures, which are found best for suturing wounds about the buccal cavity.
The same methods as above given apply to the correction of upper-lip deformities.
Where the fault is too great to be overcome by this method, the author advocates removing an elliptical or diamond-shaped piece of the lip from the inner surface or mucosa, the whole length of the lip and wide enough to correct the fault, as shown in Fig. 249, and bringing together the margins by an interrupted suture, as in Fig. 250. This is the most satisfactory method to restore[189] either the upper or lower lip to normal position. The resulting cicatrix of the mucous membrane offers no objection whatever, and soon becomes obliterated.
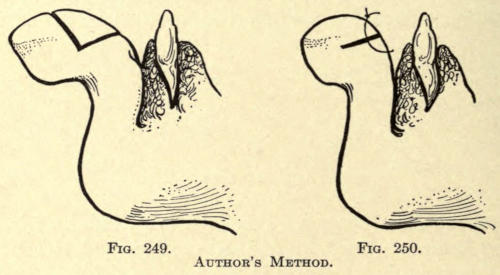
Fig. 249. Fig. 250.
Author’s Method.
If the operator feels justified to remove a triangular piece, with its base upward, in case of the lower lip, and vice versa, from the whole thickness of the lip he can do so, but the operation has the objection of leaving a noticeable vertical scar in the skin and a notch in the vermilion border.
The former can of course be materially hidden by the mustache or beard in man.
While labial inversion is in most cases caused by the removal of tissue from the inner or whole lip structure due to disease or other causes, it may nevertheless be met with in hereditary instances. The condition is termed microcheila.
It is more common in the upper lip, perhaps because of the frequency of harelip corrections undertaken with that part of the mouth, but it may involve both lips or be partial in one or both lips; in the latter case often the result of the habit of talking, chewing, or laughing with one side of the mouth, in which the active side is the normal and the passive side the one showing a lack of development.
In the latter case daily facial gymnastics should be advised, and such teeth as need attention to permit of the use of the side favored should be restored to usefulness—the loss or uselessness of teeth in the earlier days of puberty often causing the deformity. The correction of such defect has in view to widen the lip structure, and the best method to follow is the suturing of one or more horizontal incisions in a vertical direction, these incisions depending in number upon the extent of the lack of tissue, whether total or partial. This, of[190] course, overcomes only the rolling in of the vermilion border, and does not in cases of the extensive variety overcome the deformity. In such cases an incision is made through and along the entire mucosa half an inch below the vermilion border. The incision should be made deep enough to permit of free movement of the upper section of the lip, which is drawn up by an assistant, while a flap of mucosa, either pedunculated or free and taken from the inner side of the cheek in the near vicinity to the lip, is sutured into the opening thus made by traction.
If a pedunculated flap is employed, it should be cut in such a way that the twisting or rotation of its pedicle will not be too abrupt, and thus cause gangrene.
The secondary wound is sutured with silk and heals quite readily under proper hygienic care (see matter on mucous-membrane grafting, page 101).
If, for traumatic reasons, a more extensive operation involving the whole lip structure is indicated, one of the harelip operations heretofore given will answer the best purpose.
The cosmetic surgeon is often called upon to correct the vermilion borders of the lips, the usual fault being a lack of sufficient of the delicate membrane to give an artistic appearance or form to the mouth, and in some rare cases the absence of the so-called “Cupid’s Bow” of the upper lip.
Surgical means are of little avail to correct or beautify such fault, and the cosmetic operator must resort to other means. The only practicable method at hand is the careful tattooing of the skin with rose pigment introduced into the skin, preferably with an electric instrument made for that purpose. The hand-tattooing[191] method is slow, irregular at best, and much more painful because of this.
The part to be tattooed is first outlined and then tattooed in linear fashion parallel to the vermilion border presenting, working upward to the peripheral line. The color applied should be pale rose at the first sitting, to be gone over after healing has taken place, and repeated even thereafter until the desired shade has been attained.
The method and instruments involved in the above and the tattooing of scar tissue is fully described in a later chapter.
This branch of surgery has to do with the plastic restoration of the oral orifice. Operations of this kind are required to enlarge a contracted mouth, termed microstoma, whether the same be due to congenital origin or to cicatricial contraction after operative interference about this origin.
Stomatoplasty may also be needed to rebuild an abnormally enlarged mouth, termed macrostoma, which has already been described on page 149.
The operative methods to correct the latter need little mention, since there is usually sufficient tissue present from which the orifice can be properly formed.
The simplest method is to excise the borders of the enlarged mouth or buccal clefts, whether unilateral or bilateral, and to bring the raw edges together by suture. These sutures should be made nearly through the muscular walls of the cheek and at sufficient distance from the edges of the wounds to avoid tearing through.
When the cleft is of sufficient length to warrant tension sutures, they may be employed, alternating with superficial sutures to neatly coapt the skin surfaces.
The mucous membrane should also be sutured with fine silk to insure a perfect closure of the parts, and to avoid, as far as possible, intra-oral infection.
When possible the vermilion borders of the lips should be neatly brought out to the angles of the mouth, where they should be sutured one to the other somewhat diagonally. This will tend to give the angles a normal appearance and shape.
Dieffenbach-Von Langenbeck Method.—It is not unusual after the extirpation of a malignant growth that a greater part of the prolabium has been sacrificed in either of the lips. In this event the vermilion border must be carefully and neatly trimmed away from the healthy lip, leaving a median attachment (see Fig. 251).
The two strips of prolabium will be found to stretch easily. They are utilized to line the entire denuded raw surface and are held in position by a number of fine silk sutures, as shown in Fig. 252.
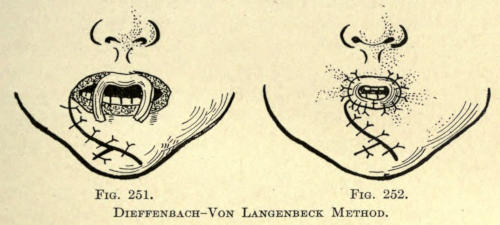
Fig. 251. Fig. 252.
Dieffenbach-Von Langenbeck Method.
Accessory mobilizing incisions, as shown in the above figures, may be necessary to contract the oral orifice sufficiently to permit of such a prolabial grafting, especially where a greater part of the vermilion border has been destroyed. These extra incisions are not necessary when only a small part of the latter is lost; a partial unilateral dissection in that case would suffice to restore the part.
This prolabial lining of the mouth gives it a puckered and contracted appearance for a time only, because the[194] parts soon stretch, while oral gymnastics will help much in restoring its size and usefulness.
The objection to the above method is the danger of partial or total gangrene of that part of the prolabium which has been dissected up and stitched to line the mouth as a result of lack of nutrition or to the bruising or rough handling of the delicate strips during the operation.
Tripier Method.—Tripier refashions the prolabium of the mouth by means of a mucous strip taken from the inner surface of the lip. This strip is left attached at both ends, forming a bridge flap of mucous membrane, the pedicles of the ends giving nourishment to the whole. The bridging strip is slipped into place and is sutured to the outer skin by its superior border, so as to restore the normal appearance and thickness of the lip.
Antisepsis must be carried out scrupulously and a strip of iodoform gauze be placed between the lips operated upon and the gum. In forty-six cases operated upon by this method forty-two were successful, while in two of the unsuccessful cases there was partial gangrene of the flap.
Macrostoma and Overdevelopment of the Lips.—In the cosmetic correction of macrostoma there may be an overdevelopment of one or both lips as well as the wide oral fissure. In such cases the lip structures is to be reduced by the methods heretofore given, before shortening of the mouth line is undertaken, because of the greater freedom allowed the surgeon to correct the deformity.
If possible the operation at the oral angles above referred to should be avoided because of a certain amount of scarring of the skin at either side of the mouth and the resultant stiffness of the parts due to the surgical interference; therefore, when practicable, or when the deformity is of moderate extent, the angles of the mouth should be advanced toward the median vertical of the lips. In such case it is best to do such[195] operations before any labial corrections are undertaken.
Author’s Method.—The method advised by the author is the employment of the Dieffenbach procedure as follows:
A V-shaped incision, its apex pointing inward and its distal ends a half inch from the prolabial line, is made quite deep through the mucosa and muscular tissue, as shown in Fig. 253. The part included in the V is now drawn toward the median line of the lip, causing the wound to gape. The latter is then sutured with deep and superficial silk sutures in the form of a Y, as shown in Fig. 254. The same operation is repeated at the other angle of the mouth.
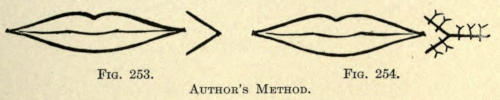
Fig. 253. Fig. 254.
Author’s Method.
When the oral orifice has become lessened, as is frequently the result of cicatricial contraction following ulcerations or operative interference, but which may, too, occur congenitally, the condition is termed microstoma.
Dieffenbach Method.—Dieffenbach advocates the following operation for the correction of this abnormality:
Two lateral incisions are made outward from the mouth across the cheeks and through their entire thickness, extending in length a little beyond the intended angle of the mouth (see Fig. 255). The mucous membrane from within is brought forward and is sutured superiorly and inferiorly to the skin with fine silk sutures.
If there be any difficulty experienced in accomplishing this, owing to the presence of cicatricial thickening of the parts, the latter must be excised in gutterlike fashion (author), and the mucous membrane be freed from its attachment until it comes into place readily.
Care should be especially exercised in lining the angles of the newly formed mouth.
The subsequent contraction of the rima oris following the above operation is prevented only by lining the angle with mucous membrane, healing into place by first intention.
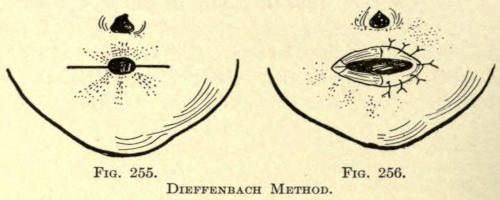
Fig. 255. Fig. 256.
Dieffenbach Method.
Rose Method.—Rose advises sewing a small triangular flap of mucous membrane into each angle to overcome the contraction.
Heuter Method.—Heuter employs an artificial mouth of hard rubber tubing of a size corresponding to the new mouth made in the form shown in Fig. 257.
This ring is forced into the oral opening and the patient is instructed to wear it for some weeks after the operation or until the tissues have become softened and elongated and will no longer retain it.
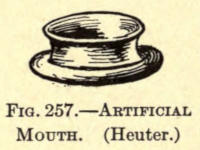
Fig. 257.—Artificial Mouth. (Heuter.)
Nonoperative Treatment.—Smaller operations about the mucosa alone are of no avail to correct this deformity, but where the contraction of the oral orifice is moderate and of recent origin, exercising the mouth and stretching the angles forcibly may help to overcome the deformity[197] to a great extent. Smaller deformities due to contraction usually subside after a time from the normal use of the mouth.
The hypodermic injection of a solution of thiosanimin or fibrolysin (Mendel) are of import in cases where an operation cannot be undertaken. Their use is more fully described in a later chapter.
This branch of surgery has to do with the reconstruction or restoration of the cheek following the excision of scars or the extirpation of malignant growths. The procedure is also recognized as genioplasty.
Where the defect occasioned by the ablation is of small extent, the free and somewhat undermined margins of the wound, which should be made in elliptical form, are neatly brought together with several retention sutures alternating with superficial sutures of fine twisted silk.
If deeper structure than the skin be involved, the diseased area should be carefully removed even to the limitation of the buccal mucous membrane, the soft parts detached from the mucous membrane to render them mobile, and the wound brought together by suture. Care must be exercised so that the tension of the suture does not create a new deformity, such as blepharal ectropium, distortion of the rima oris or the alæ of the nose. If there is enough mucous membrane after the excision of the diseased area, Oberst advocates closing the defect with two pedunculated flaps made each from the mucous membrane of the cheek and of the lip.
In cases where the whole thickness of the cheek is involved the cheek can be incised from the angle of the mouth as far as the border of the masseter muscle down[199] to the adipose layer. A part of the fatty tissue is exsected and pushed aside, the thumb of the operator being introduced into the buccal cavity and pressed outward against the cheek to determine the position and extent of the pathological involvement. The diseased area is cut out with curved scissors, going well into the healthy tissues.
The wound is then brought together by suture while the defect of the mucous membrane is tamponed for four or five days, when it can be covered with Thiersch grafts. The latter in a short time takes on the appearance of mucous membrane and overcomes the contraction of the ordinary sutured wound (Edward-Albert).
Serre Method.—For still larger defects Serre makes the ablation in rectangular form, as shown at A, Fig. 258, and forms a longer flap of rectangular form from the tissue of the cheek and neck. This flap he dissects off from the margin of the maxillary bone to give it the proper mobility. The flap is drawn upward and sutured, as in Fig. 259.
There is little retraction experienced in this method, and answers well for defects of medium extent.
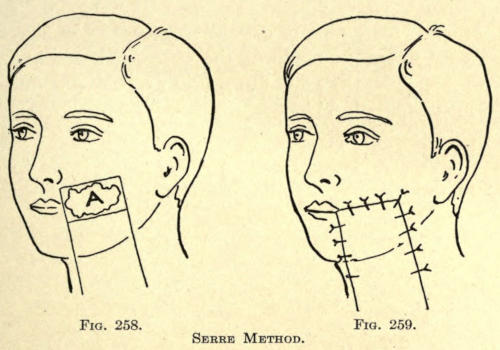
Fig. 258. Fig. 259.
Serre Method.
In larger defects the flaps to be utilized in overcoming the deformity must be taken from the cheek above as well as the anterior chin, as shown in Figs. 260 and 261.
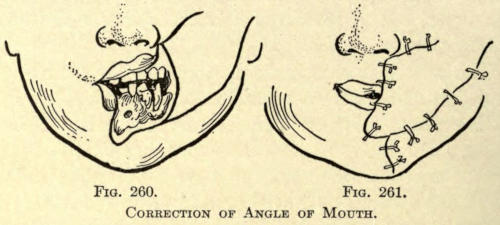
Fig. 260. Fig. 261.
Correction of Angle of Mouth.
Another method is to cut the two flaps as in Fig. 262.
These flaps are made of the entire thickness of the cheek tissue, and are slid down into position and sutured or approximated, as in Fig. 263.
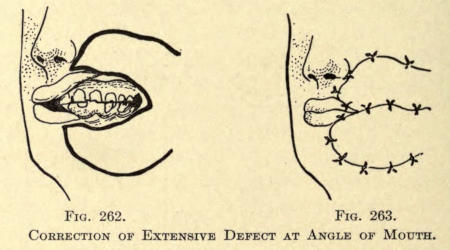
Fig. 262. Fig. 263.
Correction of Extensive Defect at Angle of Mouth.
As a rule the excised mucous membrane subsequently prevents a free opening of the mouth added to by the contraction of the flaps themselves.
To overcome this a flap of skin with its epidermal surface turned inward is sutured into the defect, as will be shown presently, or a pedunculated flap formed at the[201] wound surface before its transplantation into the defect may be covered with skin grafts (Thiersch).
Bayer Method.—Bayer has successfully utilized a large flap from the mucous membrane of the palate and covered it externally with a flap of skin taken from the submaxillary region.
Kraske Method.—Kraske forms the flap to be turned into the defect of the tissue immediately surrounding it, as shown in Fig. 264. This flap may heal into position, even though its pedicle is made up only of subcutaneous tissue, according to Gersuny.
The epidermal surface of such flap is made to form the inner or mucous surface of the repaired cheek (see Fig. 265), while its external surface and the secondary wound are covered with Thiersch grafts, at one and the same sitting.
The only difficulty experienced in the case with men is that the bearded surface of this inturned flap offers considerable discomfort to the patient, although in the majority of cases the skin thus inverted soon takes on the appearance of the mucosa, the objectionable hairs falling out and the hair follicles becoming obliterated.
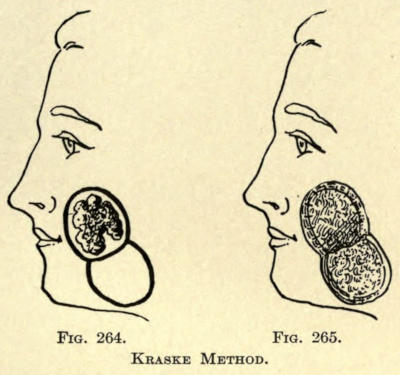
Fig. 264. Fig. 265.
Kraske Method.
Israel Method.—To overcome the above objection Israel makes his flaps from the skin of the side of the neck, the flap being elongated and attached at its upper end, as in Fig. 266.
This flap he turns upward into the defects with its epidermal surface facing inward and sutures it into place, as shown in Fig. 267, leaving the outer surface to granulate over and thicken on the sutured margins[203] to heal into place. This requires from fourteen to seventeen days, when the pedicle is severed and the lower or freed portion of the flap is brought forward. The granulation of the entire surface is scraped off and the free end of the flap is turned over upon itself, as it were, and its margins sutured to the descended skin margin, as in Fig. 268.
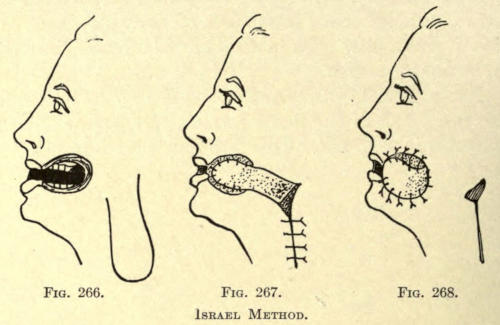
Fig. 266. Fig. 267. Fig. 268.
Israel Method.
Bardenheuer Method.—Bardenheuer has given this subject a great deal of attention, and advocates the use of the skin of the forehead for closing these buccal or oral[204] defects. The skin of the forehead is without hair, is well nourished, and has little adipose tissue underlying it, facts that make it especially useful for these operations. The skin surface he turns into the mouth cavity, while the outer or raw surface is covered with a pedunculated skin flap taken from the region of the intramaxillary region.
The secondary wounds of the forehead and below the jaw should be covered with Thiersch grafts at the same sitting.
The best cosmetic results are obtained by correcting the entire defect at one sitting, as the subsequent contraction of the flaps do not allow of it in successive operations.
The apposition of the raw surfaces of the flap from the forehead and that of the cheek or chin greatly increases their vitality and overcomes markedly the cicatricial contraction.
The pedicle of the forehead flap is cut apart about the fourteenth day and replaced.
In the case depicted in Fig. 269 a large portion of the cheek and the whole upper and a part of the lower lip had to be removed. A large flap taken from the forehead that turned into the defect (see Fig. 270), and a flap taken from the intramaxillary region, were brought over the major and lower portion of its raw and outer surface.
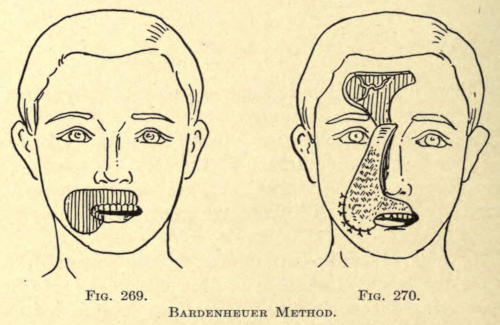
Fig. 269. Fig. 270.
Bardenheuer Method.
In Figs. 271, 272, and 273 the various steps of the same operation are more fully shown, including the placing of the Thiersch grafts and the replacing of the pedicle in Fig. 274.
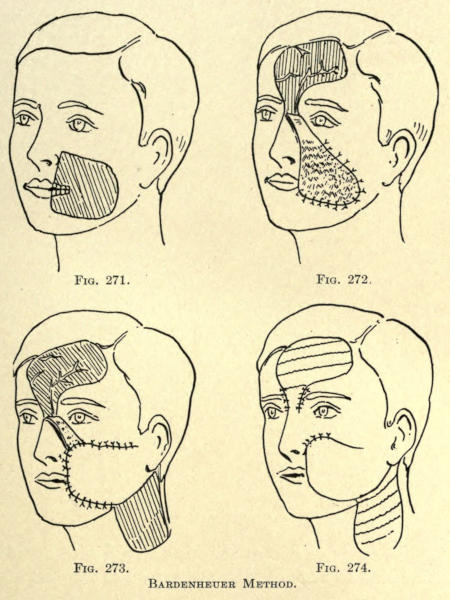
Fig. 271. Fig. 272. Fig. 273. Fig. 274.
Bardenheuer Method.
A still more extensive restoration of the cheek is[206] shown in Figs. 275, 276, and 277, and the position of the skin grafts and replaced flap pedicles in Fig. 278.
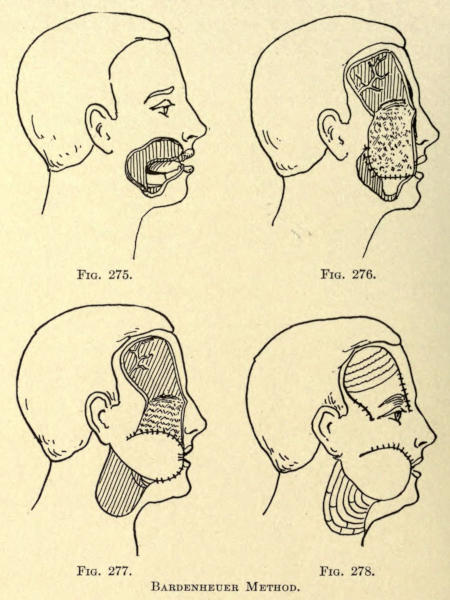
Fig. 275. Fig. 276. Fig. 277. Fig. 278.
Bardenheuer Method.
Staffel Method.—Staffel has also utilized pedunculated flaps taken from the forehead to correct defects of the cheeks and mouth.
His method of procedure in an aggravated case resulting from mercurial stomatitis with resultant cicatricial trismus is shown in Figs. 279 and 280.
Two pedunculated forehead flaps were employed in the above case as well as two flaps each attached by a broad pedicle from the skin under the chin Tripier fashion, and although the patient thus operated upon was only five years of age, an excellent result was obtained.
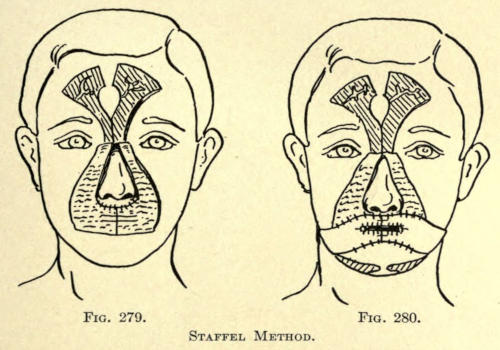
Fig. 279. Fig. 280.
Staffel Method.
When the defect of the cheek due to the removal of a greater part of its structure is so large as to frustrate[207] all attempts at its correction we may resort to the employment of protheses made for the purpose.
In Fig. 281 a case of Morris is shown following the removal of a myeloid sarcoma involving a greater part of the upper cheek, the eye, and the palate. The operator had a prothesis constructed by Hayman, which provided not only an artificial cheek, but also an eye and the palate.
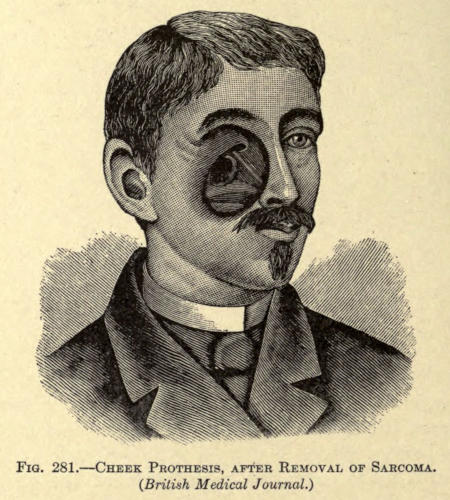
Fig. 281.—Cheek Prothesis, after Removal of Sarcoma. (British Medical Journal.)
How excellently this has been accomplished is depicted in Fig. 282. This prothetic contrivance not only improved the patient’s appearance, but also enabled him to speak intelligibly, which had been impossible, owing to the absence of a greater part of the soft palate.
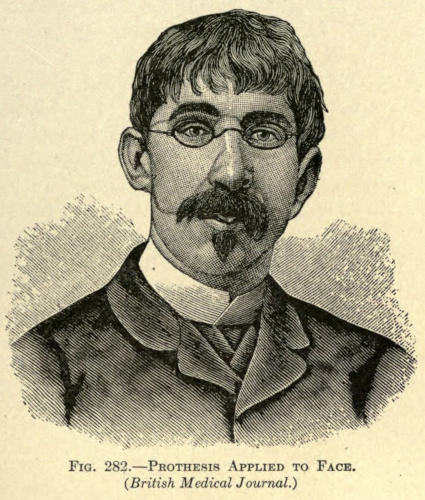
Fig. 282.—Prothesis Applied to Face. (British Medical Journal.)
Hayman describes what he did as follows:
“I obtained a model of the mouth, after which an ordinary plate was made, then a special obturator to correct the palatine defect. With the obturator in position[208] a model of the remaining hollow was taken, and from this a silver plate was struck, which filled accurately into the hollow and under the right ala of the nose; a small tongue of silver was adjusted over the bridge of the nose, and on to this the spectacles were subsequently soldered. An artificial cheek and eye were then modeled in wax to match the other side of the face. A second silver plate was struck upon a metal cast taken from the model, soldered to the inner plate as a cover is fixed to a box. An artificial eye was then fixed to the plate in the proper situation, and the face portion painted flesh-color and japanned. In order to keep the mask in position, a strong wire, fixed to the posterior edge of the artificial cheek, passes around the right ear, and the ear pieces of the spectacles are joined behind the head by an elastic band.”
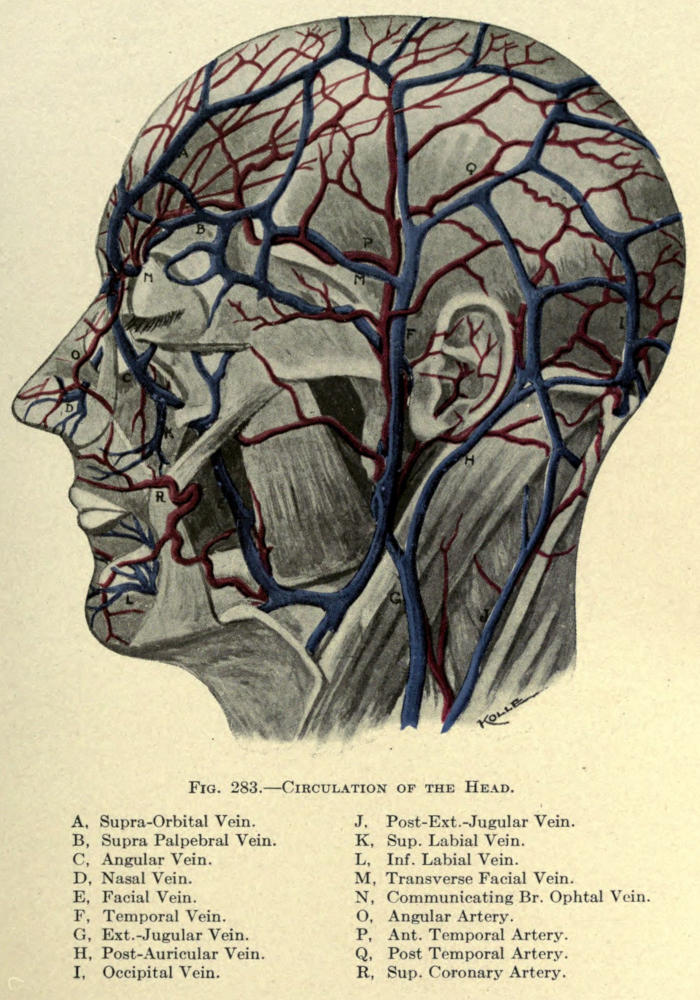
Fig. 283.—Circulation of the Head.
Although the subcutaneous employment of oil and liquefied paraffin has been known for some years, particularly by Corning, who refers to his use of solidifying oils in surgery in an article published in 1891, no actual application for prothetic purposes was made until 1900, when Gersuny first advocated the method. In his published report he says that, “if vaselin, which at the temperature of the body has the consistency of ointment, be liquefied by heat and by the means of a Pravaz syringe is injected into dilatable tissue of the human body, there is produced, at the site where the injection is made, a tumefaction whose volume corresponds to the quantity of vaselin injected. The reaction which results from the procedure is insignificant and the mass appears to rest without change where injected.”
This subcutaneous method of vaselin injection he employed in the case of a young girl to correct a saddle or depressed nose. The operation was purely a cosmetic one, and was performed on May 8, 1900, with a very satisfactory result.
From the time of the appearance of Gersuny’s paper, “Ueber eine Subcutane Prothese,” a number of operators, such as Halban, von Frisch, Kapsammer, Delangre, Rohmer, Stein, and others, began to follow the method with gratifying results.
Pfannenstiel, shortly after, claimed that the injection of vaselin was not wholly without danger, and that pulmonary[210] embolism had been observed by him subsequent to its use. Moszkowicz denied the possibilities of such danger, although at this date it is quite evident that there are many objections to the sole use of sterile vaselin for all subcutaneous cosmetic purposes where such protheses might be indicated.
Eckstein, on July 24, 1901, rehearses these objections and advocates the use of “Hart paraffin,” or paraffin with a melting point of 57-60° C. (140° F.). His method was taken up by Brœckært, Baratoux, Brindel, Watson Cheyne, Walker Downie, Leonard Hill, Lake, Scanes Spicer, Karewski, and other prominent surgeons abroad, and by Parker, Harmon Smith, Hamilton, Quinlan, Connell, and others in the United States.
Drs. Lynch and Heath were the first American physicians to place themselves on record in the employment of the method of Gersuny for the correction of nasal deformities.
Each of the operators employing the now so-called Gersuny method advanced their individual ideas and improvements in the art, and those of distinctive merit will be considered later by the author, who has employed both methods from the time of their incipiency.
The method of procedure in the injection of vaselin or paraffin is practically similar, except for the various ways in which the paraffin of different melting points is rendered liquid.
The indications for the protheses of either method are the same, except where the author advocates the use of either one or the other or a combination of the two from an experience with over five hundred personally conducted cases.
The advantages of the Gersuny method is that the operation is practically painless, causes no scar if properly[211] performed, and corrects a deformity that could not be overcome otherwise in some cases, while in others it would entail not only difficult surgical interferences, but subsequently unsightly cicatrices that would render them more objectional than the very defects which were intended to be corrected.
This is particularly true in the cosmetic correction of depressions about the forehead resulting from direct violence or frontal sinus operations, for obliterating habit furrows, or frowns, between the eyebrows; also to restore the symmetry of the face in hollows of the cheek due to the removal of malignant growths, the maxillæ, or when caused by facial hemiatrophy or a congenital or long-acquired sinking in of the cheeks; while it may also be employed with excellent result to prevent post-operative adhesions about the face after mastoid operations and even to restore the form of the breast after operation for malignant disease and the raising of smallpox pits.
Numerous other uses may be mentioned, such as elevating an undue depression at the root of the nose, raising sunken furrows below the eyes, obliterating nasolabial folds, angular droops about the chin, rebuilding weak or pronounced oval or peaked chins, filling hollows about the neck and shoulders, and in fact anywhere about the body to restore the contour.
In correcting the deformities of the nose, whether congenital or acquired, this method has met an urgent and most useful demand, so much so that many rhinoplastic operations of extensive delicacy have been thrown aside for this simpler, rapid, and gratifying means of surgery.
Not only has it been employed to restore the nasal line in saddle noses, but also in many other deformities of that organ which do not require the removal of superabundant tissue.
According to the appended classification of nasal deformities,[212] given by Roe, it will be seen that many faults of that organ may be overcome by the method.
| Deformities of the nose | { Bony Portion | { Vertical | { Concave. |
| { Convex. | |||
| { Lateral | { Spatulated. | ||
| { Defected. | |||
| { Cartilaginous Portion | { Tip | { Excessive or Deficient Tissue. | |
| { Deviation from Median Line. | |||
| { Wings | { Collapsed. | ||
| { Expanded. |
From the above arrangement, and taking each division separately, the author enumerates the applicability of the subcutaneous prothesis, adding such as are not included in the above.
1. Vertical concavity. An overmarked depression at the site of the bony structure and about the root of the nose.
2. Lateral deficiency of form about the root of the nose extending downward as far as the inferior borders of the nasal bones.
3. Median anterior vertical concavity or saddle nose involving the middle third, otherwise the inferior and superior sections.
4. Deviations of the cartilaginous structure about the middle third of the nose, either unilateral or bilateral.
5. Deviation of the lobule.
6. Deficiency of the lobule.
7. Lobular cleft.
8. Subseptal cleft.
9. Collapsed alæ, unilateral or bilateral.
10. Retraction of subseptum.
In these ten subdivisions much can be done to bring about a normal appearance of the nose.
In selecting a case for subcutaneous injection the operator must well consider the methods to be employed, his successes with such methods, the importance and gravity of the operation, the condition of the patient, the extent of the deformity, the peculiarity of the patient and, particularly, the state of mind of the patient.
While at this date of the use of this method of beautifying parts of the human face we may feel certain of the happy outcome of an operation undertaken by the operator, he must not lose sight of the hypercritical person upon whom the work is to be done; even with an outcome gratifying in the extreme from a surgical standpoint, the patient will insist, and that in eighty per cent of all cases, to still further improve them in spite of the fact that a normal appearance has been attained, often leading the operator into doing what he should not do, and eventually undoing his own excellent efforts.
The author does not mean to imply this as a weakness on the part of the surgeon, but cannot impress too deeply upon him the unreasonable demands of a person insanely bent upon having the alabaster cheek ideal of the poets, the nose of a Venus, the chin of an Apollo, the neck of swanlike form, etc.
The patient believes it lies in the power of the cosmetic surgeon to do with their malformations as a sculptor would model in clay and will insist upon gaining their ideal beyond all reason.
Let the author warn the operator against the “beauty cranks,” especially of those who are just about to engage in great theatrical ventures, circus performances, or “acts,” and very desirable marriages. These are patients who are not only difficult to deal with, but the first to harm the hard-earned, well-deserved reputation of the surgeon and to drag him into courts for reimbursement[214] for all kinds of damages, especially backed up by events, losses, and sufferings largely imaginable and untrue, and ofttimes entirely impossible.
In all cosmetic surgery this branch is the most dangerous from that point of view; therefore the operator should take his case well in hand, proceed with an unshakable determination and give the patient to understand his position, even to explaining what disappointments there might be and what dangers, if any, he might look forward to. The author believes it no unjust demand to have an agreement made with the one to be treated in which these matters are fully considered. Such an arrangement will save him much worry and will tend in the majority of cases to keep his patient satisfied.
On the other hand, the operator should not undertake to do an operation of a cosmetic nature unless he has a fundamental and practical experience of long standing in this branch of surgery, and is ready at all times to cope with such post-operative conditions as are likely to arise, which will be described later.
The author has on various occasions been asked to correct the most hideous malformations of parts of the face, particularly the nose, in which surgeons of high standing, both here and abroad, had injected paraffin in liquid form, usually under a general anesthetic, the most remarkable being that of a hospital orderly in the United States service, who had been subjected to not only one of such injections to correct a saddle nose under chloroform anesthesia, but to three distinctive operations, with the result of a permanent disfigurement, bettered only by a succession of excisions at different parts of the nose.
Apropos of such cases it may be timely to state that a general anesthetic for the performance of a prothetic injection operation is never justifiable and should be considered a lack of knowledge on the part of the operator,[215] unless its use be advised by another surgeon in consultation.
The greatest mistake made with this so-called “filling method” has been a desire on the part of the patient or the operator, or both, to complete the work too quickly. Unscrupulous operators have restored a saddle nose or the contour of the cheeks in a few minutes, when it is an established fact that the work should be done slowly, giving time for the injections to accommodate themselves and to organize before others are attempted. This is not only true of fillings about the cheeks and shoulders, but also of injections about the nose and forehead.
Eschweiler particularly emphasizes the advocacy of oft-repeated injections, and the author recommends such rule without reserve or deviation.
As has been said, the advantage of the Gersuny method over other procedures is that it can be undertaken practically without pain, that it is quick, bloodless, leaves no scar, and is harmless except under such conditions as will be referred to under a separate heading.
While the method entails only the pain of a pin prick a local anesthesia may be employed to overcome this, but never a general anesthetic. The ethyl-chloride spray, except at very small points of the skin, is not to be recommended because it freezes and consequently hardens the very tissue which should be flexible, the operation being undertaken the moment the needle is inserted and lasting only a few seconds. The hypodermic use of a two-per-cent solution of cocain, or better Eucain β, can be employed, but the author sees no advantage in it, as the hyperemic engorgement following its use obliterates, to a certain degree, the actual extent of the deformity.
It is desirable to obtain the best result to have the skin above the part as free as possible. When closely adherent it should be freed by the careful use of a delicate tenotome, inserted at the point where the injection is to be made, the same opening being used for the introduction of the needle of the syringe. If this opening has been made too large a fine suture of silk should be employed to bring the lips of the wound together before the injection is made; the needle point, being knife-edged, will not disturb the apposition and will tend to retain the filling if no undue pressure is used, as in the case of hyperinjection.
Connell has tabulated the difficulties and dangers met with in this work as follows:
1. Toxic absorption.
2. Marked inflammatory reaction.
3. Loss of tissue, due to infection and abscess formation.
4. Pressure necrosis, caused by hyperinjection.
5. Sloughing of tissue as a result of the heat of paraffin.
6. Injection into very dense or inelastic structures, or where scar tissue is firmly attached to the underlying and adjacent parts.
7. Subinjection of too small an amount of paraffin with an insufficient correction of the deformity.
8. Hyperinjection with overcorrection of deformity.
9. Air embolism.
10. Paraffin embolism.
11. Primary diffusion or extension of paraffin (when first introduced) into adjacent normal structures.
12. Interference with muscular action of the nose.
13. Escape of paraffin after the withdrawal of the needle or primary elimination.
14. Solidification of the paraffin in the needle, which renders the injection difficult and causes injudicious expedition on the part of the operator.
15. Absorption or disintegration of the paraffin.
16. The difficulty of procuring paraffin at the proper melting point.
17. Hypersensitiveness of the skin over the injected area.
18. Redness of the skin over the injected area.
To those the author would add:
19. Secondary diffusion of the injected mass.
20. Hyperplasia of the connective tissue following the organization of the injected matter.
21. A yellow appearance and thickening of the skin after organization of the injected mass.
22. The breaking down of tissue and the resulting abscess due to the pressure of the injected mass upon the adjacent tissue after the injection has become organized.
Each of the above subdivisions may be advantageously considered individually, to wit:
1. Intoxication.—The danger of intoxication may truly be said to be more so due to the unclean or unsterilized matter injected than to the absorption following its employment, although Meyer has claimed untoward symptoms found in his experiments from absorption of injections of vaselin in the animal. Taddie and Delain, Stubenrath, Straume, Sobieranski, and Dunbar have corroborated this claim. They injected paraffin of various melting points in the lower animals and observed results therefrom, among which were loss of hair, a reduction of eighteen per cent in the body weight in two months and death.
Stein and Harmon Smith refute these conditions and remarked neither systemic nor local untoward results from such injections when paraffin of higher melting points were used.
Jukuff claims that no toxic symptoms resulting from the absorption of paraffin injected into tissues are shown, unless the amount be equal to ten per cent of the weight of the animal. To have this apply to the human as much as ten to fifteen pounds would have to be injected—an amount never required in operations of this nature.
While it cannot be denied that the injected mass becomes more or less absorbed in from two to three months and is replaced by connective tissue, it may be definitely stated that no toxic symptoms are caused directly thereby, except by the employment of an impure product.
2. Reaction.—The reaction following a properly made injection is of a mild inflammatory character. Considerable inflammation points to some fault in the technique or impurity of the injection. More or less edema of the site and its adjacent area may be noted, associated with slight or marked discoloration and pain of variable degree. The normal reaction following the injection is temporary and does not necessitate treatment or confinement of the patient, who can resume the duties of life fifteen hours after the operation.
3. Infection.—The cause of infection cannot be said to be due to anything but surgical uncleanliness, as it is with any surgical undertaking, and can be overcome by the same means.
The material injected should be thoroughly sterilized by boiling before using. Brœckært suggests combining an antiseptic with the paraffin and has used guiaform, a combination of formic aldehyde and guiacol in a proportion of five to ten per cent; yet this is of little value when we consider how readily[219] these hydrocarbons can be rendered sterile at high temperatures.
4. Necrosis.—Death of tissue may follow an injection of paraffin when too much pressure has been applied, or when too much has been injected into the tissue, cutting off the blood supply, or when the injection has been made into the skin instead of beneath it. Again, constitutional disease, such as diabetes or Bright’s disease, may superinduce the breaking down of the tissue.
Hyperinjection should and can be avoided by the use of the proper instrument with which the required amount is graduated to a nicety. At no time should an injection be crowded into a dense tissue or where the skin is closely adherent, nor carried so far as to create a blanching of the skin. By carefully injecting the mass this danger should be overcome.
Dense or bound-down areas of skin should be loosened and freed, as has already been mentioned.
If care be exercised and small amounts be injected, in preference to overcoming the defect in one sitting, pressure effects are entirely overcome.
The circulation in the skin over the site of injection should be normal immediately after the operation has been performed, determined by observing the reaction in the color of the skin after delicate digital pressure.
5. Sloughing.—That sloughing of the skin should be occasioned by the high temperature of the paraffin injected is a condition entirely inexcusable. Paraffin of high melting points 58° to 65° C., or the so-called “Hart paraffin” employed by Wolff, liquefying at from 57° to 60° C., are to be used with caution. The author doubts whether the temperature of the paraffin at the time of injection, even in the latter method, is ever beyond 54° C. even if the thermometer registers 60° C. in the liquefying, hot-water bath.
By the time it has been drawn into the syringe, which has been heated by dipping into hot water, and the[220] moment it is injected it has lost several degrees in heat.
It would not be permissible to inject a molten mass of a temperature so high as to scar or burn the tissues, and the best results of most operators have been obtained with such of the paraffin group that become liquefied at a temperature of not over 45° C. (112° F.).
The claim of Eckstein, that paraffins of low melting points are more likely to be absorbed, has not been substantiated in actual practice, since we now know that any and all of these injections, irrespective of their melting points, are absorbed in time, giving place to connective tissue, and that rarely, if ever, is there a true and complete encapsulation or encystment of the mass thus introduced. Even the hard paraffins are split up in time into minute pearllike particles which are displaced by the growth of tissue arising from the presence of the foreign substance. This is true even in those cases in which the author has introduced by surgical means solid paraffin plates in the cold state.
6. Sloughing Due to Pressure.—When an injection is forced into a dense or firmly bound-down tissue, as into the body of a thickened cicatrix, or about the point of the nose or the subseptum of the nose without first dissecting off the skin above the subcutaneous layers, an acute anemia is at once marked, followed by inflammation and gangrene.
By injecting sterile water into the area thus loosened with the knife a good idea of the thoroughness of the dissection and the possibility of building up the part to be corrected is obtained, yet in these cases the author has always found more or less difficulty in keeping the injected mass in place for the reason that the divided surfaces tend to unite at their peripheral borders, crowding the mass upward or to one side or diffusing it in such a way that the result has been anything but satisfactory.
To overcome this it is advisable to inject a smaller quantity than necessary to entirely correct the defect, to mold it out flat and to allow it to organize before more is introduced.
7. Subinjection.—Insufficient injection leading to an undercorrection of the defect is a far more desirable condition than hyperinjection, and is easily corrected by a repetition of the treatment, even to a third sitting, until the desired result is obtained. Following this rule will give far better results, as has been said, than to be compelled to remove a part of the filling and some of the connective tissue which has resulted therefrom.
8. Hyperinjection.—The injection of too much vaselin or paraffin is one of the most common faults found with operators. In the first instance a tumefaction of the site results which with the production of the tissue which takes the place of part of the filling makes the result very unsatisfactory and requires one or more cutting operations to reduce it. A peculiar fact with these hyperplastic growths is that even though they may be reduced with the knife to a normal size they seem to redevelop again and again, giving both surgeon and patient great concern.
This, in the opinion of the author, is due to the binding down of the marginal borders, which, in the event of partial extirpation, are not injured sufficiently to displace them and that they unite again in their former position. To overcome this it is found best to excise the entire filling much beyond the margins and to apply pressure over the area until perfect union has taken place.
This is best accomplished with a disk of aluminium, bent to conform to the shape of the part operated, lined with sterilized lint and fixed over the site by strips of Z. O. plaster.
While the hyperinjection of vaselin is not as objectionable as that of paraffin, because of the more ready[222] accommodation and absorption of the mass, it nevertheless leads to diffusion of the material, owing to its softer consistency and consequent greater facility in seeking fine avenues of escape, paraffin having the advantage of cooling upon itself en masse, leaving little to escape into undesirable channels after it has once been molded and set.
Vasserman cites a case in which gangrene of the bridge of the nose resulted after an injection of 2.05 c.c. of vaselin.
However, when these faults occur they are errors of technique, and should be avoided, as has been mentioned heretofore.
The removal of such hyperinjected masses by the aid of paraffin solvents, such as benzine, ether, chloroform, or xycol, applied to the skin above the filling, has proved a failure, nor will heat used externally in the same manner remedy evil.
What is left to the operator is to open the skin and, with a small, sharp spoon curette, remove the mass early, before it has become organized, or to excise the new connective tissue and the broken-down filling, as mentioned.
When, however, the tumefaction resulting from such hyperinjection is not extensive, as is often found about the chin and at the root of the nose, the secondary deformity can be materially, if not entirely, remedied by electrolysis. A needle or brooch of certain hardness is to be employed, connected with the negative pole of a continuous current apparatus. From twelve to twenty milliampères are required. The process is similar to that used with the destruction of hair, nævi, or moles on the face. The needle should puncture the entire tumor or penetrate its maximum diameter and be charged with the current for two or three minutes. Several of such punctures should be made at each sitting, the latter being repeated as often as is deemed necessary by the operator.[223] The reaction which follows this procedure is of little moment, and these sittings can be undertaken every three or four days.
While this method is liable to leave little punctuate scars at the sites where the needle is introduced, it is nevertheless more satisfactory than the linear scar made with the knife, to the use of which the patient may, on the other hand, object, not to speak of the difficulty and unsatisfactory results usually obtained therewith.
9. Air Embolism.—The fault of introducing air under the skin with the syringe at the time of injection can only be the result of flagrant negligence. Every physician should know enough to hold the syringe in an erect or vertical position, and to expel the air above the solution in his syringe, as is done with any hypodermic injection.
Air embolisms are also occasioned by a careless filling of the syringe with the hydrocarbon in a cold state, as the material is now generally used, and while the dangers of such emboli are very much exaggerated they should not be permitted, when by the pouring in of the liquefied material the syringe can be filled evenly.
Practically there is no harm done by the injection of air under the skin, yet it elevates the skin at the site of the defect and hinders the surgeon in accomplishing the best results.
These emboli cause a bulging up of the skin for the time being and may occasion more or less pain to the patient, which passes away in ten or twelve hours, leaving the parts as injected except for such reactionary symptoms or edema, already referred to.
10. Paraffin Embolism.—The creation of an embolism is invariably due to an injection of the foreign substance directly into a blood vessel. This condition is one of the most objectionable, if not the most dangerous, factor associated with the subcutaneous injection of any foreign[224] matter, be it a liquid substance, as, for instance, an oil; many cases have been placed on record where they have been observed after the introduction of even paraffin of high melting points, when introduced under the skin in hot liquid state. Consequently the use of vaselin liquefied by the aid of heat is especially liable to give rise to such condition.
Pfannenstiel cites a case wherein he injected paraffin in which the patient was at once attacked with violent coughing, and for three days exhibited symptoms of grave nature, such as pain in side, intense dyspnea, acceleration of the pulse, hyperthermia, cyanosis of the face, hemoptysis, violent cephalalgia, and vomiting—all indications of pulmonary and cerebral embolism. The injection in this case was one of 30 c.c. of paraffin, with a melting point of 45° C. The symptoms as mentioned continued for about one week, gradually subsiding, and followed by recovery.
Kapsammer has also noticed such symptoms. Leiser, after injecting vaselin to correct a saddle nose, noted an immediate collapse of the patient, which was obviated only by the hypodermic use of ether and the resort to artificial respiration. When the patient returned to consciousness, he was found to be entirely blind in the right eye, the eye before the operation having been known to show only a pronounced astigmatism.
Kofman cites the loss of a patient from the injection of 10 c.c. of paraffin for vaginal prolapsis. Moskowicz observed two cases of pulmonary embolism treated in the same manner, stating that an alarming dyspnea continued for several hours.
Especially have cases in which the injections of paraffin were made submucously for the correction of atrophic coryza shown embolic tendencies. This is especially true when paraffins of high melting points have been employed, as in the case of Pfannenstiel, in which[225] instance the condition of the mass permitted of freer absorption or the high temperature caused a coagulation of the blood in the veins, leading to thrombosis and embolism, and when the amount of such an injection is so large as to prevent cooling and hardening in the normal space of time added to the quantity and associated at the same time with consequent pressure, predisposing to absorption or dissemination, especially if the injection be made into the parenchymatous instead of the subcutaneous tissue.
Comstock, in his experience on animals, states that “in all cases in which paraffin was used at 102° F. the animals died within two weeks’ time, hence the specimens at that temperature are limited (death being by thrombosis). In all other cases with the higher melting point, 110° F., no unpleasant results were experienced.”
Hurd and Holden have observed a patient who had previously undergone two injections of paraffin for the correction of a depression in the upper part of the nose. A third injection was advised and made under the same conditions as the first, except that no cocain anesthesia was employed, the paraffin being at same temperature as before.
The moment the injection was made complete blindness in the right eye resulted, while a small ecchymotic spot appeared at the site of the needle insertion in the skin. Half an hour later an examination of the eye showed the right pupil dilated and inactive light stimulus, the patient being unable to distinguish light from darkness. Ophthalmoscopically the lower branch of the central retinal artery and its subdivisions were found to be empty and in a state of collapse, evidenced by their pale appearance. The upper branch of the same vessel was found to be poorly filled.
The authors endeavored to remove the embolism to a collateral branch of the artery by the use of amyl[226] nitrate, digitalis, and pressure on the globe of the eye, with no effect. Some hours later edema of the retina appeared, followed by permanent loss of sight. The same authors have observed several cases of pulmonary embolism result from the injection of paraffin.
It is also a fact that injections of the nature being considered, while not causing immediate embolism, may do so as a result of phlebitis, caused by a direct injection into the vein or over or upon it in such a way as to cause irritation.
Mintz reports a third case of amaurosis following a paraffin injection. The latter was made to correct a saddle deformity caused by syphilis. Three minutes after the injection the patient complained of pain in the left eye, which was followed by total blindness, vomiting, and a pulse of 48. Several days later there appeared symptoms of venous congestion in the orbit, paralysis of the ocular muscles, corneal cloudiness, and exophthalmos, a small gangrenous spot appeared at the site of the injection.
Brœckært observed a case of facial phlebitis, followed by pulmonary infarction. Brindel cites a case in which he observed a hard line of considerable extent and painful to the touch, extending from the inner angle of the eye to the angle of the eye, where it deviated toward the root of the nose and terminated at the origin of the eyebrow.
De Cazeneuve made an injection, and on the following day noted that the right cheek had increased considerably in size with an elevation of temperature in the part. Two days after, under the right eye and to the right of the nose, the whole cheek was red, hot, and much distended, giving the skin a glazed appearance. Palpation was extremely painful. A hard line could be made out, extending from the inner angle of the eye outward and downward under the lower eyelid and terminating in the center of the edematous cheek. The[227] phlebitis in this case resulted without the development of an embolism.
After a careful study of the causes of such embolisms we come to the conclusion:
1. That the injected mass should not be heated above a certain melting point.
2. That hyperinjection should at all times be avoided, particularly with paraffins of high melting points.
3. That the injection should be made subcutaneously not into parenchymatous tissues, and
4. That a puncture of a vein or the introduction of the injected mass into a vein should be avoided.
In the consideration of the first two causes the author advocates using injections of low melting points only at all times; in fact, from his experience with over two thousand subcutaneous injections, he relies entirely upon such paraffins or hydrocarbon mixtures as are semisolid at 70° F., appearing as a white cylindrical thread from the needle of the syringe as pressure is applied.
With such a preparation and a careful introduction of the needle, as described later, and with the injection of an amount much less than that needed to correct the deformity and proper digital compression on the blood vessels and about the site of the injection embolism is practically impossible.
The avoidance in the third instance is self-evident, and it is to the fourth fault and cause that we must pay particular attention.
Stein says that all that is necessary to avoid puncturing a vein is to first introduce the needle alone under the skin and to attach the syringe only when it is found no flow of blood results from the puncture thus made.
Freeman and the author add to this by advocating the use of a somewhat blunt-pointed needle instead of the extremely sharply pointed knife-edged needles usually furnished with syringes intended for this purpose.
11. Primary Diffusion or Extension of Paraffin.—The spreading of paraffin into normal tissues about the site to be corrected by prothetic injection is a fault due principally to a careless use of the syringe. The employments of an improper syringe in which the amount to be injected cannot be graduated or controlled will be considered later—the result with such being hyperinjection. In this event, when the anterior line of the nose is to be restored, the mass is liable to find its way into the loose areolar tissue of the infra-orbital region; in correcting a nasolabial furrow the mass is pushed upward or is forced into the tissue of the cheek above it, aggravating the trouble; in obliterating a frown it travels upward toward the margin of the scalp, giving a median prominence to the forehead that is found to be very difficult to correct; in injections about the mouth the mass moves down upon the chin or accumulates at the angle of the jaw; in correcting the creases beneath the chin it seeks the sides of the neck, even traveling to the superior border of the clavicle at its sternal third. Many other forms of such diffusions can be mentioned directly due to primary diffusion the result of hyperinjection.
Enough has been said of the danger of hyperinjection, yet even with a proper amount of the injected mass this distention may be observed. To avoid this the operator, or his assistant, should compress the margins of the site of the injection with his fingers firmly applied, as, for instance, in the injection of the root of the nose pressure should be made at both inner canthi and over the tissue just above the root of the nose and beneath the finger tips.
Downie advocates the use of celloidin in the correction of a saddle nose as follows: He paints a band of celloidin or collodion down each side of the nose, limited by the line of junction with the cheeks, and another band across the root of the nose. These painted on bands he[229] allows to dry and contract for fifteen minutes before undertaking the injection.
The contraction of these bands prevents to a certain extent the spreading or extension of the liquid paraffin into the cellular tissue about the eyes, yet experienced digital pressure is at all times to be preferred.
If a liquid paraffin or hydrocarbon mixture or vaselin is used, the immediate use of ice cloths applied to the part as digital pressure is removed, is advisable to aid in the rapid hardening or setting of the injected mass before the tension of the tissues over and about it might influence it. With semisolid injection this is not necessary, except in the subsequent treatment, as will be considered later, because the mass, unless of too soft a consistency, as, for instance, vaselin, will practically remain as injected and molded.
Vaselin when injected into tissue where there is tension would naturally be forced out of position and shape, and should not be used except in combination with a paraffin of a melting power high enough to give the proper consistency to the former.
12. Interference with Muscular Action of the Wings of the Nose.—That nasal respiration may be encroached upon as a result of injecting paraffin about the nose has been observed by Alter. He points out that during nasal inspiration there is a tendency for the alæ to contract upon themselves or to move inward, decreasing the lumen of the orifice, and that in the normal state this movement is counteracted by the action of dilator muscles of the alæ—that is, the dilator naris anterioris, the pyramidalis nasi, and the levator labii superioris alæque nasi—and that this muscular action is interfered with owing to the pressure of the paraffin upon these delicate structures, and resulting in more or less permanent collapse or indrawing of the alæ during inspiration. He observed considerable interference with inspiration in a case cited in which an injection of paraffin had been made.
To avoid undue pressure upon the structures referred to, it is advised to have an assistant place a thumb into each nostril and the index fingers without and above the alæ in such way that the tips of the fingers may be enabled to exert the necessary pressure over the injected mass into these structures, and to maintain this pressure until the mass has been properly molded and set. Connell advises inserting the little fingers into the nostril to prevent an encroachment on the lumen of the nasal canal.
The above applies particularly to those cases where injections are made into the anterior lower or lateral third of the nose, as, for instance, in overcoming slight depressions in the anterior line, immediately above the lobule or in a low unilateral deviation of the nose.
13. Escape of Paraffin after Withdrawal of Needle.—When the injected mass employed is of a semisolid consistency, as heretofore advised, it is hardly possible for the mass to be forced out through the opening of the skin made by the introduction and withdrawal of the needle, unless there be an unwarrantable immobility of the skin above the site to be injected. The latter should be corrected before injection.
The mass after having been molded in the shape desired may be further hardened and set by the application of ice cloths or spraying with ether before the needle is withdrawn from the skin, yet this is hardly necessary, and the author advises against the practice for the reason that pressure of the needle prevents proper and free molding of the mass and renders the tissue liable to further injury by scraping its point to and fro subcutaneously, adding to the extent of the wound and the dangers of infection and repair.
The skin immediately around the needle hole, after withdrawal of the needle, may be gently smoothed out with the dull rounded metal handle end of the bistoury to free the interdermal canal of any foreign matter.
The skin about the needle hole is then gently washed with a fifty-per-cent solution of hydrogen peroxid, dried with a sterile cotton sponge and the opening sealed with a drop of collodion. Subsequent treatment of the parts will be considered later.
14. Solidification of Paraffin in Needle.—This occurs only when paraffins of high melting points are employed in liquid form in the syringe, and is due to the rapid cooling of the paraffin in the small metallic cannulæ, or needle, wherein it sets more readily, since the volume contained therein is very small, often not more than two or three drops.
This cooling establishes a pluglike formation in the distal end of the needle, which prevents a proper use of the syringe, often breakage, and when suddenly liberated by an extra pressure on the piston rod causes a rapid discharge of the contents of the syringe to an extent not desired with the result of hyperinjection.
This fault was one of the most annoying in the early days of such injections when syringes of ordinary pattern, such as the Pravaz, or those built like the ordinary hypodermic, were used. It was not unusual to have the paraffin cool in the needle so quickly between the latter in the flame of an alcohol lamp that the syringe became unmanageable and broke in the hands of the operator. Since that time new and more useful syringes have been introduced by various operators which overcome this difficulty, yet with them, too, come the employment of semisolid paraffins or mixtures thereof. Yet, as some authors insist upon using paraffins of high melting points, it may be well to rehearse their methods of overcoming this annoying intraneedle solidification.
Eckstein surrounds the syringe and needle shaft, except the tip of the needle, with a rubber tubing, as shown in Fig. 284, to act as an insulator, and thus, for a time at least, keep the preparation liquid. Before filling the syringe he heats it by several immersions in and internal[232] washings of hot sterile water. To prevent the paraffin from setting in the exposed tip of the needle he draws into the filled syringe a few drops of hot water, which are injected into the tissues, causing no objection to the method.
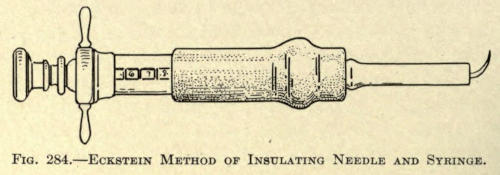
Fig. 284.—Eckstein Method of Insulating Needle and Syringe.
Paget and Harmon Smith warm the needle in hot sterilized or even boiling water. Previous to this Smith cools the contents of the syringe drawn into it at a temperature of 120° F. by immersing the latter in a bath of sterilized water at a temperature of 80° F.
From the above it will be noted that Smith advocates using the injections in semisolid state being ejected in a thin, cylindrical thread. A syringe of special construction, as referred to later, is, of course, required for such work.
Quinlan has invented a so-called paraffin heater, as shown in Fig. 285, in which the paraffin is kept in solution by the syringe being surrounded by a continuous flow of hot water. A plain and very objectionable syringe is shown in the illustration, and while the preparation in the syringe is thus kept in[233] a liquid state the solidification in the needle is not overcome.
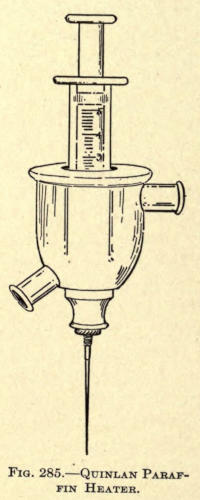
Fig. 285.—Quinlan Paraffin Heater.
Downie winds fine platinum wire about the needle through which he passes the current from a storage battery to keep the needle hot, yet such an arrangement is obviously difficult of manipulation, and when paraffins of high melting points are employed it is quite likely that a plug is formed in the exposed point of the needle.
Karewski has introduced a syringe having a jacket through which hot water is allowed to circulate, while similar instruments have been originated by Pflugh and De Cazeneuve. None of these overcome the difficulty in question.
Viollet went even further by inventing a syringe surrounded with a coil of resistance wire, heated by an electrical current, and Delangre, Ewald, and Moszkowicz use special thermophorm sleeves over the syringe proper; all, however, offering the same objection in the exposure of a part of the needle in which temperature of the liquid must necessarily be lowered, or be low enough to cause plugging, the very fault for which all these modifications have incidentally been urged, as the greater amount of paraffin in the syringe itself is as a rule large enough to retain sufficient heat to permit of its ejection, if the injection is made as expeditiously as possible.
The objection of the setting of the paraffin in the barrel of the syringe has never hampered any operator, the difficulty in these instances having been entirely due to the obstruction offered its ejection by the threadlike plug obstructing the metal cannula before it; the barrel, being glass, retains its temperature more readily than the thin metal needle, hence the difficulty.
That all prothetic preparation of the nature in hand should be placed in the barrel of the instrument in liquid form is essential, in that the syringe is thus filled to its required height evenly, and devoid of air spaces, yet in the light of the best and most successful results[234] the mass should be allowed to cool and be ejected in semisolid state from a specially constructed instrument, to be described later.
With such method it is impossible to have an occlusion of the needle at any time, and the objection of sudden outbursts of unknown and undesirable quantities of the mass is entirely overcome.
15. Absorption or Disintegration of the Paraffin.—The question of the ultimate disposition of paraffin, injected subcutaneously for any purpose, has been an extensive one in which many operators have taken part.
Gersuny at first claimed an encapsulation for the injected mass of vaselin, which he states was not taken up by the lymphatics, but remained in situ as an inert, nonirritating body. Shortly after it was shown that the encapsulated mass soon became ramified by newly formed, fine bands of connective tissue, which developed more and more in the part until the entire mass had become displaced by this tissue with an eventual consistency of cartilage.
Eckstein claims that at first a capsule of new connective tissue incloses the injected mass (Hart paraffin) a few days after the latter is injected, which can be easily stripped away from the encapsulated matter several weeks or months after, showing a smooth inner wall, the encysting capsule showing a decided lack of blood vessels, proving histologically its relation to the structure of cicatricial formation.
In this Eckstein is undoubtedly mistaken. He objects to the ultimate replacement with connective tissue for the vaselin process of Gersuny, when in reality we have begun to realize that such result will follow any hydrocarbon subcutaneous injection unless the latter be made in small quantity into parts of the body which are in constant motion.
The latter is shown with injections of paraffin made into or about the nasolabial fold. The tumor is so small[235] as to be hardly felt by the palpating finger, but soon takes on larger proportions, evidencing an encapsulation of some extent or less independent of the encysted mass. That this is true can be ascertained by incising these little hard tumors when the contents can be readily pressed out or evacuated, the mass appearing practically as injected months before.
The same result is shown by Harmon Smith, who made an injection of paraffin (110° F.) into the peritoneal cavity of a rabbit which was killed twenty-two days later. On examination no sign of inflammation of the peritoneum was found—a fact that seems to prove the nontoxic effect of paraffin—nor were there evidences of the formation of adhesions. The mass had become rounded, had traveled about the abdominal cavity, and was found lodged between the liver and the diaphragm.
Comstock, with his experiences of injections of paraffins at high melting points, found that the harder paraffins do not become encysted, but become a part of the new tissue, which belief is corroborated by Downie, who introduced paraffin into a carcinomatous breast. Upon subsequent amputation and microscopic examination there was shown an intimate connection between the ramified site of the injection and the surrounding tissue. The same results have been noted by Jukuff.
Smith found that, in trying to remove an injected mass of paraffin several months after introduction, the greater part of the mass had become so thoroughly imbedded in the meshes of the newly formed connective tissue that it was practically impossible to remove it without including a considerable portion of the connective tissue as well.
Stein claims also that the paraffin is absorbed, little by little, as it is replaced by the new connective tissue, no matter what the melting point of the introduced paraffin might have been. The mass grows smaller to a degree, according to the amount injected; finally, at the[236] end of a month or more, the entire mass is replaced by a tissue perceptibly analogous to cartilage.
Freeman, like Eckstein, claims that encystment of the paraffin occurs soon after the injection, much like that following a bullet or other foreign body in the tissues, but, unlike the latter author, that a limited amount of the connective tissue also penetrates the mass, which is speedily converted into a solid cartilagelike body.
Wendel believes entirely in the encystment theory, while Hertel, in specimens removed twelve to fifteen months after injection of paraffin with a melting point of 100° F., found a wall of round cells under various states of inflammation surrounding the masses with fibers of connective tissue traversing the latter. In the various histological findings he argues that the greater the tissue surface exposed to the injected foreign body the greater the irritation, and the larger the smooth paraffin mass the less the reaction; in other words, small masses of the injected mass cause a higher rate of tissue formation, while the larger masses have a tendency to encystment merely. He also believes that the harder paraffins require a greater length of time to become absorbed, and that during such time of resorption new connective-tissue growth is established, continuing to the time of its complete disappearance.
Comstock, after thorough and extensive investigation with the injection of paraffins of various melting points made at varying times after the injection of such procedures, concludes definitely that, “In paraffin we have a substance that will fill in spaces of lost tissue, and not remain entirely a capsulated foreign body, but become a bridgework, and, in fact, a part of the new tissue.”
Wenzel, after an unsuccessful attempt to overcome a laparocele by the injection of paraffin, a year later performed a radical operation of the parts. The excised tissue at the site of the injection showed deposits of the[237] broken-up mass of paraffin, each being enveloped by a capsule of connective tissue without any signs of ramifying bands, and hence decided against the belief of the resultant tissue formation.
Eschweiler, the latest authority on the above question, after examining microscopically a portion of paraffin-injected tissue that had been carried “in situ” on the bridge of the nose for about one year, concurs absolutely with the connective-tissue replacement belief.
From the foregoing it may be definitely accepted that while there may be an encapsulation or encystment of the injected mass, be it what it may so long as it belongs to the paraffin group, there is always a ramification of the mass by the formation of the strands of new connective tissue which eventually in a month or more, according to the amount of the mass, develops to a size corresponding to the latter or even beyond the size of the latter, as will be mentioned later, and that in all cases the paraffin is ultimately and almost, if not completely, crowded out of the area occupied by the injection, and that its disappearance is accountable to absorption.
This absorption, following such an injection, is productive of no harm to the human economy, and the new tissue caused to be formed by such injection truly enhances the cosmetic and surgical value of the method inasmuch as an encapsulated mass of paraffin is liable to displacement, spreading, and irregularities, should it be subjected at any time to external violence.
Such violence, again, would lead to the irritation and inflammation of such cyst wall, causing an undue crowding upon the parts injected and possible gangrene of that part of the wall upon which such pressure was brought to bear, leading to unsightly attachment and ultimate contraction of the skin where bound down by the inflammation, or even evacuation by the absorption of gangrenous material and resultant abscess.
That this absorption or disintegration of paraffin is[238] of no consequence may be proven by all the early cases in which such injections were used. Gersuny’s first case, having been done May, 1899, shows no diminution of the prothetic site at the end of two years. The same may be said of the hundreds of cases done by other operators.
The greater question in the mind of the author is what will be the ultimate behavior of this new connective tissue.
That the development of this new connective tissue is gradual has been mentioned, some authors claiming a complete replacement of the mass at the end of a month, others from two or three months. Morton says that four months’ time is required before the mass is, more or less, completely removed and replaced by organized tissue. The author believes, however, that the length of time necessary for this replacement not only varies, proportionately with the amount of paraffin injected, but that it differs in each case, and markedly with some patients in which the growth or developments of the new tissue did not cease for months and even a year after such injection. This corresponds truly to a hyperplasia, and will be considered later.
Time alone will show the ultimate behavior of this new tissue, and while it is reasonable to argue that this newly organized tissue could cause no untoward results, it must be determined whether this tissue will not undergo atrophy and contract, or become susceptible to other changes in time. It is a new tissue practically, and as yet we know nothing of its idiosyncrasies, although its histological nature is determined.
We do not know that irritations, such as surgical interference, will cause it to take on new growth, as evidenced by the attempts of extirpation of unaccountable overcorrections obtained with injections made early in the time of the employment of the Gersuny method, in which the parts practically grew back to their former size or became even larger. This may be accounted for[239] by the fact that most, if not all, of the connective tissue was not removed or points to an active nucleus or several such centers which were not destroyed.
That the growth is not limited by the size of the mass injected is the author’s belief; in other words, the replacement of the new tissue is not proportionate to the injection, but that other forces, such as adjacent tissue pressure and presence and outer influences, as, for instance, the daily massage of the parts with the hands, have much to do with the final amount of tissue caused to be developed by the initial stimulus of the injection. Nothing further or definite, however, has been written on this supposition.
16. The Difficulty of Procuring Paraffin with the Proper Melting Point.—This should not prove an objection to the method, since operators can procure pure and sterilized paraffins of the various melting points from any reliable chemical house.
What the operator should determine first of all is the kind of paraffin he intends to use for subcutaneous injection.
The selection of paraffin of a certain melting point should be influenced by what he has read on the subject, as given by authorities of wide experience.
A few cases do not suffice from which to draw conclusions; it is only from a great number of similar operations that a definite form or preparation of paraffin can be decided on.
From the following authorities is shown a variance in the melting points of the preparations used, but by a glance it may be noted that the first division of men, from numbers 1 to 10 inclusive, use paraffins of melting points very near to each other; the latter group, from 11 to 13 inclusive, employ those of the higher melting points.
The former group may, therefore, be said to utilize the paraffins of lower melting points.
| Group I | |||||
| 1. | Gersuny | 36-40° | C. | 97-104° | F. |
| 2. | Moskowicz | 36-40° | C. | 97-104° | F. |
| 3. | Parker | 102° | F. | ||
| 4. | Freeman | 40° | C. | 104° | F. |
| 5. | A. E. Comstock | 107° | F. | ||
| 6. | Walker Downie | 104-108° | F. | ||
| 7. | A. W. Morton | 109° | F. | ||
| 8. | Harmon Smith | 110° | F. | ||
| 9. | Stephen Paget | 108-115° | F. | ||
| 10. | Pfannenstiel | 115° | F. | ||
| Group II | |||||
| 11. | Brœckært | 56° | C. | 133° | F. |
| 12. | Eckstein | 56-58° | C. | 133-136° | F. |
| 13. | Karewski | 57-60° | C. | 134-140° | F. |
From a glance of the first group the variance of the temperature of melting points is not a great one, practically lying between 102° and 115° approximately. When we consider the actual difference in the employing practicability and the effect upon the tissue there is practically little, if any, difference. The only difference between these authorities is that some employ their preparation in liquefied form, through the application of heat, while the others employ it in the cold or semisolid form. The choice of such method, from what has already been said, should unreservedly be the employment of a paraffin in the cold or semisolid form at a mean temperature of about 110° F.
This choice would fall upon any one of the paraffins used by the authorities given in Group I.
The objections to the “Hart paraffins” of melting points given in Group II have been sufficiently shown in preceding paragraphs, although a few pointed objections from the various surgeons may not be out of place here to offset the claims and advocacies of those employing[241] the preparation in liquid form at higher temperatures than 110° F.
Paget says: “I am absolutely sure now that Eckstein’s paraffin is without any real advantage. It is very difficult to handle; it sets very rapidly; it causes a great deal of swelling and some inflammation, and may even produce some discoloration of the skin, and it yields no better results than does Pfannenstiel’s paraffin, which melts at 110° F.”
Again he says: “The best paraffin is that which has a melting point somewhere between 108° and 115° F. When the paraffin has to stand heavy and immediate pressure, the higher melting point is preferable.”
He had up to the date of the latter extract operated upon forty-three cases of deformed noses and “in no case was there embolism, sloughing of the skin, or wandering of paraffin.”
Paget, however, employs the paraffin in liquefied form, and allows cold water to trickle over the nose while the injection is molded into form. Of this later.
Comstock says, “Paraffin must be used where it will be at all time above the body temperature,” and further that, “in selecting the melting temperature for surgical uses, it should be that from 106° to 107° F., the best for use in subcutaneous injections, for the reason that it gives a substance firm enough to hold very well its form, especially when confined by the surrounding tissue, and at the same time with a melting point out of the reach of the system at all times.”
From this we are given to understand that he uses his preparation in cold form entirely when injecting, but of the melting point mentioned.
The author can see no advantage in using any paraffins of low temperature melting points in liquid form. Here is the very factor of causing embolism reintroduced. Surely a liquid of any kind injected into a blood vessel will give cause for trouble, even if the temperature of[242] the setting of such a paraffin be high or low. The employment of the paraffins of a melting point above 120° F. in cold form is difficult, if not impossible, even with the latest pattern of screw syringe which is quite true, but there is no need of using such paraffin nor any liquefied paraffin, since any such preparation of about the melting point of 110° F. will serve every purpose overcoming all the objections of the advocates of those using any other.
If a vessel be injected and filled with any paraffin preparation there is danger of phlebitis and thrombosis; the only possible way to overcome it is not to puncture the vessel.
While a preparation injected cold can be more easily governed from without by digital pressure or guidance, what can be said for a hot seething preparation introduced under great pressure?
Furthermore, when paraffin is injected in liquid form, especially when so rendered by a temperature necessarily even higher than the actual melting point, there is danger of searing the entire site intended for injection—a condition inducive to no good and a burning of the skin where the necessary superheated needle enters it, causing a punctate scar, more or less painful during the time required to heal the wound.
With the later knowledge that small amounts should be injected, and that such injections should be repeated, it being known that such method facilitates the production of new connective tissue, may we not draw the conclusion that the result obtained by the injection depends not upon the injection per se, but the resultant of that injection—namely, tissue production, and that this tissue production is the outcome of a stimulus in the form of that injection?
There has not appeared an authority who has claimed otherwise for injections of paraffin hot or cold, while it is true that the use of liquefied paraffins at high[243] temperatures have caused all sorts of untoward results, while those of lower melting points in similar form have not escaped objections.
The author has used the cold-injection method in over three hundred nose cases without a single case of sloughing, embolism, or death, and in no case was there secondary diffusion or hyperinjection. The only fault has been the desire on the part of the patient to be finished too quickly, which usually leads to a result not as satisfactory as when the injections are made sufficiently far enough apart to allow the formation of organized tissue at the site of injection.
Gersuny’s preparation of paraffin, particularly useful for the cold-injection method, is made as follows: A certain amount of cold paraffin, melting at about 120° F., and white cosmolin or vaselin, melting at about 100° F., are mixed by being heated to liquefaction. The bulb of a clinical thermometer is then coated with the cooled mixture of paraffin, which is then placed into a hot-water bath, the temperature of which is gradually raised until the paraffin melts and floats upon the surface of the water. The water is then allowed to cool and its temperature noted just as the oil-like liquid paraffin begins to look opaque, which marks the melting-temperature point of the mixture.
Should this be found to be too high more vaselin is added, or vice versa, until the desired quantity of both is known.
This method of preparation is, however, a tedious and awkward one, and can be readily improved upon by mixing certain known quantities of the one with the other after the first experiment.
The author recommends the following formula for the preparation of a mixed paraffin, which he has found serviceable and satisfactory for use with cold-process injections and employed by him for the last four years.
| ℞ | Paraffin (plate, sterile) | ʒij; |
| Vaselin alba (sterile) | ℥ij. |
The two are placed into a porcelain receptacle and melted in a hot-water bath to the boiling point, then thoroughly mixed by stirring with a glass rod and poured into test tubes of appropriate size and allowed to cool. Each tube is sealed properly with a close-fitting rubber cork, which may be coated with a liquid paraffin without, including the neck of the tube, and put away for later use.
Since 1905 the author has used an electrothermic heating device in which the paraffin mixture is prepared. The apparatus is made up of a metal pot set into a resistance coil, and is shown in Fig. 286.
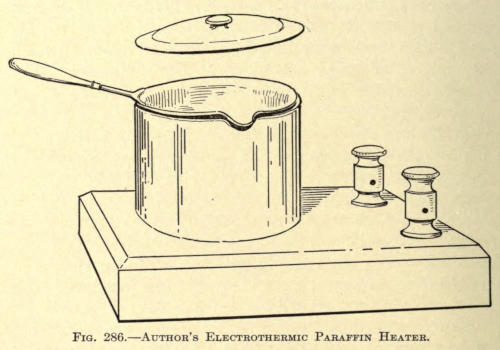
Fig. 286.—Author’s Electrothermic Paraffin Heater.
This instrument overcomes the complications of the water bath and burning or browning of the paraffin mixture, so commonly found with ordinary methods, the temperature of the resistance coil within the heating chamber being controlled by a small rheostat at will.
Before using, the contents of each test tube thus prepared are reheated to sterilization and poured into the barrel of the syringe to two thirds of its length, the piston introduced and screwed down into position; the syringe being placed to one side until its contents have been cooled, or the entire instrument is immersed in sterilized water at about 70° F. until the paraffin mixture has set or becomes uniform in consistency, which takes about five minutes.
Upon screwing down the piston the mass will be found to issue from the needle as a white, cylindrical thread, and is ready for use in this form.
Harmon Smith has had such a paraffin prepared which has a melting point of 110° F. This can be purchased in the market in sterile sealed tubes ready for use. The contents of these tubes should, however, be resterilized at the time of employment.
The same author prepares this paraffin of 110° F. melting point by mixing sufficient petroleum jelly (evidently white vaselin) with the commercial paraffin melting at about 120° F. to bring the melting point down to 110° F. He claims that making such a mixture is a difficult matter, since a plate of paraffin will have various melting points, one corner melting at 120° and the opposite as high as 140° F. He advises having the mixture accurately prepared in large quantities and dispensing it in test tubes of one-half ounce capacity, as now found on the market. The mixture is poured in hot liquid form into these test tubes, which are then sealed with wax and placed on a sand bath, whose temperature is raised to 300° F. to insure sterilization.
The latter author has devised a neat paraffin heater, shown in Fig. 287.
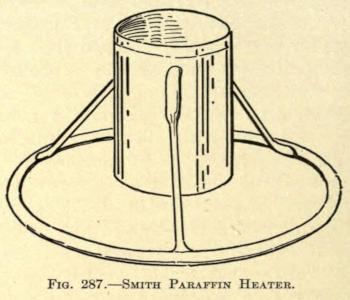
Fig. 287.—Smith Paraffin Heater.
Of this he says: “To insure still further the sterilization of the paraffin, I have devised a tin (nickle-plated) receptacle supported on an attached tripod, which raises the bottom an inch from any plane surface[246] on which it is placed, and is closed with a detachable lid. This arrangement prevents the paraffin from burning or browning. Into this I pour the paraffin from the test tube, after melting, and place this receptacle into a sterilizer, or any ordinary boiler—surround it almost entirely with water and then boil. After I have boiled it for a few minutes I remove the receptacle and permit it to cool until the paraffin therein is about 120° F. I then draw it up into the syringe, which has been sterilized in the same boiler with the paraffin. When sufficient is withdrawn, I evacuate the air bubbles from the syringe by pressing the piston upward and run my set screw into place. Some two or three minutes are now allowed for the paraffin to assume equal consistency throughout and to cool down to a semisolid state. When the paraffin reaches this consistency it may be kept many hours ready for use, at the temperature of the room, if only the precaution to warm the needle is taken each time before attempting the injection.”
17. Hypersensitiveness of the Skin.—A permanent hypersensitiveness of the skin over the site of a subcutaneous paraffin injection has never been definitely shown. While it is true there is some pain and feeling of stress and fullness[247] over and about such area, immediately after the operation, this has subsided in about twenty-four hours in the average case, except in those where a very hot liquid paraffin and of large amount has been injected, when several days are required to overcome these symptoms.
Smith claims a numbness over the site of the injected area which soon passes away, but this is perhaps more a feeling of fullness rather than one of anesthesia.
The author has observed, however, in several cases a period of extreme discomfort, fullness and cephalalgia in cases of subcutaneous injections about the root of the nose. Peculiarly these attacks appear only after the filling has become organized; that is, after the connective tissue has displaced the paraffin. The secondary tumor in such cases appears to be slightly larger superiorly than the original size at the time of injection.
The irregularity of these attacks, with edema of the forehead and slight puffing of the upper eyelids, points to a disturbance of the circulation and is undoubtedly due to pressure on the angular vessels, and the venous arch across the root of the nose. The symptoms usually appear in the early morning and moderate toward night, reappearing again the next morning or not again until the next attack, which may be expected at any time.
This condition of affairs is an unfortunate one, since we cannot look to the avoidance of the trouble nor foresee it at the time of operation. In one case the symptoms did not develop until nearly two years after the injection was made and became so troublesome that the only relief had was by opening the skin of the nose laterally and excising as much as seemed necessary of the newly formed connective tissue with a fine pair of curved scissors. None of the injected matter was discovered except two fine scalelike disks of glistening paraffin of a diameter of one sixteenth inch. These were evidently all that remained of the injected mass, and were undoubtedly held[248] in the innermost meshes of the new tissue. Immediate relief followed the operation, but no appreciable difference in the size of the tumor could be noticed.
Cold applications or ice cloths relieve the temporary pain following an injection of paraffin, but in most cases this is rarely necessary except in extremely nervous and expectant patients.
On the whole the author believes the secondary neuroses and circulatory difficulties are now practically overcome by the more conservative use of the matter to be injected, coupled with a repetition of the injection of smaller amounts at each sitting and not repeating the same until the first has become organized.
18. Redness of the Skin.—Redness of the skin following an injection of the nature under consideration was one of the early objections made by various operators.
That redness, more or less permanent, has been found in many cases in which these injections were made is true, but such redness was found particularly when the injections were those of liquid paraffin of high melting points and in which the operator was overzealous in bringing about an absolute correction of a deformity, with the result that when the paraffin had been molded and set, it was generally pinched or shaped up or outward, thus causing a great deal of pressure upon the circulatory vessels of the skin.
The redness in such cases did not appear until several days after the operation, becoming worse gradually instead of better even in spite of the efforts to reduce it by external applications. Not unusually, in the permanent cases, distended capillaries can be seen in the skin resembling the condition in acne rosacea chronica, especially when the injection had been made to correct a saddle nose.
Smith says: “Redness is present in a good many cases. I have seen a case in which the redness lasted over a year, but it gradually disappeared. There seems to[249] be a tendency on the part of nature to take care of a foreign body, and I think the reënforcement of connective tissue that grows into this mass requires an increased blood supply, and later, when the blood supply is no longer necessary, the redness will disappear.”
The latter is true where the hyperemia is either acute or subacute, but in chronic cases where the capillaries have become distended and show plainly there is little to be hoped through the effort of nature.
Eckstein, the advocate of “Hart-paraffin” method of high melting point, states that a redness of the parts develops a few days after the injection that disappears after a time, but that this redness is more marked and of longer duration when the injections are made intracutaneous instead of subcutaneous.
These injections should be made subcutaneous in all cases, and there is no excuse for deviating from this method.
With the use of semisolid and cold paraffin mixtures, as heretofore advocated, redness rarely if ever follows the injection unless undue pressure has been made, in which case necrosis is more liable to follow unless the adjacent tissue will gradually allow the mass to become relieved by a change in form and position.
Such subsequent hyperemias are not now as common as when the injections were at first attempted, and the author may say freely that they never occur when the proper method and material is used.
Paget says: “In a few cases—but only in a few—some reddening of the skin has followed the injection, and in a few this has been very slow to fade.
“The few referred to are of a record of twenty-two nasal cases, but no data is given whether the operator used paraffin of high or low melting points. F. Connell found that redness in that case continued for a year, diminishing very little in that time. It appeared on the second time after the operation for a correction of a[250] saddle nose, and remained stationary for about one month. Twenty drops of paraffin were injected. It very gradually increased, so gradually, in fact, that there is still a distinct reddened area over the bridge of the nose. On pressure this redness will disappear, but returns immediately after the removal of the pressure. A few dilated and tortuous capillaries course their way over the area. The condition is still present fourteen months after the injection.
“There has been practically no change or decrease in the redness during the last six or seven months, it is not as marked as it was during the first few months, but still requires the profuse application of face powder in order to prevent her nose from being conspicuously red.”
The above case has been cited because it is typical of such condition, and while the amount as stated was quite small, one is almost nonplussed for an explanation of the result, yet it undoubtedly must have been due to a close attachment of the skin to the underlying structures, necessitating pressure, which is known to cause it.
However, it is possible to have such redness develop weeks or months after the injections are made. In such cases it is not due to the primary pressure of the injection, but to that of the newly developed tissue which has taken its place, but which is slightly overdeveloped for the same unaccountable reason already referred to.
Almost every surgeon who has used this method of restoring the contour of parts of the face has observed redness, more or less permanent, follow the method used, but in most cases liquid paraffin of high melting points had been forced into the tissues at great pressure.
In one case, that of a southern operator, the entire tip of the nose had become injected by primary diffusion or direct filling.
It became inflamed immediately after, and some weeks later, when the swelling had subsided, the lobule was[251] found to be very hard, tense, and extremely red. Two years after the author saw this case, and the tip of the nose still appeared like a red cherry with numerous capillaries showing over its area, while the rest of the nose, although much broadened by secondary displacement of the paraffin, was natural in color.
This proves that as the pressure was relieved by absorption and displacement, the tissue took on a normal appearance, whereas in the lobule of the nose, where there was no relief from the pressure, nature could do nothing to relieve the inevitable result.
In cases where the redness is suspected it may not be too late, a day or two after the injection, to remold the mass into such form as to relieve the acute tension.
If the redness develops early, cold applications of an antiseptic nature or ice cloths can be used to advantage. Antiphlogistin or other similar preparations applied externally give good results.
Later ichthyol, twenty-five-per-cent solution, may be applied; acetate of alumen in saturated solution seems to do well. Some operators apply hydrogen peroxid, but it gives only temporary benefit. When the capillaries have become distended and the redness is practically chronic the vessels should be destroyed with a fine electric needle, using about 20 milliampères—direct current.
Sometimes when the redness is acute and seems to persist depletion of the part does some good. This is done by nicking the skin here and there with a fine bistoury and allowing the part to bleed freely. Care should be taken not to puncture the skin too deeply, so as not to allow the injected mass to escape.
In some cases it is allowable to open the filled cavity early and remove enough of the filling to overcome the difficulty, injecting later, after the filling has become organized, to make up the deficiency.
When the redness is secondary—that is, when it develops[252] after the connective tissue has replaced the paraffin—it is best to open up the part and excise enough of the tissue to overcome the pressure.
In a case where the author injected for a deep furrow in the forehead with a cold semisolid paraffin mixture, a secondary redness developed three months after the injection had been made, no redness having been noticed in the meantime. There was more or less swelling for two or three weeks, undoubtedly due to pressure phlebitis, which eventually subsided.
The redness in this case was only reduced by an excision of the tissue causing the trouble. The result was satisfactory.
19. Secondary Diffusion of the Injected Mass.—This is a condition that no operator can foretell, although it might be caused by a primary diffusion due to hyperinjection of so small an extent that it escaped the surgeon’s attention at the time.
Again, a site injected may at the time of operation present all the indications of a satisfactory result—that is, the tissues at the place of operation and its immediate vicinity appear perfectly loose and elastic; the injection being made easily and the contour of the defect being remedied either partially or entirely as the operator may desire; there being no mechanical anemia post-operatio, and no decided effort on the part of the tissues to cause primary elimination after the withdrawal of the needle; yet it is possible that, by such an injection, sufficient pressure may be caused upon some of the blood vessels within the limitations of the injection as to cause a decided reaction a few hours after the operation, as evidenced by a swelling, too great for the disturbance occasioned, and associated with all the signs of a fairly active inflammation.
It is possible that such a reaction may cause a displacement or diffusion, post-primary, of the mass injected, especially if the mass be merely vaselin or a mixture[253] of vaselin and paraffin at a melting point too low for the purpose. Nevertheless, it is practically impossible to foresee such result and the operator can only use the same care as with any or all such injections.
It is possible, when the reaction is too marked, to mitigate, to a great extent, this diffusion of the injected mass, by using such methods as reduce the inflammatory symptoms.
As a rule, these cases exhibit considerable ecchymosis after this active reaction has subsided, lasting from one to two weeks.
Secondary diffusion, as the author uses the term, signifies an extension of the injected mass beyond the intended area. This may occur in two or three weeks or be proportionate to the activity of the production of fibrous connective tissue that is supplanting the mass.
Leonard Hill has reported a case in which he injected vaselin to correct a saddle nose for æsthetic or cosmetic reasons. The result was very satisfactory to both operator and patient, and continued so for nearly twelve months, when secondary diffusion of the mass began to be noticeable. Eventually the diffusion became so great in the upper eyelids as to close both eyes completely.
The worst case of such secondary diffusion the author has ever heard of or seen came to his attention early this year. The patient had been subjected to a subcutaneous injection of oils for the cosmetic correction of an abnormal deepening of the inner clavicular notch. The injected mixture, as far as the author could learn, was made up of sweet almond, peanut, and olive oils with two others that had been forgotten. Her physician had made two injections several days apart with a satisfactory result. The reaction was trifling and the parts returned to the normal in two weeks.
Five months later the part injected became tender to the touch and began to enlarge daily. With the increase in size a gradual inflammation involved the whole lower[254] region of the anterior region about the root of the neck. Various applications were made to the part to reduce the inflammation, but at the end of ten days a region of skin that had indicated the pointing of an abscess burst, allowing the escape of about eight ounces of pus. Under the most careful surgical attention this discharge continued for about three months, until under the influence of gauze packing the wound was made to heal from the bottom, leaving an ugly irregular scar at the site of the opening. With the healing of this fistular wound, however, the size of the tumor did not diminish whatever, but continued to grow until, at the present time, one and one half years after the injections had been made, the size of this peculiar hyperplastic growth of ovate form measures nearly five inches across its horizontal diameter and three and one half inches through the vertical. It is closely adherent to the overlying thickened skin, which has undergone a yellow pigmentary change to be considered in the next text subdivision. The tumor is hard, painless, and freely movable beyond the limitation of its skin attachment and rests upon the sternal thirds of the clavicles, extending upward and forward with evidences of traction on the whole anterior skin of the neck. Laryngoscopy discloses nothing abnormal. The deformity is hideous, and necessitates a mode of dress to conceal it. The patient has not as yet been operated on for the extirpation of the growth, owing to her present physical condition, the result of melancholia.
Scanes-Spicer injected some vaselin to correct a saddle nose with satisfactory immediate result, but after several days the upper lids became slightly edematous, and soon after a small hard lump, the size of a grain of shot, was felt in the left upper lid.
Harmon Smith observed a secondary diffusion in two cases in which the abnormality in one occurred on the side of the nose and in the other at the inner canthus following the course of the angular vein.
While in the foregoing cases the difficulty may have been overcome by using the cold, semisolid paraffin mixture and reducing the amount injected, it is questionable if the diffusion could thus have been entirely overcome.
The author points to the fact that undoubtedly this fault is observed more when the tissues at the side of the nose, or about the alæ, are injected, and that the cause here is one of an unequal pressure of the parts—the skin more or less bound down above and the ungiving cartilage below.
In such cases great care should be exercised in the amount injected, and if, after introducing the needle, the tissue be found to be unduly adherent and inelastic, to withdraw the needle and with a fine tenotome divide or dissect up the skin before the mass is injected. At no time would an operator be justified to inject more than ten drops of the mass, at a single operation, into the parts referred to.
As already mentioned, there is not only danger of diffusion of the mass in such region of the nose, including the lobule and the subseptum, but there is a special danger of gangrene from pressure where the tissues are less supportative than where muscular tissue or greater mobility of the skin is found.
After the immediate attempts to reduce a reactive inflammation, nothing can be done to overcome secondary diffusion except excision of the amount not wanted. This should not be undertaken until at least three months after the time of injection.
The mass of connective tissue must be entirely excised as thoroughly as possible, and slightly beyond the border of the abnormal elevation. A sharp curette is practically of no use for this purpose, and only wounds the skin, and by reason of retentive shreds of tissue may cause infective inflammation.
The opening into the skin should be made with a fine bistoury, the skin be dissected off from the elevated connective[256] tissue, and the latter extirpated by dipping cuts of a fine small, sharp-pointed, half-rounded scissors. The operation can be done neatly and painlessly under eucain anesthesia.
The wound may be sutured with fine silk or be allowed to unite of its own accord.
It is advisable to supply a small pressure dressing, made of a circular gauze pad, over the site to assure of the best union between the dissected or undersurface of the skin and the floor of the wound.
Dry dressings are to be preferred, since moisture would tend to soften the skin and permit it to crawl, which would not improve the ultimate result.
20. Hyperplasia of the Connective Tissue following the Organization of the Injected Matter.—The overproduction of connective tissue replacing the injected mass is rarely observed, yet a few cases have been noted.
Sebileau has reported a true case of diffuse fibromatosis following an injection of paraffin. This not only included the site of the injection, but extended to the surrounding or adjacent tissue, making the secondary defect much more disfiguring than the first.
The author has observed in one case of hyperplasia following the correction of a saddle nose, that the area injected presented no unusual appearance for six months, when the nose at its middle third began to enlarge slowly until it resembled a marked Roman shape, the enlargement extending laterally and as far down as the nasogenian furrows at the end of nine months.
The injection used was a cold, semisolid paraffin mixture, and only sufficient to barely correct the defect was injected, the skin being thoroughly flexible at the time of operation.
No reason can, therefore, be given for this unusual result, except, perhaps, a peculiar idiosyncrasy of the tissues, that may be compared, somewhat, with the external tissue changes in hypertrophic or keloidal scars, especially[257] noted in the wounds of negroes—a condition for which we have, as yet, found no attributable cause.
While we cannot definitely prevent such a result, following an injection of a hydrocarbon, we may at least be sure that hyperinjection is not the cause.
The hyperplasia as exhibited in these cases is one of true fibromatosis. The microscopical examination may show the retention of paraffin in small, round, pearllike masses lying in cells of varying size, but with specimens of such tissue removed after a number of years’ standing does not show the paraffin in situ.
In a specimen taken from a chin five years after the injection of paraffin the Lederle Laboratory makes the following report accompanied by microphotographs of sections taken from the fibromatous area as shown in Figs. 288a and 288b:
“Anatomic Diagnosis.—The specimen consists of several pale, tough masses of tissue removed from the chin covered on the outside by normal skin.
“Histologic Diagnosis.—The various layers of the epidermis—i. e., the strata corneum, lucidum, and granulosum—are unthickened and practically normal. In the corium the papillary and reticular layers are apparently normal, showing no thickening nor round-cell infiltration.
“The glandular elements in this area and the hair follicles appear normal.
“Toward the deeper layers and the subcutaneous connective tissues appear isolated areas of round-cell infiltration separated by masses of fibrous connective tissue, much of which is of new formation, as indicated by the nucleated character of the elongated cells. There are areas of diffuse round-cell infiltration.
“In this portion of the corium there is also to be found a large number of vacuolated areas varying very greatly in size, and which are surrounded by membranous fibrous-tissue elements, much of which is likewise of new formation, as indicated by the character of its cells.
“These vacuoles doubtless represent the areas containing the masses of paraffin which have been split up by the new formation of fibrous tissue. Between the vacuolated areas can be seen actual infiltration by true fat cells.
“In many spots the fibrous-tissue formation has proceeded to the point of thick bands containing but few nucleated cells. Fig. 288a, which is a photomicrograph of this portion of the section, shows these changes.
“In one of the foci of round-cell infiltration which have been surrounded and invaded by bands of new fibrous tissue there are numerous giant cells of the so-called ‘foreign-body’ type. This is shown in Fig. 288b.
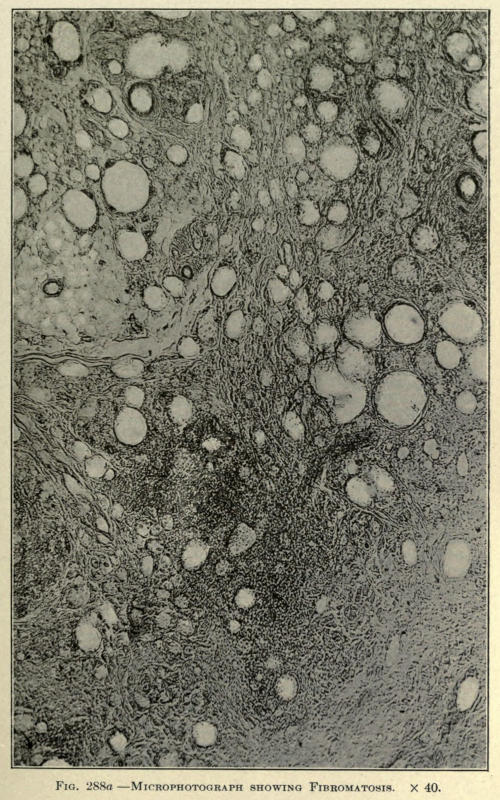
Fig. 288a.—Microphotograph showing Fibromatosis. × 40.
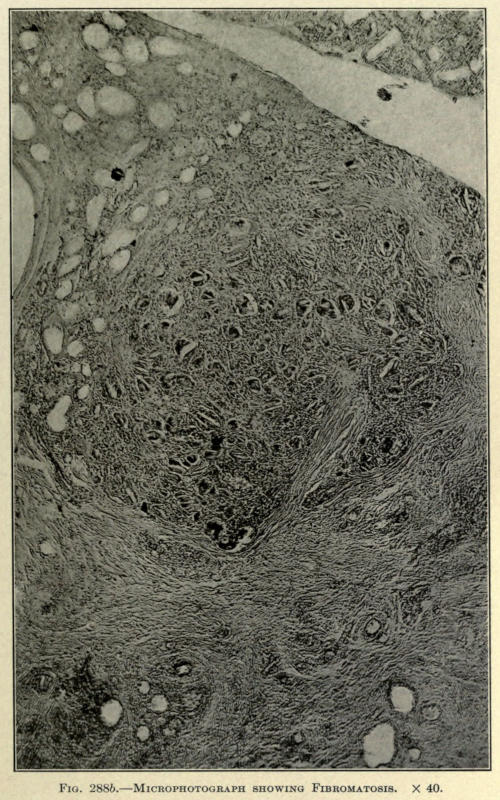
Fig. 288b.—Microphotograph showing Fibromatosis. × 40.
“Summary.—Histological Diagnosis.—Diffuse fibromatories with fatty infiltration and giant-cell formation in a vacuolated area produced by paraffin injection.”
Once the hyperplasia is established the surgeon must simply wait until he believes the activity of the abnormal growth has subsided and then remove the superabundant tissue with the knife.
With another case, in which the patient was operated on by another surgeon, the author was called upon to remove the growth. A part of the coarse, yellowish pale and cartilagelike tissue was excised, sufficient to restore the parts to a normal contour. After an uneventful recovery the patient went away, greatly pleased, only to return in six months, presenting a similar condition as before the extirpation.
A second operation was done, this time more extensively, the entire yellowish connective tissue being removed by the aid of a long median incision on the anterior aspect of the nose.
The wound healed readily and showed very little scar, and the patient was discharged. One year after the last operation the nose was still normal in appearance and the growth had not reappeared.
From this it is deemed absolutely necessary to remove[259] practically all of the newly formed tissue to warrant a nonrecurrence of the fibromatosis.
21. A Yellow Appearance and Thickening of the Skin after Organization of the Injected Mass Has Taken Place.—This condition of the skin is evidenced some time after the injected mass has become organized, beginning about the sixth month after the time of injection. It has been especially noticed with the hard paraffin fillings of the nose, but also with other injections, even of the lowest melting points, about the sternoclavicular regions of the neck.
The skin becomes at first streaked with a superficial and irregularly defined patch of red, the forerunning indication of the size of the ultimate pathological change. The red color subsides slowly, leaving the area pale, which thereafter gradually thickens, taking on the appearance of a light yellow stain in the skin.
Practically opposite to the condition in xanthalasma, where the yellow area is slightly elevated and occurs in the loose tissue of the eyelids.
The cause seems to be a degenerative change in the skin dependent on pressure upon its underlying tissues. Evidently the pressure of an overproduction of the connective tissue which has sprung up to replace the injected mass.
Seemingly the cause is due to an injection being made too close to the derma where the latter is bound down to the subcutaneous tissue, or a desire on the part of the surgeon to prevent an injection into the deeper areolar tissue, especially when the injection is made in the vicinity of the larger blood vessels, for fear of causing embolisms or phlebitis.
Excluding the use of hard paraffin for such injection, the operator should be sufficiently experienced to use these injections properly and without fear, and at all times avoid injecting into the skin instead of subcutaneously.
Making the puncture first and observing if blood[260] flows freely or trickles from the detached needle will assure the operator into what tissues he has thrust his needle.
Should active bleeding follow the puncture, he should withdraw the needle and wait to inject the site at a later sitting, using the same precaution; at no time should he be in doubt as to the absolute placing of the injected mass.
When the injections are done about the lower neck or shoulders great care must be exercised to avoid the blood vessels, and small quantities be only injected to prevent reactions that may cause phlebitis of these vessels; furthermore, the injected mass must be carefully molded to prevent the formation of uneven elevations or lumps. Without doubt an injection into one of the blood vessels of the neck would mean certain death.
Kofman lost a patient by pulmonary embolism twenty-four hours after an injection of 10 c.c. of paraffin. How many punctures he made to inject this amount is not stated, but certain it must be that he introduced part of the mass directly into some blood vessel.
The author advises, when injecting about the neck, to use a stout, dull-pointed needle introduced under local ethyl chloride anesthesia and to elevate the tissue with the needle as the injection is made. In this way the operator can observe the behavior or placing of the injected mass, at the same time stretching the skin to permit of the injection without encroaching upon the blood vessels. The mass is immediately molded after each injection. The further question of the practical method of making these injections will be fully considered later.
If, however, the pigmentation under consideration has taken place, electrolysis with a fine needle may be resorted to, with the object of whitening the discoloration by producing scar tissue, in the form of punctations, in the discolored area.
While the numerous white spots so caused are objectionable, they are better borne by patients than the pigmented appearance. A thorough needling of the spot in this way eventually brings about an improvement, and if, for æsthetic reasons, the patient objects to the unsightliness of the result thus obtained, the white area may be carefully tattooed with an appropriate color to match the rest of the skin of the face or neck.
If the pigmented area is not too large, it can be excised with the knife and the healthy skin be brought together with a fine silk suture, thus leaving a thin linear scar which can be dealt with as the punctate scar area, if desired; the electrolysis being a painful procedure at all times, since sufficient milliampères must be used to cause scar-tissue formation, which is between 20 to 30 milliampères in such cases.
22. The Breaking Down of Tissue and Resultant Abscess Due to the Pressure of the Injected Mass upon the Adjacent Tissue after the Injection Has Become Organized.—The above result is particularly noticeable when the injections have been made into the cheek or the breast. It is understood that the suppurative changes under consideration herein are not attributable to imperfect sterilization of the injected matter, although it is possible, and perhaps is the cause in fifty per cent of the suppurative elimination of the infected mass from the cheek, that a nucleus of infection is carried into the tissues and is held in suspense for a time, because of its imbedment in a neutral media that does not readily permit of bacteriological propagation, but eventually this nucleus must come in contact with tissue which it can affect, and only then may its infection be taken up.
The author believes that such secondary affections are accountable to pressure effects upon the blood vessels or glandular structure, as in the case of breast injections, the new connective tissue causing a lack of nourishment in the part or gland, and a resultant breaking down of the[262] tissue, directly influenced in some instances by external violence.
Tuffier reports the elimination of paraffin injected into the breast several weeks after the injection. If this elimination had been caused by primary infection an acute reaction would have taken place at least within forty-eight hours, ending in abscess shortly after.
A case which came to the author’s attention was that of a lady who had been operated upon for the correction of a saddle nose three months before. The result had been satisfactory. The day previous to consulting the author she had injured her nose in an automobile accident. The nose was much swollen, very painful, and red over the entire upper and middle third. The use of external cold did not relieve the condition much, and on the fourth day the skin broke open at one point, allowing pieces of the paraffin to escape. Immediate relief followed, the wound healed with a marked sinking of the middle third of the nose. After three weeks the nose was again injected with no further untoward symptoms, the result being satisfactory for two years past.
In this case undoubtedly the exciting cause was directly due to violence, which may be the forerunner in many of such cases, but there is a number of such eliminations directly due to a breaking down of the tissue from internal pressure alone.
There is no way to overcome this difficulty, except to await the definite formation of the abscess and then to puncture the skin directly over the soft fluctuating area and to drain the cavity.
Once relieved, the condition quickly subsides, leaving a certain amount of loss of contour, which can, however, be corrected several weeks after by a secondary injection.
When the abscess occurs in the cheek it is not advisable to open interiorly, but to make the puncture through the skin, on account of the danger of infection from the[263] buccal cavity and of the imperfect evacuation thus attained.
A trocar and cannula of proper size will be found to be the most suitable, the parts being gently manipulated to evacuate the contents of the abscess.
Aspiration can also be resorted to, but for the breast a small linear incision, made under local anesthesia at the most dependent point, best answers the purpose.
A small gauze strip drain may be employed for a few days to insure of perfect drainage in the latter case, the wound being brought together eventually by a delicate cosmetic operation if desirable.
Although Gersuny advocated the use of a Pravaz syringe for injecting the liquefied vaselin mixture for prothetic purposes, it was soon found that such an instrument was practically useless, especially when the parts to be injected offered more or less resistance to the introduction of the foreign matter.
Other operators, following the advice of Eckstein, who advised the employment of “Hart paraffin” of high melting point liquefied by heat, raised the objection that the metal needle became so easily obstructed by the rapid setting of the paraffin in its distal end that the great force necessary to eject the contents of the syringe usually resulted in a breakage of the glass barrel in the hands of the operator, or, as in some types of the syringe, a separation of needle and syringe at the point where the former was slipped upon the ground point of the latter, with the annoyance of the paraffin squirting over the faces of both patient and operator.
Eckstein tells us how to overcome the first difficulty with this same style of syringe as used by him. He covers the syringe with a rubber insulating sleeve and draws[264] several drops of hot, sterilized water into the needle to overcome the plugging up of the latter; an illustration of his syringe has been shown on page 232. Mention has also been made of the various methods used to overcome this difficulty by other operators.
It was presently found that such an instrument was not only impractical, but also a detriment to procuring desirable results, the paraffin solution shooting out suddenly, in some instances causing hyperinjection, and at other times emerging so slowly that it required unusual force on the part of the operator—a painful procedure for delicate hands, inasmuch as the fingers only can be applied to operate the instrument.
With the object of overcoming this uncertainty of the amount of the injection and the unnecessary exertion to inject any given quantity, as well as to establish enough vice à tergo to keep the needle free from plugging up with cooling paraffin, various operators devised instruments, all having practically similar points of mechanical merit and usefulness. The required necessities being to invent a syringe which would have a known capacity, a piston under control of the operator at all times, and metallic needles of proper lumen, to prevent the solidification of the liquid paraffin, screwed to the syringe to prevent loosening.
With the object of overcoming these difficulties the author devised a syringe which was made for him by Tiemann & Co., early in 1902. He begs to introduce the same here, as a type similar to which most operators have built their special instrument.
The syringe at that time consisted of a glass barrel, of a size to hold 6 c.c. of liquefied paraffin. At either end of the barrel tube were placed metal ends, the distal one containing a cap with a screw thread to receive the needle, the upper cap being threaded to receive a check nut through its center and on its outer surface, on opposite sides to each other, two metallic rings to accommodate[265] the thumb and forefinger. The center of the check nut was double threaded to receive the piston rod, the piston or plunger being held in place by two, upper and lower, washer nuts, the lower being threaded to receive a small rod passing through the bored-out center of the piston rod, and which ended in a check nut, in the handle, threaded upon the outer or manual end of the piston rod, in such a way that the fiber or asbestos piston washer could be tightened and loosened at will.
The syringe permitted of being used as an ordinary syringe by unscrewing the cap check nut or be made into a screw drop syringe by screwing the same nut into place. By turning the handle end of the piston rod the contents of the syringe were forced out smoothly and evenly in any quantity desired.
With the later employment of the cold, semisolid preparation of vaselin and paraffin, as heretofore considered, it was found necessary to reënforce this syringe, so that the greater pressure necessary to eliminate the wormlike thread of hydrocarbon would not force off the lower cap or break the barrel of the syringe at its needle end.
This was done for the author by the Kny-Scheerer Company, December 6, 1902, when metallic strips were added to opposite sides of the glass barrel connecting the lower with the upper cap.
The instrument as then made is shown in Fig. 289.
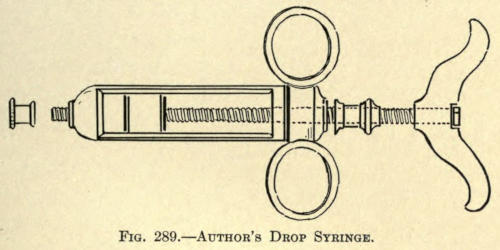
Fig. 289.—Author’s Drop Syringe.
At the same time the same firm made the author a syringe entirely of metal, similar in construction, except that the barrel was made larger in diameter and shorter in proportion to bring the instrument near to the seat of operation. The regulating washer rod was not needed, since in this instrument no washers were required, the piston head being made of solid metal throughout and the rod being soldered to the plunger, thus overcoming any objectionable fault in sterilization.
This type of syringe was found to be most suitable for the cold, semisolid injections, and is of the type now universally used except for the slight modifications of the various operators. It is illustrated in Fig. 290.
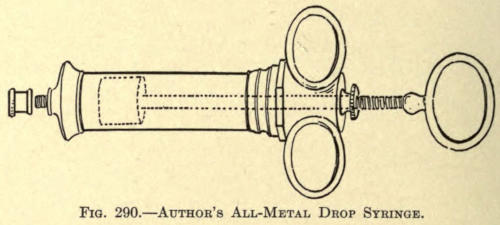
Fig. 290.—Author’s All-Metal Drop Syringe.
Since there were no objections to making the barrel large enough to permit of injections, such as are required for restoring the contour of the cheek and the neck and shoulder, it was made to contain 10 c.c. working capacity, overcoming the necessity of constant refilling, when comparatively large injections had to be made—a fact worth remembering from a practical standpoint, although two or three of these syringes, specially prepared for each patient, might be found desirable by some operators. Yet the simplicity and ready facility with which this instrument can be used and refilled renders it useful and sufficient for performing operations of this nature to any judicious extent.
Syringes holding small quantities of the paraffin mixture are found to be a nuisance.
The following operators employ syringes of the capacity given:
| Brœckært | 3 c.c. | 50 mm. |
| Eckstein | 5 c.c. | 80 mm. |
| Freeman | 5.6 c.c. | 90 mm. |
| Downie | 10 c.c. | 150 mm. |
The instrument employed by Brœckært, holding less than one dram, would be of little use except to correct very slight deformities about the brow or nose, or dressing up or completing the contour of parts previously filled by larger injections.
Another syringe similar in type to the author’s, but of a capacity of 5.6 c.c., was introduced by Harmon Smith.
The principles of the syringe are alike, but the style of handles, two flat metal bars at opposite sides, offers no objection when comparatively hard mixtures of paraffin and vaselin are used.
While operating the syringe the narrow blades are brought in contact with the soft flexor sides of the thumb and forefinger, indenting the flesh deeply, and with the least unexpected move on the part of the patient permitting it to slip out of the grasp of the surgeon. Its incapacity for large injections also offers some objection,[268] but for correcting smaller defects it is both practical and compact. It is illustrated in Fig. 291.
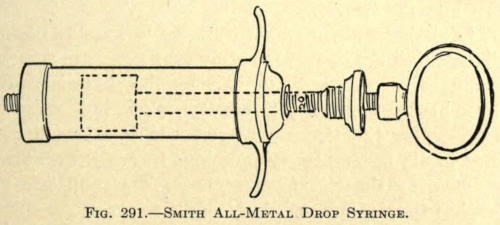
Fig. 291.—Smith All-Metal Drop Syringe.
It is obvious that with the screw drop type of syringe the cold semisolid paraffin mixture contained in its barrel is always under the full command of the operator, nor can there be a plugging of the needle, since the great force that can be exerted with a turn of the piston handle would free it, even if the mixture were of a comparatively high melting point, although the force to be applied would naturally increase in proportion to the hardness of the mass within the syringe.
The turning of the screw piston forces out the contents of the syringe in the form of a white thread of a diameter equal to the diameter of the lumen of the needle.
To facilitate this ejection, the needles should be of ample diameter, not over one inch long and having knife-edged points. Longer needles are not necessary, and only add to the force required to turn the screw handle.
Curved needles, used by some operators, are never needed, and the author does not see how they could be applied at any time in preference to the straight.
As much of the paraffin mixture can be forced out of the syringe as may be desired by screwing the piston down into the barrel.
The piston rod may be graduated in five- or ten-drop divisions, but the operator rarely ever refers to the scale. He judges the amount required by the elevation of the tissues brought about by the presence of the paraffin thus forced under the tissue. Experience soon teaches him the amounts necessary or judicious in each case, always remembering that it is better to do a second and later injection than to hyperinject.
The entire instrument being of metal permits it to be sterilized as readily and in the same manner as any other metallic instrument.
It is understood that the syringe must be taken apart for sterilization at all times.
Lubrication, to facilitate operation, is never required, since the nature of the mixture used in the syringe answers this purpose in every way.
Owing to the greater amount of metal in the solid piston itself, the latter is very likely to expand under dry heat sterilization or boiling, so much so that for a moment it cannot be introduced within the barrel. This can be quickly overcome by dipping it into cold sterile water or absolute alcohol, which brings about its contraction.
After using, the syringe should be emptied entirely, unscrewed and sterilized, and placed in the metal case furnished for it. A screw cap is furnished to take the place of the needle when not in use.
The method of filling and using the syringe will be considered later.
The same surgical precautions should be observed when a paraffin injection is to be undertaken, as with a minor surgical operation.
It is hardly found necessary to prepare the site of operation the day before, nor need the patient be detained for such time for the purpose of making him ready.
With careful observance of ordinary surgical technique, both as to surgeon and patient, all of this class of operations can be performed in any physician’s office, providing that both instruments and the mass to be injected have been rendered sterile.
Especial care should be given to the operator’s hands, for with these he not only handles the instruments, but must also mold the mass injected, thus frequently coming in contact with the needle opening or openings made in the skin.
When injections are to be made in the cheeks of the patient, the mouth should be prepared by cleansing the[270] teeth thoroughly and washing out the buccal cavity with warm boric acid or hydrogen peroxid solution, or any of the preparations of the Listerine composition.
This rinsing should be continued every few minutes for at least ten minutes before the operation is undertaken.
This is necessary, as the surgeon must introduce his finger into the mouth and behind the cheek to mold out the mass injected subcutaneously, and infection could easily be introduced by his fingers during this procedure.
Externally a generous field of the operation is scrubbed with a brush dipped into green soap and water.
The skin is then thoroughly washed with gauze sponges steeped in absolute alcohol, followed with spongings with a 1-5,000 solution of bichlorid of mercury. The whole surface is then wiped off with a sponge dipped in ether and covered for the time being with a pad of sterilized gauze until the operator is ready to proceed with the operation.
The manner of preparing the necessary mixture of paraffin has been described on page 244. After such preparation, the mixture, still hot, may be poured into test tubes, which are sealed and put away for further use, each tube holding just enough to fill the syringe two thirds full.
When a syringe is to be filled, one of the tubes is opened and the contents are again boiled over a spirit flame, or simply liquefied and poured into one of the types of heaters already described for the same purpose of resterilization.
From the test tubes or the heater, the boiling mixture may be drawn up into the sterilized syringe to the required amount or it may be poured into the opened piston screw cap end.
In the latter event the ready cooling of the mixture as it enters the needle will permit it to be retained in the barrel, or the needle may be immersed in sterile water as the paraffin is poured into the syringe, yet even if a few drops escape from the needle in the former method, no harm is done, as such loss amounts to nothing and helps to eventually fill the syringe evenly and free of air.
If the mixture is drawn up into the barrel to the required height, more or less air enters, which must be removed by turning the syringe, needle up, and screwing up the piston rod until either the liquid or cylindrical thread of the cooled mixture appears.
If the mixture is poured into the syringe the piston is slowly pressed into the barrel, thus allowing the air to escape along its sides if the mixture is set, or if warm the syringe is turned up and the piston screwed into place. As this is done the few drops of cooled paraffin will be forced from the needle before the air is exhausted. The screw is turned until the paraffin emerges evenly from the needle.
The syringe must now be laid aside, or placed in sterile water of the temperature of the room, to allow the liquid within to set evenly and become uniform in consistency.
The operator will follow what method he pleases in filling his syringe, but at no time should he fill it with the cooled product with a spatula, or other such means, as he is sure to fill it unevenly in this way, incorporating a number of air spaces. The air issues from time to time during an operation with sudden sputtering outbursts, that not only tend to annoy the patient, but also to frighten him—the shock being unusual and unexpected, while the air thus forced into the subcutaneous tissues puffs out the parts and interferes with a perception of the proper amount to be injected and adds to the danger of air embolisms.
Slipshod methods are inexcusable, and should not be[272] tolerated. The best results possible should be given the patient, and only from the best results obtained with the best care can the most reliable data be attained, all helping to fix the reliability, efficacy, and exactitude of this branch of cosmetic surgery.
The field of operation and the instruments having been properly prepared, as described, the modus operandi must next be considered.
Since the various parts of the face to be injected demand specific procedure, they will be considered somewhat individually hereafter, whereas the general technique, applicable in as far as the method of injection is concerned and applying similarly in all cases, may tersely be first taken up.
Various and noted surgeons point out that these subcutaneous injections should be made under general anesthesia, i. e., ether, while others consider the hypodermic use of cocaine or Eucain β solution in one to four per cent necessary to accomplish good results.
The author considers the method in the first case objectionable both as to patient and operator, entailing much discomfort to the one operated on and demanding an unnecessary waste of time for the etherizing and recovery. Likewise is the employment of a local anesthetic not indicated or demanded, since the operation to be undertaken necessitates only the pain associated with the prick of the needle through the skin.
The objection to etherization is obvious, while the hypodermic employment of any local anesthetic, by the very fact of its presence of volume and its physiological action upon the tissue, tends to interfere with the proper injection of the parts by reason of temporary swelling of the parts, not caused by the later injections of the prothetic mass.
If in nervous irritable patients an anesthetic is required to allay fear it is best to use the ethyl-chlorid spray upon the skin sufficiently to overcome the sharp sting of the needle insertion. For this purpose the ether spray is used only to the point of blanching the skin, and no longer.
This mode of procedure is especially useful when a number of injections are to be made, as in the rounding out of a cheek or of the shoulders, in which the contour cannot be restored from one point of injection, as will hereinafter be described.
The patient, being now in readiness, the skin over the area is lifted or pinched up with the fingers of the left hand of the operator as a guide to its mobility and to steady the part.
The point of the needle is now forced through the skin and into the subcutaneous tissue at a point along the periphery of the deformity and pushed a little beyond the center of the cavity to be filled.
The elevation of the skin is in the meantime partly kept up with the needle itself, while the syringe is grasped with the freed hand, the thumb and forefinger of the right hand being placed upon the handle of the screw or piston rod, which they must rotate to force the semisolid mass from the instrument.
Before beginning the injection an assistant is instructed to press with his fingers the tissue about the margin of the defect to prevent the filling from becoming misplaced or being forced into undesirable channels, especially if the skin over the defect is found to be thick and inelastic.
The screw handle is now rotated evenly and slowly, discharging the mass to be injected, which will soon be evidenced by the rise of the skin over the depression to be corrected.
Only sufficient of the mass must be injected to fairly correct, never to overcorrect, the defect.
Experience alone will assure the surgeon when this point has been attained, since he cannot immediately judge the necessary amount injected, as it will appear as a round or irregular lump under the skin, until it has been molded or worked out into shape.
Owing to the pressure exerted upon the contents of the syringe, which will continue to emerge from the needle for a time, the needle is left in place for a few seconds before withdrawal, so that the needle canal through the skin will not become filled with the semisolid mixture.
Such blocking up of the opening causes a cystic development or enlargement about the opening in the skin by this backing up or exuding, ofttimes crowding itself in between the layers of the skin and necessitating later removal with the knife. If not this fault it tends to keep the wound open unnecessarily after the operation, preventing healing and permitting the escape of a certain amount of the injected mass, if a mixture of low melting point has been utilized.
The needle, having been allowed to remain as advised, is now withdrawn. The tip of one finger is placed over the opening in the skin and held there gently, but firmly, while the mass is molded into the shape required or desired with the fingers of the right hand.
If it now appears that the injection is insufficient the needle may again be introduced through the same opening and more is injected, remembering, however, that if the correction is quite normal no more should be added for several days, or until the injected mass has become organized, which should take place in about three weeks.
If it is found that the skin over the defect is inflexible and bound down, it will be found advisable to sever or dissect subcutaneously the adhesions that bind it down with the use of a fine tenotome or a spear-headed paracentesis knife.
This may be done two or three days before the parts are injected to assure the surgeon of an absolute cleanliness of the wound.
Mayo advocates the injection of a saline solution into subcutaneous wounds thus made as a guide to the extent of dissection and to further loosen the tissues.
When the parts, thus loosened, show little tendency to bleed, the author advocates immediate injection, as the waiting for several days permits the throwing out of new connective-tissue cells that interfere to a certain extent with the proper injection of the part.
It is with such wounds that secondary elimination is most likely to take place, especially if “Hart paraffin” or paraffin of a high melting point has been employed.
This is undoubtedly due to the healing down and contraction of the margins of the wound, which seems to progress more and more, encroaching eventually upon the hard mass and ending in inflammation of the overlying skin and ultimate elimination. With injections of softer consistency this is less frequent and, in fact, may be entirely overcome by limiting the amount of the injection at the first sitting, relying upon a full correction for later operations, when the periphery of the wound has become more or less influenced by the presence of the neutral mass between the wounded surfaces.
The subcutaneous dissection referred to must, of course, be done under local anesthesia, preferably the Schleich mixture or a one-per-cent solution of Eucain β.
The injection of the paraffin, or hydrocarbon mixture, in semisolid form, having been made and properly molded into shape, is set or fixed by spraying the part with ether or by the application of sterile ice cloths. When liquid paraffin has been injected it will be noted that the paraffin in setting contracts upon itself considerably, leaving less of a correction than anticipated.
The needle opening in the skin is next washed off[276] with a twenty-five-per-cent solution of hydrogen peroxid and closed over with a drop of collodion.
The patient may then be discharged for the time being, with the instruction to apply ice cloths to the part for at least twelve hours to reduce, as far as possible, the reactive resultant inflammation.
On the third day the collodion patch may be removed and replaced with isinglass adhesive plaster applied with an antiseptic solution. The latter is allowed to remain on the skin until it falls off.
Reference has been made heretofore to the general indications for which subcutaneous injections of paraffin or its compounds may be employed. With the object of systematizing such indications and to further bring out the practicability and judicious use of the method under consideration the author submits the following tabulated arrangement, with the hope that it may lead to a more concise and better knowledge of the possibilities within the reach of the plastic or cosmetic surgeon.
The face will be considered in such grand divisions as are easily and readily understood, the defects of each part being shown under its distinctive regional heading.
| Transverse Depressions | { Punctate. |
| { Linear. | |
| Deficient or Receding Forehead: | |
| (Exhibition of Undue Superciliary Ridges.) | |
| Unilateral Deficiency | { Surgical (Frontal Sinus). |
| { Traumatic. | |
| Interciliary Furrow | { Single. |
| { Multiple. | |
| Temporal Muscular Deficiency | { Unilateral. |
| { Bilateral. |
| Anterior Nasal Deficiency | { Superior Third. |
| { Middle ” | |
| { Inferior ” | |
| { Superior Half. | |
| { Inferior ” | |
| { Total. | |
| Lateral Insufficiency | { Unilateral. |
| { Bilateral. | |
| Lobular Insufficiency. | |
| Interlobular Deficiency. | |
| Alar Deficiency | { Unilateral. |
| { Bilateral. | |
| Subseptal Deficiency | { Partial. |
| { Complete. |
| Labial Deficiency | { Upper Lip | { Unilateral. |
| { Median. | ||
| { Bilateral. | ||
| { Lower Lip | { Unilateral. | |
| { Median. | ||
| { Bilateral. | ||
| Nasolabial Furrow | { Unilateral. | |
| { Bilateral. | ||
| Oral Angular Furrow | { Unilateral. | |
| { Bilateral. |
| Deficiency of Cheek | { Total | { Unilateral. |
| { Bilateral. | ||
| { Partial | { Unilateral. | |
| { Bilateral. |
| Anterior Mental Deficiency | { Partial. |
| { Total. | |
| Lateral Mental or Angular Deficiency | { Unilateral. |
| { Bilateral. |
| Pro-auricular Deficiency | { Unilateral. |
| { Bilateral. | |
| Post-auricular Deficiency | { Unilateral. |
| { Bilateral. |
| Supraclavicular Deficiency | { Unilateral. | |
| { Bilateral. | ||
| Infraclavicular Deficiency | { Unilateral. | |
| { Bilateral. | ||
| Interclavicular (Notch) Deficiency. | ||
| Supra-acromion Deficiency | { Unilateral. | |
| { Bilateral. | ||
| Infra-acromion | { Unilateral. | |
| { Bilateral. | ||
| Supramammary Deficiency | { Unilateral. | |
| { Bilateral. | ||
| Mammary Deficiency | { Partial | { Unilateral. |
| { Bilateral. | ||
| { Total | { Unilateral. | |
| { Bilateral. | ||
| Supraspinous Deficiency | { Unilateral. | |
| { Bilateral. | ||
| Infraspinous Deficiency | { Unilateral. | |
| { Bilateral. | ||
| Interscapular Deficiency. |
Punctate Form.—Such deficiencies are either of sharply defined depressions in a part of the frontal bone due to congenital malformation or of traumatic origin.
In the first instance they are usually unilateral or median and rarely ever bilateral. In those of the second class the deformity may be median, but is more often found to be unilateral.
Linear depressions of the forehead are usually found to be congenital, although traumatism in the form of direct violence may be the cause, as, for instance, the kick from a horse or a severe blow or fall.
The acquired linear form of lack of contour is found in people of middle life given to undue use or corrugation of the forehead, as in frowning.
The correction of this class of deformities may be accomplished by carefully raising the depressed area by repeated injections of small quantities, always avoiding the frontal and supra-orbital vessels.
At no time should such a deformity be corrected in one sitting, unless when the defect is a congenital one of small moment.
The reaction following these injections, owing to the close attachment of the integument to the bone, is usually found to be more severe than where the skin is more loosely attached.
In traumatic cases the scar attachments should be freely liberated, under eucain anesthesia, by the aid of a fine probe-pointed tenotome, before the cold paraffin mixture is introduced.
In such event only one opening should be made and just enough of the mixture be injected to raise the skin to its normal contour, if this be possible. Generally, later[280] injections are required, and these may be made without further dissection. They should not be undertaken until the incised wound made with the tenotome has healed thoroughly, otherwise the pressure of the injection is liable to burst through the delicately healed wound, and thus delay if not endanger the success of the first operation.
When the reaction following such injections be severe, associated with considerable edema, cold pack or ice cloths should be applied or resort may be had to hot applications of antiphlogistin. The patient should be kept on his feet during the day and sleep with the head high at night. The bowels should be kept open, and general tonics be given if indicated. The patient usually returns to the normal, except for a little tenderness about the forehead, in three or four days under the treatment outlined.
In this condition there is usually a transverse lack of contour across the forehead above the superciliary ridges, giving the patient a degenerate appearance. The defect is congenital and is to be corrected, as described in the foregoing division, although the injections may be at either outer or temporal end of the forehead, gradually being brought nearer to the median line until the contour of the whole forehead has been raised by subsequent injections.
This defect may be traumatic—the result of direct violence, but is more commonly due to a frontal sinus operation.
In both events it will be found necessary to detach the cicatrices that bind the skin down to the injured bone, before a prothetic injection may be undertaken.
In some cases where the cause of the deformity has[281] been moderate and the scar is linear and of long standing the injection may be undertaken without subcutaneous dissection.
Several injections are necessary, as the tissue about such parts is usually much thickened, apart from the firmness added by the scar tissue.
A short stout needle should be employed, the puncture being preferably made under ethyl-chlorid anesthesia, as the pressure necessary to raise the tissue causes considerable pain.
To further facilitate the injection the operator should raise the skin with the needle introduced subcutaneously.
Only one injection of small amount (10 to 15 drops) should be done at a sitting. The injected mass, unless too easily introduced, and thus forming a tumefaction, need not be molded out, since the pressure of the skin overlying it will accomplish it more satisfactorily, while the pressure required in molding tends only to press out more or less of the mass, thus lessening the benefit of the operation.
A second sitting must be undertaken in not less than one week, or even later, if a subcutaneous dissection has been done.
The secondary treatment should be followed as heretofore described. The reaction, for even a small injection in these cases, is usually considerable.
This deformity is usually spoken of as a frown. It may be said to be congenital, when it appears in early life, but is commonly acquired through the habit of frowning.
The furrow may be a simple linear one or made up of a number of furrows. The author has been called upon to correct one made up of six distinct furrows.
The furrows or creases radiate upward and outward, conelike from a point beginning at the root of the nose.
In the correction of this common deformity the operator is tempted to overdo the fault by hyperinjection. A single furrow is readily corrected by a few drops of the injection, which should be neatly smoothed out. A little of the mass at this part of the face seems to accomplish considerable; in fact, the part seems overcorrected for some time after a judicious and carefully done operation, which is undoubtedly due to the active reaction that follows such cosmetic procedure, owing to the close proximity of the frontal veins and those of the venous arch at the root of the nose, which undergo more or less phlebitis of a mild type, the resultant edema depending upon the pressure caused by the mass on these vessels. The intimate relation and anastomoses of the latter is clearly shown in the carefully prepared dissection represented in the frontispiece.
In injecting, the needle should be introduced at a point directly at the root of the furrow or furrows—that is, at the junction of the forehead with the nose.
A needle one inch long should be used, taking care not to puncture any of the veins which are found to be very differently placed in various patients. If blood flows from the needle puncture, no injection should be made at that point, but another be chosen which does not give such result, preferably at a later sitting.
The needle should be introduced well upward under the skin so that its point corresponds to the point of greatest depression.
The injection should be made slowly and continued until a tumor, judged to be sufficient to overcome the major deformity when molded out has been formed.
This knowledge can only be gained by experience, and the operator must be cautioned to underinject rather than cause undue prominence of that part of the face.
If, however, his judgment has not been accurate enough, the operator can immediately thereafter squeeze out enough of the filling to give him the desired correction.
If more than a single furrow is to be corrected, he may inject the two center ones, leaving the outer for later operation.
In multiple furrows the injections must be made in conelike form, to give a normal contour to the forehead. The apex of such cone corresponding to a point at the root of the nose, and the base to an arc with its greatest convexity near the median hair line of the scalp, depending upon the length of the furrows.
The injections in such cases should be made at least three days apart, two being made at each sitting, after the central or two inner depressions have been raised by the first operations. These later injections should be made to relieve the furrows lying next to the median, gradually working out to each slant side of the cone until the contour of the middle forehead has been made normal.
Never superimpose an injection about the median line until the major defect in general has been overcome, and only then when the first injections have become settled and organized, as such untimely disturbance is liable to set up considerable reaction, with enough induration and resultant new connective-tissue formation to cause a decided lumpy or protuberant appearance of the part.
The mixtures of low melting points should be preferred to the harder variety in frown corrections. They lend themselves to better molding, and seem to undergo organization with less pathological change than those of the latter class.
When the injections must be made over the inner third or half of the eyebrows, as is often the case, they should be made well above the hair line and molded out in an upward direction, to avoid the dropping down of[284] the mass into the upper lids or to prevent the resultant displacing connective tissue from involving them.
If the upper lids do become involved, as shown by fullness, hardness, and partial ptosis, the connective tissue causing the same must be carefully cut out from the lid by a transverse semicircular incision made in the upper lid along the line of its backward fold or hinge. If need be, an elliptical strip of the skin of the lid may be removed at the same time to give better scope to the extirpation under consideration.
The author has recently corrected two such cases where a surgeon had hyperinjected the entire forehead with a combination of oils at one or two sittings. The resultant involvement and later discoloration of the lids at the end of a year’s time might have been expected.
Such wounds, when neatly sutured with No. 1 twisted silk, leave surprisingly little scars; in fact, the cicatrices are rarely ever detected a few days after healing has been established.
The treatment post-injectio for all furrow protheses should be as already laid down.
Apart from general surgical cleanliness and an antiseptic powder, the blepharoplastic operation mentioned required no special attention. The sutures may be removed in forty-eight hours.
This facial defect while possibly unilateral, as in hemiatrophy, is generally met with in the bilateral form due to either hereditary causes or a lack of nourishment of the parts, the latter usually involving the greater part of the face. Chronic diseases and the cachexia dependent upon disease may be the origin, in which the deformity is rarely ever overcome entirely by internal treatment and massage of the parts; if anything, massage[285] tends to elongate the skin about the temples, causing a worse disfigurement in the form of numerous fine furrows.
The correction of the defect under consideration may be readily overcome by repeated and careful injections of a hydrocarbon of low melting point.
The author prefers the use of sterilized vaselin injected in its cold state. The use of paraffin of high melting points or its compounds is not advisable, and if employed leaves the temples uneven or lumpy, due to the unequal organization or new tissue formation caused thereby, at the same time causing sagging of the skin of the adjacent parts, particularly the upper eyelids, owing to the added weight of the new tissue growth occasioned by such preparations.
Contrary to general expectation, this part of the face is readily injected and corrected.
The skin should be pinched up with the thumb and forefinger of the left hand and the needle introduced with the right hand in such way as to exclude the puncturing of blood vessels.
To assure the operator against such difficulty the needle may be withdrawn after insertion, and if blood does not trickle from the wound it may be reintroduced without pain to the patient and the injection begun.
It is not advisable to correct the defect at one sitting. One third or one half of the depressed area may be overcome by one injection. The resultant tumefaction must then be thoroughly molded out, until little seems to have been accomplished by the injection.
The operator trusts in these particular cases more to the development of new connective tissue than in any other part of the face, except perhaps in the correction of an interciliary furrow. It is surprising how much is attained by the most conservative injections in and about the temples.
The molding of the injected mass must be done in a[286] superio-posterior direction to avoid forcing it into the upper eyelids, resulting in the same overdevelopment previously referred to.
Both temples should be injected as advised at one sitting. The use of the ethyl-chlorid spray makes the operation less fearful to the patient.
Subsequent injections should not be done earlier than three weeks or until any discoloration of the skin of the parts has disappeared. The latter is not an unusual occurrence, and is undoubtedly due to the pressure of the injected mass upon the numerous blood vessels found there.
The post-operative treatment should be followed as heretofore advocated.
The use of hydrocarbon protheses for the correction of nasal deformities has revolutionized, to a great extent, the rhinoplasty of many centuries. Through their employment many unsatisfactory cutting operations have been entirely displaced, and it is quite right to hold that the introduction of other subcutaneous protheses and like apparatuses of amber, celluloid, caoutchouc, silver, gold, aluminium, ivory, or other nature have been supplanted by this method of operation, when these were needed to correct a partial deformity of the nose.
When a total rhinoplasty has to be undertaken the paraffin group of protheses of course cannot be resorted to, owing to a lack of the necessary retentive walls of tissue, except perhaps in such cases where the so-called double flap, or French method, is employed, and there only after the parts have become thoroughly organized.
A somewhat complete tabulation of nasal defects has been given heretofore which gives an excellent idea of the extensive use these hydrocarbon injections may be put to.
Such nasal deformities as are amenable to this method of correction may be due to either congenital causes, lack of development, direct violence, ulcerative changes following catarrh, syphilis, and tubercular disease. In some cases, however, the defects are purely of a cosmetic nature, and not considered as abnormalities except by the critical eye of the patient. This is true particularly with lobular and supra-alar deficiencies, as well as a slight lack of contour about the anterior line.
In some instances the defect may be an acquired one, as in the lateral deviation known as handkerchief bend.
A specific and somewhat elaborate classification has been given to the more important and distinctive deformities of the nose, principally to facilitate the proper citation and recording of cases.
It may be readily understood that each one of these classifications may be further subdivided, but such subdivision can be only of the degree or extent of the deformity, and must be left to the individual operator and his thoroughness of observation and nicety of recording.
The author prefers making a plaster cast of the entire nose which is to be corrected, and a second cast after the operation has been completed, or at the time of his discharge. A record sheet, or a direct photograph, can be made before and after operation for the same purpose, which is not so desirable, however, because it has been found quite impossible to procure the desired accurate pictures of a nasal deformity, the photographer not being given to bringing out imperfections as the surgeon wishes them, even under the most explicit instructions, unless the surgeon accompanies the patient to the studio to supervise the posing. This requires a waste of valuable time; not to speak of the expense of making pictures of a pathological nature. The better way would be to have an apparatus in the operating room. The surgeon can then pose his patient against a screen background in the position and to the size of picture he may[288] desire. Plate cameras and time exposures are best for this purpose. For recording and half-tone reproduction silver prints are found best.
For all deformities of the anterior nasal line a hydrocarbon compound of the higher melting points should be used. This should be injected in the cold form. The mixture given on page 39, with perhaps an added half dram or dram of paraffin, has been found excellent, the addition of paraffin being made to assure a suitable fineness of contour and width. The softer mixtures are more liable to cause a lack of contour and a consequent widening of the part injected, even after molding, because of the contractility of the skin overlying the injected mass, which tends to flatten it out, giving the nose a less artistic and delicate appearance.
Furthermore, a soft mixture will be found to be inefficient in overcoming the tension of the skin in most cases, especially those about the middle third of the nose.
In some cases of lateral deformity, and where otherwise mentioned, it is advisable to use only a mixture of the lower melting points, as in the case in the correction of interciliary furrows and temporal muscular deficiency.
Superior Third Deficiency.—The degree of depression about the superior third or root of the nose varies considerably. The most extensive form may be commonly found in the negro nose, where there is almost an absence of a rise in that part of the nasal bones. Such noses are also found in the Chinese and Japanese. The condition ofttimes may be associated with epicanthus.
Epicanthus, formerly corrected by an elliptical excision done anteriorly, can be entirely overcome by the subcutaneous injection method, thus not only avoiding the resultant linear cicatrix, but building up the depressed nose to its normal contour.
The skin overlying most of the defects of the superior third is usually found to be loose, hence injection is readily accomplished.
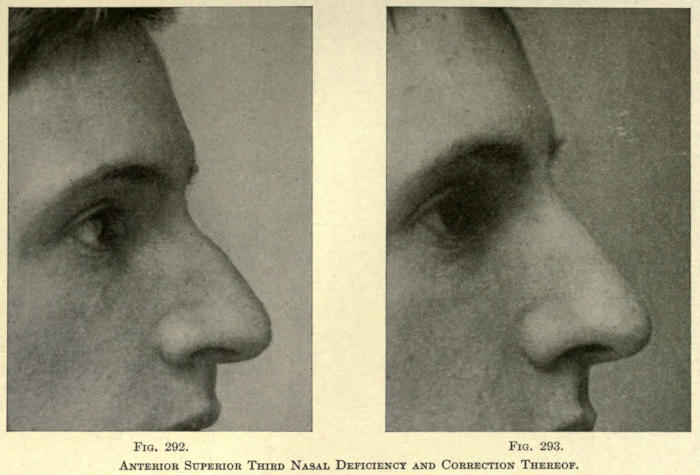
Fig. 292. Fig. 293.
Anterior Superior Third Nasal Deficiency and Correction Thereof.
The needle should be introduced laterally and anterior to the angular vessels to prevent their occlusion and injection. The point of selection is made at about the middle of the deformity. The needle is introduced until its point lies in the center of the depression, or at the median line from the anterior view.
The mass is injected slowly as the skin of the nose is pinched up between the forefinger and thumb of an assistant.
The part is injected until a tumefaction, equal in body to the extent of the deformity, is attained.
The needle is allowed to remain in place for a moment, to permit of a stoppage of the threadlike mass, usually following the pressure applied to the piston, after the operator has stopped turning the screw. This will prevent the mass from following into the channel made by the needle, or the backing up of the mass, as it were. Should this occur the paraffin mixture should be squeezed from the skin opening to prevent the formation of an intercutaneous encystment.
Immediately the needle is withdrawn the operator places a finger tip over the opening and proceeds with the thumb and forefinger of the right hand to mold the mass into the desired shape.
The post-operative treatment should be as previously given, and is the same with all injections about the nose, so that it will not be referred to again under this heading.
While a fairly large defect can be corrected at one sitting, it is advisable to rather reinject one or two weeks later to secure the exact shape.
It is to be impressed upon the operator that there is always a slight broadening of this part of the nose following the development of the connective tissue which takes the place of the injected mass, hence the injection should not be overcrowded nor the parts overcorrected.
The mass should be molded out as narrow as possible and be pinched between the fingers by the patient two[291] or three times a day after the reaction has subsided, which is usually about the third day. This procedure will keep the mass from being flattened during the time tissue replacement takes place.
Middle Third Deficiency.—This defect is commonly seen in football players and pugilists as the result of a breaking of the inferior extremities of the nasal bones and the displacement of the articulating cartilages, although the defect is often seen as a result of an injury to the nose early in life, causing a lack of development in the superior or articulating extremities of the cartilages. Nondevelopment from catarrh, syphilis, and intranasal disease are other causes. This type of deformity is generally designated as the saddle nose.
In the latter cases the skin is usually bound down to the cartilaginous structure by cicatricial bands, and needs to be liberated. This is accomplished subcutaneously with a fine tenotome introduced laterally.
To assure the operator of a thorough dissection he may inject the site with sterile water through the opening made with the knife, squeezing it out before injecting the nose.
If the skin has had to be freed by surgical means the mass injected should be sufficient to overcome the defect almost entirely, to prevent the reformation of the bands of connective tissue which have been severed. Their re-establishment would mean an unequal development of the new connective tissue springing up from the injected mass, thus defeating the object of the operation.
If no dissection has been done the defect should be corrected about two thirds and added to by a subsequent injection.
The mass in either case should be well molded out, especially at both sides, to keep the nose as narrow as possible. There will be more or less widening ultimately following the organization of the mass.
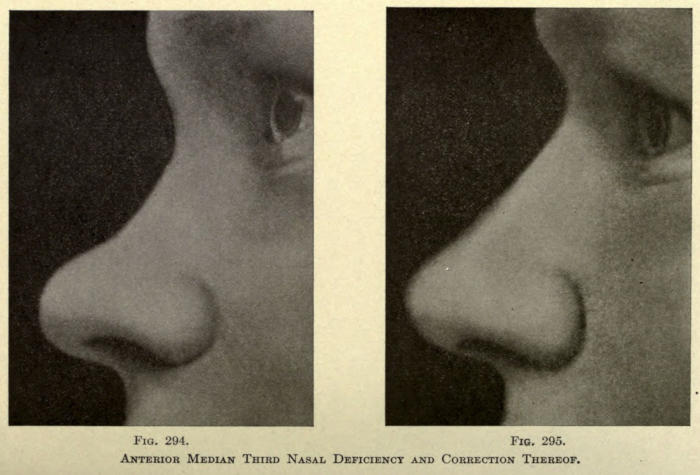
Fig. 294. Fig. 295.
Anterior Median Third Nasal Deficiency and Correction Thereof.
It is not uncommon to find a dividing wall of subcutaneous tissue about the articulation of the nasal bones and cartilages, as evidenced by a rising up or down of the injected mass above or below this line. If this be found, rather than break down this wall with the injection, it is deemed advisable to inject each chamber separately and mold the two masses after injection, as in the ordinary type of cases.
Inferior Third Deficiency.—This deformity of the nose is due purely to a lack of development or a luxation of the cartilage of the septum and the upper lateral cartilages. The point or lobule of the nose is usually tilted upward and the subseptum curved upward at its middle third.
The cause of this deformity is usually due to direct violence at some time in life, with improper replacement at the time of injury. Syphilis and intranasal catarrh, lupus and ulcerative diseases, are also causes.
The skin overlying the defect may or may not be closely adherent, but is in most cases rather thickened and inelastic. It is therefore necessary, in most cases, to loosen the skin by subcutaneous dissection, done as already described before the injection is made.
To rebuild such a nasal defect without dissection, except in such instances where the skin is quite elastic, is not to be advised, since the injected mass would be flattened, more or less, antero-posteriorly, giving the nose a broad and ugly appearance after the connective-tissue formation has been attained.
It is with cases of this kind that paraffin injections introduced in the liquid form and of high melting points are usually expelled in a week or ten days, or even later, subsequent to a breaking down of the surrounding tissues and the resultant abscess.
The best preparation to employ is the form of paraffin mixture advocated in the preceding operation used in its cold state and injected slowly, after the integument has been rendered mobile enough to permit the desirable correction.
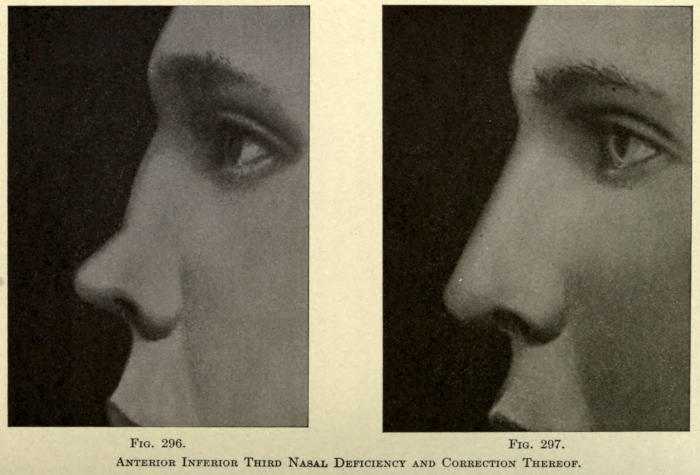
Fig. 296. Fig. 297.
Anterior Inferior Third Nasal Deficiency and Correction Thereof.
The defect should not be corrected in one sitting, for the very reason that some widening of the nose may take place, owing to the contractility of the skin, post-operatio.
The mass injected should correct the major part of the defect and be molded out carefully, especially from both sides of the nose, and the patient be instructed to pinch the nose laterally several times a day after the reactive inflammation has subsided with the object of keeping the nose as narrow as possible.
After the mass has been thoroughly replaced with connective tissue and the anterior line is found to be too depressed, a fine line of the mass about the thickness of the needle may be injected over it in a vertical direction, the point of a fairly large needle being introduced just above the anterior aspect of the lobule and thrust upward to the superior border of the now existing deformity, and be slowly withdrawn as the mass is injected.
This will leave a rounded cylindrical-like mass along the anterior nasal line, which must not be molded at all, except to soften or shade off the superior and inferior extremities.
The author advocates making two such injections, at the same sitting, when the deformity has persisted. These injections are made parallel to each other with a distance of about one eighth inch between them.
The subseptal deficiency will also have to be corrected. This will be referred to later under its separate division.
The reaction in cases of this type is usually more severe than those just mentioned. There may be considerable swelling and discoloration, but by following the methods of treatment laid down heretofore the symptoms usually subside in two or three days.
Superior Half Deficiency.—In this type of deformity there is found a nondevelopment of the bridge of the nose, while the greater part of the cartilage of the septum and the lower lateral cartilages seem to be quite normal in[296] contour. The nose has a dished appearance, with an undue prominence of the nasal base or lower half.
Various causes may be given to this condition, but heredity is responsible in a great majority of the cases.
The deformity in the type under consideration rarely takes in an accurate half of the nose, there being an involvement more or less of the lower anterior half, yet it is sufficiently distinctive to give it specific classification.
For the correction of the defect in such cases the injection is made laterally, the same mass being employed as in the preceding cases.
In this type of case the mass injected should quite correct the defect and be molded with great care to a desired contour, keeping in mind always the condition and elasticity of the skin overlying it.
An inflexible skin should be rendered mobile by digital massage, practiced for a few days prior to operation, or in tense conditions be loosened by subcutaneous dissection.
The great fault in injecting so large a quantity as is necessary in these cases is to make the nose too wide from the very beginning, which, added to the widening following the replacement by new tissue, makes the shape of the nose unsatisfactory.
For this reason it will be found of some benefit to apply an anterior nasal splint of aluminium, covered interiorly with a fold of white flannel or gauze and pressed into such shape that when applied to the nose it will keep the latter pinched up laterally to the desired width. This splint will hardly ever be borne by a patient and causes great discomfort until after the post-operative reaction has subsided. It may then be bandaged or held in place by strips of Z. O. Adhesive plaster for an hour or two in the day and during the entire night.
After the first few days’ wearing the patient soon becomes accustomed to the splint. It should be worn as mentioned for about three weeks, when the patient may[297] be permitted to pinch the nose laterally with his fingers two or three times a week or more.
The secondary injection may be made in the ordinary way or as advocated by the author in the manner described in correcting defects of the inferior third of the nose.
Inferior Half Deficiency.—In this type of deformity the greater point of nondevelopment or deficiency is found at the upper extremity of the cartilage of the septum, below its articulation with the inferior border of the nasal bones, and involving to a greater extent the area over the upper lateral cartilages.
This deformity, due to whatever cause, rarely affects the base or inferior part of the nose, owing undoubtedly to the greater protection and stability offered by the lower lateral and sesamoid cartilages and the dense cellular tissue making up the alæ. Except in such cases where violence of an extreme nature has been exerted in early life, or where ulcerative disease has broken down most of the cartilage of the septum, the point of the nose is usually normal in size and shape. In the latter cases there is an upper tilt of the lobule and a shortening of the columna upon itself with a convexity in an upward direction.
The cause of this type of deformity is usually a direct blow upon the point of the nose, syphilitic ulceration internally, catarrh, or other ulcerative disease.
When due to violence the point of the nose may or may not present a normal appearance, there may be a normal base tilted upward (retroussé or snout nose) or a dropping forward and downward (hook or beak nose).
The shape of the nasal base depends much upon the time of life the injury was received—that is, before or long after puberty, also upon the extent of injury inflicted and where applied.
From injuries received early in life we may look to a lack of development in the cartilage of the septum[298] alone, or associated with deficiency in one or both lateral cartilages.
The deformity is usually symmetrical, but where the nasal bones have been injured as well, particularly where one bone is injured more than its fellow, there is a possibility of the disfigurement being unilateral. This is rarely the case except when due to punctured wounds; generally in such cases the anterior nasal line assumes a twisted form.
Some operators have included noses of undue lobular prominence (à la Cyrano de Bergerac) under this type of deformity, and while it is to be admitted such a nose might be built up by subcutaneous prothesis the result is anything but harmonious or normal. Such a nose should be reduced by cutting operations instead of being added to. The seeming depression above the lobule is only comparative to the overdeveloped form of the lobule. The face values of every patient should be studied, and the surgeon should never attempt to break up the harmony of facial form by simplifying an operation and rendering the patient’s appearance even more ridiculous than before his attempt to correct a fault.
The correction of the deficiencies of the lower half of the nose is associated with difficulties in various directions. Either the skin over the defect is too dense to render injection an easy matter, or the nose is so broadened horizontally from the original injury that the injection, no matter how artistically done, leaves the nose bulky and ugly in appearance.
When the nasal processes of the superior maxillary bones have not been widened unduly by an injury and the skin is dense, simple subcutaneous dissection before injection will overcome the difficulty easily enough.
In that case the needle is inserted laterally in a line with the maximum depth of the depression and the point shoved up to the median line anteriorly.
Enough of the cold mixture of paraffin and vaselin, as[299] heretofore advised, is injected to reduce the deformity nearly to the normal.
The mass is molded to give the nose as near a normal contour as possible, always keeping in mind the later broadening of the nose when the new connective tissue has taken the place of the injected mass. A later injection made, as advised heretofore, will restore the anterior line to better form.
If the nasal processes of the superior maxillary bones have been thrown outward considerably a surgical operation is necessary to reduce them.
No injection should be made until the wounds from such operation are thoroughly healed and contracted.
In all cases of this type the skin will be found to be rather dense and likely to be tied down by past inflammations to the anterior aspects of the lower lateral cartilages at their juncture with the upper lateral cartilages. If the adhesions are not too dense the harder form of the cold mixture should be used. This will not only permit of raising the skin more readily than with a softer kind of mixture, but will be more likely to retain its form under the contractile pressure brought to bear down upon it.
When the skin is closely adherent it should be loosened subcutaneously, as already advised. The injection may be done at the same sitting, and be of greater quantity than in the cases where this had not been done, for the reasons mentioned.
Pressure splints and manual compression should be employed as in the preceding deformity.
The reaction following the first injection is likely to be severe. Cold applications, as previously referred to, are indicated, and should be continued for at least two days.
Care should be taken not to inject into the lateral vessels, which usually lie on a line with the juncture between the lateral and lower lateral cartilages. If this should[300] happen, the point of the nose at once assumes a bluish hue, and there is more or less pain felt at once, with considerable swelling a few hours after the injection. Later, every symptom of gangrene of the lobule is liable to be noticed, yet with faithful attention to furthering the circulation of the parts by either cold or hot applications, the active inflammatory symptoms usually subside in ten to fourteen days, leaving the patient with a whole nose, more or less colored at the lobule, according to the state of the circulation and the exposure of the parts to the various temperatures. This may be overcome in time, yet it may persist for years, depending entirely upon the ability of the anastomosing vessels to overcome the artificial thrombus or occlusion offered by the mass injected.
That a reaction quite similar in character, but of milder degree, is likely to be seen when one of these vessels has not been injected, can be readily understood when we consider that a hard and somewhat ungiving mass is made to overlie the vessels themselves. The symptoms just described in such case are apt to be noted much later, even several hours after the injection, because the swelling has then begun to add its pressure to that of the mass in obstructing the flow of blood to the lobule. Such condition may be termed pressure occlusion in contradistinction to thrombotic obstruction.
These symptoms usually subside in a day or two, or with the swelling caused by the reaction.
If the symptoms appear at once after the injection, it is best to force out as much of the injected mass as is possible through the needle hole through which it has been introduced.
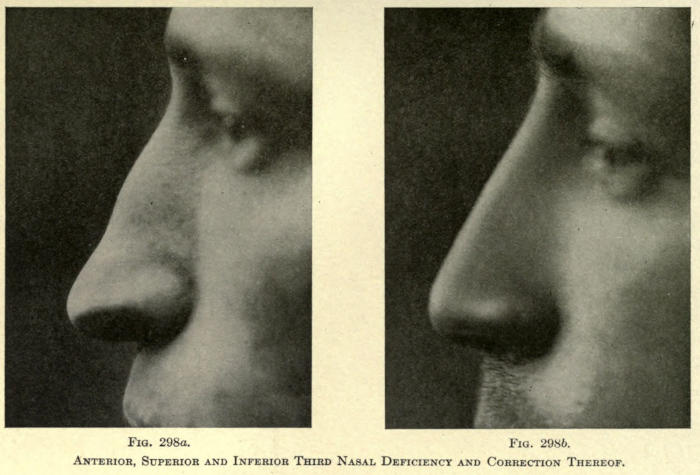
Fig. 298a. Fig. 298b.
Anterior, Superior and Inferior Third Nasal Deficiency and Correction Thereof.
The author was called to attend a case several hours after the operator had injected a nose. The acute symptoms pointed to a direct occlusion of the vessels, yet the surgeon who had performed the operation assured me he had not injected until he found that blood did not flow from the needle after its insertion. To relieve the patient of immediate fright and some pain, a dull pointed needle of larger caliber than the one used in operation was pushed through the needle wound previously made, taking the place of a cannula, and a greater part of the injected mass was squeezed out. Ice cloth applications were followed through the night and the nose recovered in three days without showing the discoloration of the skin usually observed following such cases. The nose was never injected again, on account of the dread of the patient, but peculiarly the anterior line showed almost a normal contour after four weeks had elapsed. This only goes to prove that very much less of the mass to be injected is required than is commonly supposed by operators.
Total Anterior Deficiency.—In this condition there is a scooped-out or general curved-in appearance of the entire anterior nasal line. The lobule of the nose is usually normal in size.
This defect should be corrected by two injections of the paraffin compound previously referred to. The points of injection should be lateral and anterior to the angular vessel on the side of the nose preferred by the operator—one about the center or major curvature and the other about the inferior third.
Care should be taken to mold the injected mass as narrow as possible, or as much as the skin will permit. If the latter is bound down it should be mobilized by subcutaneous dissection or levation. A subsequent injection should not be undertaken until the entire mass has become settled or fairly organized, which is about the end of three weeks.
The mass should be injected well up to the root of the nose to give it the appearance of the normal bridge. If this is found impossible owing to a dividing skin attachment, a third needle puncture should be made at a point on a level with the internal canthus.
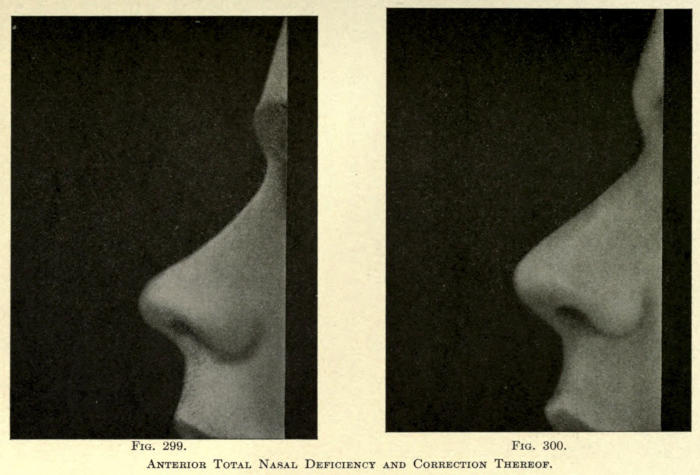
Fig. 299. Fig. 300.
Anterior Total Nasal Deficiency and Correction Thereof.
Care must be exercised to keep the mass from creeping into the loose tissue about the internal canthi by having an assistant press the sides of the nose at that point with the thumb and forefinger.
This undesirable condition is much more liable to occur when a hot liquid paraffin is employed, since the operator can observe quite accurately the extent and direction taken by the mass injected when the cold product is used.
Some authorities have injected noses of this type from the point of the nose, but it will be found that the position of the puncture at this point allows a considerable portion of the mass to work out during molding and also to permit of the readier oozing out of the mass during the pressure exerted by what reactive inflammation follows the operation. This is accounted for by the fact that the needle creates a tubelike canal in the tightly bound down tissue overlying the lower lateral cartilages, whereas in the lateral punctures the short canal is easily displaced by the swelling, thus causing its obliteration and preventing the free oozing.
On the other hand, it will be found to be more difficult to inject from the point of the nose alone and that a very long needle has to be used which must be withdrawn as the parts above the point are filled. Furthermore, it will be found necessary to thrust the point of the needle in different directions to overcome vertical attachments of the skin which are more readily lifted up than thrust aside by the mass, hence necessitating a greater amount of injury to the tissues, not to speak of the possibility of injecting transverse blood vessels higher up in the nose of which the operator would not be aware at the time; showing only in the resultant phlebitis and unexpected reactive symptoms, associated with a discoloration more or less lasting according to the extent of obliteration of the vessels.
The post-operative treatment should be as heretofore advised.
Lateral Insufficiency (Unilateral and Bilateral).—Depressions about the sides of the nose are usually due to hereditary causes, when they are likely to be bilateral, yet intranasal ulcerations may cause a falling-in, as it were, of either one or both nasal walls, involving in such instances the entire side or part of it. In the partial cases the depression may be in any of the division of thirds used by the author—that is, it may lie laterally over the region of the nasal bone and such of the nasal process of the superior maxillary bone as goes to make up that part of the nose, or in the middle third below the bone structure and above the superior limitation of the lower lateral cartilages, or within the lower third over the inferior border of the cellular tissue making up the nasal rim.
Traumatism may be found to be the cause of such depressions, especially in the middle third, after fracture or luxation of the nose. In such cases the defect is usually unilateral or at the seat of the former injury, a convexity usually being exhibited on the opposite side.
Since the skin is rather firmly adherent at the sides of the nose, except in the major part of the superior third, it will be found best to raise the skin of such defect into normal contour by a series of very small injections instead of following the method heretofore advised in connection with tense or adherent areas of skin, for the reason that such dissection would render the skin too mobile over an area usually beyond the defect itself and inviting the surgeon to an annoying hyperinjection which renders the part more unsightly than prior to the operation. This is true in most cases unless the depression is of traumatic origin and beyond the size of deformity usually corrected.
The author advocates the employment of a hypodermic needle attached to the syringe in place of the regular needle and that the injection be of sterile white vaselin without additions of any kind.
Such injections may be made very readily, one or more at the first sitting, being introduced below the deepest part of the defect. It is surprising how much four or five drops of such an injection will accomplish. Furthermore, it is to be remembered that the injections about the side of the nose are readily replaced by new connective tissue, equal to, if not commonly greater in amount, than the mass injected, such growth being completed in about two months after the time of injection. This may be explained by a more or less active perichondritis when the injection is made over the cartilage, the inflammation, thus set up, being of longer duration than where the skin and bone or areolar tissue are involved. Any subsequent injection should not be undertaken until at the end of two weeks or more for the reasons above stated.
The injected mass at all times should be introduced under normal pressure, never to the extent of rendering the skin above it white in color. The mass should also be molded out with the tip of the finger or the rounded, dull handle end of a scalpel. If necessary, the small finger may be introduced into the nostril to facilitate this molding. Should the reactive inflammation be severe such remedial agents as have been referred to should be used to reduce it.
Phlebitis following injections at the side of the nose is due entirely to the injection of a blood vessel and must be avoided. When a fine needle is used there is less likelihood of free bleeding from an injured vessel, therefore a thorough knowledge of the usual position of the vessels about the sides of the nose is absolutely essential. Bleeding of greater extent than that which would follow the thrust of the needle through the skin should put the surgeon on his guard. Experience is the better teacher and conservatism in these ofttimes delicate, subcutaneous operations will save the surgeon much annoyance and eventually the need of having the patient[307] submit to a cutting operation to reduce an overcorrected area.
Should a hyperplasia of connective tissue result from such an operation, a small linear incision, under four per cent eucain anesthesia, should be made directly over the greatest prominence, through which the offending mass can be removed by the aid of a small hooked knife or a fine pair of curved scissors.
The mass should be removed beyond the plane of the skin; in fact, it should be rather removed in conelike form, apex inward, and the peripheral attachment completely obliterated, in order to obtain the desired result, as it is not unusual to have the prominence reappear after imperfect extirpation and improper dissection.
Moist pressure dressings may be applied over the small wound thus made, for several days, or until the inflammation following the operation has subsided. Suturing such a wound is hardly necessary, but if the incision be over one fourth of an inch long, two fine silk sutures, deeply placed, may be utilized, their tension adding to the compression needed to bring the mobilized skin into position in reference to the base of the wound.
The author has used contractile collodion in place of compress dressings with very good result. This should be renewed within forty-eight hours.
After eight or ten days silk isinglass adhesive plaster is applied over the wound until it falls off.
Lobular Insufficiency.—This defect of the nose is usually of hereditary origin, although it may be occasioned by the retraction of the inferior half of the organ in tubercular or syphilitic ulceration in which the lobule falls inward and upward by the loss of the retaining cartilages.
Owing to the close adhesion of the skin to the lower lateral cartilages and the cellular tissue about the rim of the alæ it is found difficult to restore the contour or elongate the organ at that site by subcutaneous injection.
Even after thorough mobilization of the integument[308] the subsequent injected mass is liable to be thrown off by an overactive inflammatory reaction, due undoubtedly to the adhesions formed between the divided surfaces from the periphery inward which has a tendency to crowd the injected mass forward and downward before a new connective tissue has had time to be formed, causing a breaking down of the skin at some point overlying the mass and allowing it to escape.
The author has attempted to replace the injection by small solid paraffin plates introduced through a small lateral incision made for the subcutaneous dissection, and while the wound healed readily enough and the nose appeared normal, the plates were in every case thrown off by a later inflammatory process before the end of the third week.
The author then attempted to replace the solid plates with granular paraffin, gently packing the latter into the wound until the desired elevation had been obtained with the idea that such mass would accommodate itself much better under the pressure caused by reactive inflammation, but even this procedure proved unsuccessful.
The best results are obtained with sterilized white vaselin injections when there is considerable mobility of the skin. A single needle opening should be made, preferably about the center of the side of the lobule, or slightly anterior to this point, carrying the point of the needle forward to the anterior median line and a little above the actual point of the nose.
The injection should be made slowly, closely watching the size of the elevation caused by the mass and the state of the circulation about the entire lobule.
Usually ten drops of the mass suffice to give the desired result. The mass may be molded out if found desirable, but if the skin appears normal after the operation and the tumefaction thus made does not make the nose look grotesque, it may be allowed to remain as injected, depending upon the subsequent reactive pressure[309] to force it into shape. In this way a greater part of the mass is retained at the wanted site and is not crowded to the sides of the lobule by the customary post-operative molding.
Even with this method great care must be exercised in not injecting too much at each sitting. A failure is sure to result in hyperinjection about the lobule. When it be remembered that only a very small quantity of the mass will make a decided difference, the surgeon and patient should be satisfied with the slightest gain.
If, however, the mass be retained and further elongation of the lobule is desired, a subsequent injection can be undertaken, but not until a full month after the primary operation.
Here, as with lateral nasal injections, there seems to be an overproduction of new connective tissue following such an injection; a decided factor in eventually pleasing the patient.
It is needless to say that the operator must avoid injecting one of the blood vessels of the lobule, as this will cause considerable inflammation from which the lobule does not recover readily, owing to the dense tissue the surgeon has to deal with, leaving the tip of the nose discolored and bluish for some time after the operation.
If the injected mass causes an immediate venous stasis of the lobule, hot applications should be applied at once, or as soon as the operator discovers that the proper massage and pressure to remove the offending mass does not improve the circulation.
The author advocates the judicious use of antiphlogistin, faithfully applied hot every six hours and continued until the acute inflammatory symptoms subside, when the surgeon may resort to ice cloths or cold pack until the danger of pressure and resultant gangrene have subsided.
Despite the very grave symptoms associated with such inflammation, the operator may assure the patient against[310] permanent disfigurement, although the three or four weeks’ duration of treatment, usually required in such cases, is an ordeal the cosmetic surgeon and the patient are not liable to forget.
If the injected mass causing this state of affairs has been of liquid paraffin, the better method to pursue is to make several small incisions into the site of the injections and remove the little masses of solid paraffin as far as possible with the view of relieving the pressure or encroachment, at the same time alleviating the pain and stasis by the resultant depletion. Moist, hot applications should follow this procedure. The small wounds made in the skin will heal without suture, leaving hardly any perceptible scar.
The author, however, advises against any mixture or liquid paraffin injections about the lobule, never having seen a satisfactory result when either had been employed.
The post-operative treatment in uncomplicated cases may be of aristol and adhesive isinglass plaster or collodion.
Interlobular Deficiency.—This condition is hereditary in the great majority of cases. The defect, while quite disfiguring, giving the appearance of a cleft nasal point, is easily corrected by the subcutaneous injection method.
Paraffins of high melting points should, however, never be employed for this purpose for diverse reasons: first, the hardening of the mass after cooling causes too much pressure upon the small blood vessels at the point of the nose and results in more or less permanent discoloration of the tip; second, by reason of the pressure of a hard mass, at the end of the nose, considerable inflammation results which usually terminates in the evacuation of the entire mass and consequent cicatrization; third, by virtue of the greater irritating qualities of paraffin a greater amount of new connective tissue than necessary is thrown out, causing a general and hyperplastic rounding of the entire tip of the nose that requires[311] surgical interference to overcome. In the illustration shown the patient’s nose was injected along the entire anterior line and the lobule with paraffin liquefied under heat. A marked post-operative inflammation resulted, with permanent redness of the entire organ and several decisive capillaries showing about the sides and tip of the nose. This was followed in about six weeks by a progressive hyperplasia which left the nose about three times its natural size, and the lobule a hard, ball-like knob of high red color. Several cosmetic operations were required to make the nose appear anywhere near normal, while the electrolytic needling process was resorted to for a number of sittings to destroy the acute redness and the individual vessels showing.
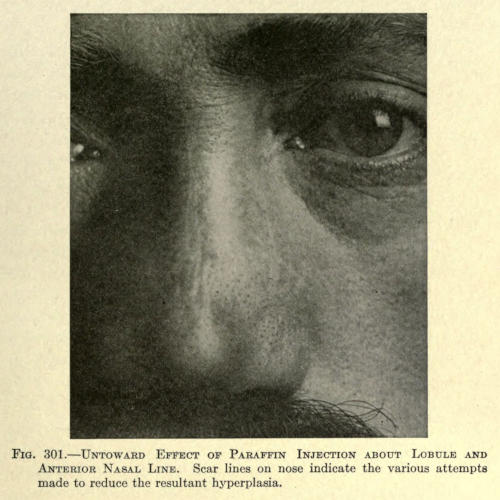
Fig. 301.—Untoward Effect of Paraffin Injection about Lobule and Anterior Nasal Line. Scar lines on nose indicate the various attempts made to reduce the resultant hyperplasia.
While a great many workers with paraffin deny any beneficial results from the employment of sterile white vaselin for subcutaneous injections, the author claims that in this particular class of deformity it is almost exclusively required.
The vaselin in cold state should be injected directly under the skin overlying the deepest point of the cleft and be slowly continued until the lobule assumes its normal contour. The puncture may be made below the point of the nose.
One such injection usually suffices to correct the fault. The reactive symptoms are not severe if proper technic has been applied, and cold compresses usually relieve it within twenty-four hours.
Should the skin be adherent about the anterior aspect of the lower lateral cartilages, it can be forced away with a small, dull, round-pointed knife resembling an eye spud, the opening for which need not necessarily be greater than that made for the needle. The latter is inserted through the same opening, which must be closed over in this event with a drop of contractile collodion into which aristol is introduced with the pulverflator, which not only embodies an antiseptic, but at the same time hastens its hardening.
Alar Deficiency (Unilateral and Bilateral).—The contraction about the nasal rims may be due to hereditary causes or the result of intranasal disease. The defect is usually bilateral, involving the entire alæ or only their lower half or third.
The fault should be corrected by several injections made along the rim of the nasal wing, using a fine needle, preferably of the hypodermic size. Vaselin only should be used and two or three drops, according to the extent of the deformity, be injected into the cellular tissue at the point of each needle insertion.
Three of such punctures may be made along the rim, one beyond the other in each wing. According to the[313] defect the injection may be carried higher or lower above the margin of the rim by shoving the needle upward and toward the inferior border of the lower lateral cartilage.
The reaction in these cases is very little, rarely necessitating other than an antiseptic powder-plaster dressing. Subsequent injections should be made if the first do not give the desired contour; but never until the surgeon is satisfied that the resultant new connective tissue thrown out has reached its ultimate growth.
The harder paraffins, especially those injected in the liquefied state, are not to be tolerated for the reasons given with the preceding method of correction.
Subseptal Deficiency (Partial and Complete).—It is not uncommon to find a marked concavity of the subseptum in noses that have sunken in by reason of intranasal disease or traumatism.
This concavity, when partial, is usually most marked near the lobule, but in the complete variety the upward curve may be greatest near its juncture with the lip.
Owing to the usual adhesions formed during the inflammatory period causing the deformity the correction of this defect is quite difficult. As a rule, the skin of the entire subseptum needs to be dissected away from the underlying structure before it will permit of correction by the injection method.
This dissection is advocated and can be readily done from one of the nostrils at a point just beyond the union of skin and mucous membrane.
The dissection under such method can be made more thoroughly than when done exteriorly, for the reason that the entire field is laid open to a free use of the scalpel, leaving no visible cicatrix externally. The dissection may be followed by the immediate injection of the mixture of paraffin and vaselin, as already referred to, used cold, or the area is injected with normal salt solution until the intranasal wound has healed, which usually takes place in about five days. The mucous membrane[314] in such instance may be neatly but not too tightly sutured with No. 1 silk. If the operator deems it advisable he may inject the salt solution again on the third day to prevent the formation of such adhesions as may interfere with the ultimate hydrocarbon injection. This is rarely found necessary.
If the post-operative inflammation prove mild, then the adhesions will not be as tenacious, in which case the surgeon may wait until even the seventh or eighth day before injecting the paraffin compound, to be sure of not forcing the intranasal wound apart under the pressure of the mass injected.
Never should so large a quantity of the mass be injected as to cause blanching of the narrow strip of skin. This is sure to result in gangrene of some, if not all, of the skin of the subseptum—a result much to be regretted, since subsequent correction of the deformity increased by the contraction of the dermal cicatrix is rendered well-nigh impossible by reason of this very tissue.
Hard paraffin injected in its molten state is never borne in this part of the human economy. It is usually thrown off after a few days of very painful and highly inflammatory symptoms, undoubtedly explained by the fact that the circulation of the subseptum is principally dependent upon the delicate branches of the two small septal arteries of the superior coronary and a hard, ungiving mass would readily cause their obliteration.
Labial Deficiency (Upper and Lower Lip).—There are a number of causes creating deficiencies about the labial orifice. The same causes apply naturally to both lips, whether the defect be unilateral, bilateral, or median. Some of these deformities are more often met with than others, as, for instance, a median deficiency of the upper lip following cicatricial contraction due to a harelip operation[315] done early in life; in elderly patients a partial paralysis is found to affect one half the upper and sometimes a part of the lower lip, giving to the mouth a drooped and grinning appearance.
Other causes are dental defects, abnormalities of the alveolar processes, traumatism, and disease.
In those conditions where loss of tissue is responsible for the defect, as in the extirpation of neoplasms, ulcerative disease, etc., it is quite likely that cheiloplasty is required to rebuild the parts, but in many of these cases splendid results may be obtained by the judicious use of hydrocarbon protheses to overcome the usual post-operative oral distortion. It is understood that such injections should not be undertaken until the wounds are thoroughly healed and the cicatricial union fully contracted. This is true also in harelip operations undertaken later in life.
The correction of labial defects coming under this method is not at all difficult, but artistic skill and judgment are as necessary as the surgical technic.
The lips are plentifully supplied with blood vessels, and therefore greater care in injecting a foreign mass into their structure is necessary; furthermore, the lips cannot be placed at rest for any long period of time, so that the mass injected can never be expected to be kept in place if of a consistency hard enough to permit the contraction of the orbicularis muscle to move it about.
From the very fact of this practically constant movement of a part it is self-evident such hard mass could not be retained or held in position for any length of time, unless the mass is small enough not to be affected by the movement, and under such condition the correction of a defect as desired by the patient would require perhaps months to accomplish, owing to the very fact that only droplike masses may be deposited under the skin in perhaps a half dozen places with the necessity of a long period of rest until the injections have been replaced by[316] the new tissue before the next operation could be undertaken.
It is absolutely absurd to think of injecting a lip with hard paraffin liquefied by heat and expect to obtain a satisfactory result. While it is true the mass is moldable immediately after its introduction, so that a desired shape may be obtained, it does not overcome the fact, however, that the mass must harden, as it will, and that, while a part of it is broken away, as it were, from the mass proper, there is a nuclear contraction as the hardening takes place, thus overcoming partly the molded form; furthermore, the movement of the parts here tends to displace the mass. Unequal muscular contraction breaks up not only the form but also the mass itself, during all of which time it is made to act as an irritant by virtue of the movement of the uneven edges of the paraffin upon the adjacent tissue.
Furthermore, the presence of paraffin and the resultant mass of new and hard connective tissue, so well recognized by all experienced surgeons, is not desirable in the lip structure; it makes the lip appear bulky and hard and anything but natural.
It is in these very cases that the injections of cold sterile white vaselin is indicated. After injection the mass may be evenly and satisfactorily molded out, the mass being soft and readily pressed into shape in the various cells of areolar tissue without leaving hard and uneven lumps.
The movement of the lip is not then a source of danger in displacing the mass, since the acute swelling of the lip tissue prevents its free movement for several days, which gives the injected mass an opportunity to establish itself and find its proper place.
Another advantage in using this preparation subcutaneously is that it is less irritating than hard paraffin, permits freer movement, and creates a better production of new connective tissue.
While a part of the mass may be absorbed during the replacement period the lip retains its normal consistency, and if the desired contour has not been attained a subsequent injection may be made in three weeks’ time without interfering in any way with the former result.
The only precaution, aside from avoiding the injection of blood vessels, is to keep the injection from the prolabium or vermilion border. The latter tissue is very prone to fatty degeneration or to yellowish discolorations when such a foreign mass has been introduced into or near its structure.
There is no objection in injecting the lip, upper or lower, in several places, as the cellular network about the mouth is sufficiently dense to prevent the escape of the vaselin injected from the adjacent opening if the distance is not less than a half inch between the punctures.
The injections may be made from above downward in the upper lip and, vice versa, in the lower. They should be begun at the outer angle working toward the median line.
The reaction following such an injection is usually more severe than in any other tissue of the face, owing to the great number of fine blood vessels, but the swelling is readily controlled in two or three days by cold applications.
Aristol collodion dressings over each wound suffice to close the punctures.
In the median variety of defect, where a cicatricial band separates the lip into halves, it may be found necessary to do a subcutaneous dissection before a suitable injection can be done, but in cases of long standing the dividing wall is exceedingly thin and the threadlike adhesions below are quite easily broken up by the force of the injection. The later product of new connective tissue will tend to further improve the contour.
Nasolabial Furrows (Unilateral and Bilateral).—This condition in the bilateral form is exceedingly common in[318] adults beyond middle age. It is also found in those individuals suffering from inanition, due to whatever cause. The unilateral form is found principally in patients suffering from semifacial paralysis in which the tissue lacking the proper neurotic supply droops or sags down, causing a deep furrow to appear from the attachment of the alæ to the angle of the mouth, associated more or less by a flattening of the cheek contour of that side of the face.
The method of correction advocated by the author varies entirely from the technic advanced by other surgeons.
The usual method has been to introduce the needle of the syringe at the outer or lower extremity of the furrow and from one of such punctures to inject the whole line of depression.
While this seems right theoretically the method does not give the desired result. Owing to the free movement of the upper lip the mass, at first neatly restoring the contour, is crowded upward into the inferior malar region and very often downward toward the angle of the mouth, where it settles in a hard lump which is not only obnoxious to the sight but interferes with the proper use of the parts concerned in mastication and vocalization. Invariably the operator is called upon to remove the disfigurement.
It can be readily understood that hard paraffin itself, in such case, would prove more objectionable than a softer mass which, upon early discovery, could be molded or massaged into better position, while nothing less than excision would prove efficacious with paraffin.
As with the lip, then, the author advocates the use of either the cold mixture of paraffin, as heretofore described, or the cold white vaselin according to the operator’s opinion in overcoming the extent of the fault. For all ordinary cases white vaselin alone is necessary.
The technic of injection as used by the author is as follows: In the ordinary case when the furrow is not too pronounced one sitting only is required. Two needle punctures are made above the upper line of the defect, the first being made about one half inch from the wing of the nose and the other about one inch outward and downward.
The needle is pushed downward under the skin until its opening corresponds to the median line or deepest part of the furrow. Enough cold white vaselin is injected to bring the depressed area slightly above the plane of the skin of the upper lip. The second puncture is made perpendicular to the first and the injection made in the same manner.
With the tip of the indicis over the first needle opening the mass is molded out evenly by a gentle rocking or rubbing movement. The same is done with the second mass.
It will be found, then, that the two masses are made to meet at about the center of the furrow, leaving a slight wall of tissue between them. This wall has the virtue of preventing the falling down of the upper mass, at the same time dividing the quantity of the injected mass into two, and lessening the weight.
If the condition is bilateral both sides are operated on at the same sitting. If subsequent injections are needed they are done three weeks later, the punctures being made between the former first and second punctures and the second and outer border of the furrow. In this way the entire site is filled with a series of injections.
If the surgeon desires he may increase the number of these needle punctures at the first sitting, making them nearer together in that event.
It will be found necessary in some cases to inject the cold mixture of vaselin and paraffin into the furrow directly below the wing of the nose, since the integument[320] at that point requires a mass somewhat harder than vaselin to force and hold it up.
The rest of the furrow must, however, be injected with vaselin alone, for the reasons already given in parts that are movable.
The reaction is rarely very marked and subsides in about three days.
Gentle massage may be permitted above the site of injection to keep the mass from crawling into the cheek. This is done by gently stroking the skin from below upward toward the nose on a line an inch above the original depression.
The dressings are the same as before mentioned, although collodion painted over the needle openings is most serviceable after having sponged off the sites with absorbent cotton dipped into absolute alcohol to remove the vaselin that may have exuded from the openings during the molding-out process.
Oral-Angular Furrow.—These furrows occur at the corners of the mouth, running downward upon the anterior chin. Small as these defects appear, they are found difficult of obliteration, for the reason that the tissues are more or less under constant movement during the waking hours. Repeated injections, each of small quantity, are necessary. Hard paraffin is contra-indicated.
The injections are made from above the defect downward at right angles to the defect.
It will be found difficult to keep the mass from being expelled on account of the movement, there being more or less oozing from the puncture, but if the openings can be controlled for at least twenty-four hours this danger may be overcome to a great extent.
Ethyl chlorid may be sprayed over the part immediately the needle is withdrawn to set the mass and followed with a drop of collodion. The patient is advised to keep the mouth as immovable as possible for the rest of the day.
The reaction is never severe, and is easily controlled by cold applications. If, after one week, there is shown a tendency to sagging of the mass, it should be gently massaged upward with the finger several times during the day for at least two weeks; this will keep it in place, and allow nature to replace it with new connective tissue when desired.
Deficiency of Cheek (Total and Partial).—A total lack of proper contour of the cheek, generally termed flattening, may be due to hereditary causes, but is generally dependent upon a cachexia due to a general disease, or fatty degeneration of the muscular structure of the cheeks, as found in those beyond middle age.
A partial deficiency of the cheek or cheeks is usually hereditary, but may be dependent upon digestive disorders or other causes of malnutrition.
This class of deformity is found more often in women than men. It is usually bilateral.
Unilateral cheek deficiency, whether partial or total, may be congenital, but is often the result of a local paralysis causing hemiatrophy. Traumatisms early in life or during birth and amputation of the inferior maxillary are other causes.
This class of deformity is quite readily corrected by subcutaneous injection; in fact, it is the only known method of merit, superseding the former resort to partial correction by massage or artificial and temporary correction by the wearing of plumpers in the buccal cavity.
The method of procedure is the same in all cases, the number of injections and quantity varying, of course, with the extent of the defect.
As with the rebuilding of the contour of the lips so with the cheeks, which must of necessity be mobile and flexible, the injection of hard paraffin is out of the question. The author has observed a number of such cases,[322] and is free to say that in each case the result was not only abnormal in appearance, but a source of great annoyance to the patient.
What is worse is that the paraffin once injected can never be removed except in places where an actual encystment has taken place, in which case the hard mass may be removed through a small incision made directly over the mass and introducing a grooved director into the opening then by the rotation, or to-and-fro movement of which, combined with digital pressure, the cyst is evacuated. Once the mass is replaced by a network of connective tissue it could not be removed except by an extensive dissection and extirpation, which leaves behind it cicatrices far worse than the appearance of the parts before operation.
The author injects cold sterile white vaselin below the skin here and there about the cheek at the sites of deepest deficiency.
These injections may be made under ethyl-chlorid anesthesia.
Each injection is carried to the extent of causing a lump below the skin, the quantity being judged from a thorough experience with similar cases.
After the injections have all been done, the thumb of the right hand is passed into the mouth against the buccal mucous membrane of the left cheek and the index finger over it externally or on the skin surface. For the right cheek the index finger instead of the thumb is placed in the mouth. The mass or lumps are now gently pressed into the desired shape and thickness by the aid of these two fingers. A few drops of the mass may be forced out of the needle holes under this procedure, but this is of no consequence when it is considered that from one to two ounces may have been injected into each cheek.
This gliding form of massage should be continued until the entire cheek presents an even and rounded-out appearance.
It will be found, in the majority of cases, that the integument of the cheeks about the region of the inferior border of the zygomatic process is rather firmly adherent, and that a subsequent injection will be necessary to elevate the cheek at that point.
Injections over the malar bone are prone to cause severe reaction, leaving a puffed appearance just below the eyelids. This may be more or less permanent and is very undesirable. It should be avoided by injecting very small quantities at that site. It is always safer to add a little subsequently.
The reaction, generally, is not severe, and is readily controlled by cold applications, yet the author has experienced considerable swelling and tenderness in two cases of total cheek deficiency corrections which lasted for several weeks after the operation, giving excellent result eventually, however. Such symptoms are dependent upon circulatory interference, but resolution should take place without untoward results with judicious treatment, unless the operator has been negligent by injecting one or more blood vessels, in which case the resultant thrombosis may cause breaking down of the subcutaneous tissue, abscess, evacuation of the mass, and possibly death in part of the integument. The precautions referred to in avoiding any such possibility have been fully given heretofore.
Never should the operator hyperinject the cheeks, even if the patient insists upon looking like a puffed ball. He should be satisfied with a normal contour, and truthfully assure the patient such hyperinjected contour could not be retained owing to the weight and dropping down of the mass before nature could properly replace it by organized tissue.
Subsequent injections may be made about three weeks after the first sitting.
With nervous and hypercritical patients the surgeon may elect to give the patient a number of sittings, injecting[324] only small quantities at two or three places each time. This in the majority of cases will give better results than when an entire cheek is injected, for the reason that the larger mass is likely to be displaced by the unconscious act of the patient in sleeping on one or both of the rebuilt cheeks or the willful massage to improve the handiwork of the surgeon in their own belief.
Massage of the cheeks after the replacement period is not to be tolerated. It tends to create hyperplasia by circulatory stimulation.
It is not unusual to have the patient tell you that for weeks after the replacement period the cheeks are swollen considerably in the morning upon arising, going down gradually during the day.
This is due to the spongy or loose character of the new tissue caused to be formed by the foreign mass, which gradually takes on a harder and more compact form.
The post-operative dressing will be either adhesive isinglass plaster or collodion. With the former, moist applications during the stage of reaction are not permissible.
Deficiency of Lid Contour (Upper and Lower Lids—Unilateral and Bilateral).—The lack of contour in the eyelids is not as frequently met with as redundancy of their integumentary structure; there are cases, however, where the eyes seem to lie deep in their sockets, owing to a sinking in or a collapse of the surrounding lids.
This condition is often found to be hereditary, in other cases it is the result of malnutrition, a peculiar lack of adipose tissue about the orbit for no known reason, or fatty degeneration in past middle life.
The fault is usually bilateral. In rare instances trauma about the orbital borders may result in lack of nutrition. Such cases are usually unilateral, and the upper lid is affected in the majority of cases.
The correction of these defects is found to be rather difficult, owing to the thickness of the tissue under consideration.
The use of hard paraffin plays havoc with eyelid tissue, rendering it hard, immobile, and causing a hyperplasia of the new connective tissue formed thereby, as well as the peculiar yellowish pigmentary spots of irregular form resembling on casual inspection xanthalasma. This discoloration has been fully described earlier in the work.
The author has had occasion to remove these hard irregular masses investing the lower lid in several cases where paraffin had been injected, also two cases in which the pigmentary discoloration involved both upper and lower lids associated with the same hard fibrous masses. Excision under local anesthesia and silk suture was the method of correction employed.
From an experience of twenty-two cases the author believes these conditions most amenable for correction by the injection of sterile oils in preference to any other substance. Even white vaselin does not here seem to answer the purpose, owing to its stimulating property of causing the resultant growth of connective tissue.
While vaselin injected in the lids causes less of this new tissue to be formed, such tissue is never of the consistency required. This is especially true of the upper lids.
The oil injected, sterilized sperm oil being employed by the writer, is prone to absorption of more or less degree, but the result is gratifying, and lasts from six months to one year, leaving no untoward effect.
If the absorption has been sufficient to leave the parts as before the operation, a subsequent injection of the same character may be undertaken six months from the time of the first or even later, as the patient may choose.
The tissue of the eyelid is prone to swell immediately the oil is injected, and this swelling is entirely out of[326] proportion to the quantity introduced. This edema, due to a retardation by pressure of the blood supply, is very misleading, the operator believing the parts overinjected. A screw-drop syringe is therefore absolutely required.
A fine hypodermic needle is used, and after a few drops of the foreign matter have been injected, the lid should be massaged gently with the tip of the indicis, employing the circular movement.
The injection should be made at the outer end of the lid about one fourth inch above or below the canthus for upper or lower lid respectively.
The needle, slightly dulled, should be long enough to reach the full length of the part to be injected. Its course can be readily seen under the thin, overlying skin.
As the injection progresses slowly and evenly the needle is withdrawn.
A second puncture or injection should not be made at one sitting; if the parts are underinjected the operation is repeated as soon as the swelling of the lid has subsided, which is about the end of the fourth or fifth day.
The reaction, apart from the edema, is very little, although there may be more or less discoloration of the parts, as the result of the obstruction offered the blood vessels.
This is always an alarming symptom to the patient, but passes away completely in the usual manner in several days.
The post-operative dressings may be collodion or silk protective.
Cold or hot applications, as may be best borne by the patient, can be used; they tend to reduce the puffing and lessen the ecchymosis. The patient should be instructed to lie with the head higher than usual for the first two nights to retard the edema.
Furrow about Canthus (Unilateral and Bilateral).—This condition is commonly called “Crow’s Feet,” and is, in the majority of cases, due to advancing age, but is acquired[327] by habitually contracting the eyelids, as in laughing or grimacing. It is particularly noticeable in persons employed in the drama.
The defect is usually bilateral, but may exist at one side only in rare cases.
The correction is easily accomplished by this method of subcutaneous injection, although a reduction of the furrow alone does not suffice, leaving a lump or elevation at the site. The author shades off the injection, as it were, making the site somewhat conelike, the apex being at the canthus and the base outward toward the hair line of the temporal region.
Sterile oil should be injected near the canthus, where the overlying integument is delicate. One such injection, covering an area of the diameter of half to three fourths of an inch, should be made, and thus backed up or built outward with two or three injections of the white vaselin, as described under temporal muscular deficiency.
The hypodermic needle should be used near the canthus, and the regular one over or about the temple.
The reaction near the canthus is similar to that with lid injections. The same post-operative treatment as with the lids should be employed.
Deficiency of the Ocular Stump.—It frequently happens that by reason of extensive inflammatory disease and adjacent adhesions of the eye, a greater part of the globe must be excised than in the usual case, whether the operation be an ordinary excision, the Mules’s evisceration or the Frost modification of the latter.
In such event the granular button or the stump made of Tenon’s capsule is too small to permit of the placing and retention of the artificial eye. In other instances the stump is so contracted that while the artificial eye is retained it must of necessity be allowed to rest deep in the socket, destroying the entire contour of the orbit. Again in the enucleation operation so little of Tenon’s capsule engages the artificial eye that movement is entirely[328] destroyed, particularly when the Mules’s glass globe has not been introduced.
Excellent results may be obtained in some of these cases, others are not amenable to the injection method because of a lack of sufficient stump to inject, and the danger of injecting through the posterior wall of the capsule, the mass in part escaping into the orbital apex, where it is liable to impinge sufficiently upon the remains of the optic nerve to cause sympathetic inflammation of the normal eye. A condition at once not easily corrected, proving dangerous to the sight of the healthy eye, and possibly producing a fatal termination.
It is with the use of paraffin, liquefied by heat and injected in this state, that such fatal cases as have been placed on record have been operated. The liquid mass under pressure forced into a soft pultaceous mass cannot be easily controlled, if at all, and accidents here are of more serious import than in any other part of the human anatomy, apart from the direct injection of a facial artery of sufficient size to produce an alarming embolism and death.
The author cannot speak too forcibly against such irrational procedure. Other surgeons are beginning to realize the danger of the use of hard paraffin injections near the eye.
The proper and safe method of improving the stump is to introduce into it, under local eucain or cocain anesthesia, small masses of the mixture of vaselin and paraffin in cold state. These injections into the stump and mucous membrane should be done several weeks apart, always keeping a respectful distance from the remains of the optic nerve.
The injections should be begun as near to the surface as possible without breaking down the tissue by necrosis, keeping in mind that one or two of such successfully introduced masses will do much toward supporting the artificial eye.
If necessary the mucous membrane back of the palpebral rim can be injected in like manner to give firmer hold to the eye and at the same time give support to the usually depressed and atrophied lids.
Wet dressings are applied to allay the reactive inflammation, which should be proportionate in severity to the amount of the mass injected.
In three cases operated upon by the author excellent results were attained, and no untoward results had been experienced two years after injection.
Anterior and Lateral Deficiencies.—An anterior lack of contour of the chin is generally regarded as of the receding type. With this is usually found a bilateral lack of form, especially in men. With a generally well-formed face such a chin gives it a weak and ofttimes a degenerate appearance. In women a deficient chin is not as noticeable, because of the smallness of the face in general and the predomination of the oval type.
The lack of prominence about the chin may be anterior only, the broadness being sufficient, due to a lack of development of the mental process, or it may be deficient laterally with a pronounced mental prominence, giving it a sharp, protruding, or pointed appearance, or the lack of form is combined, as is commonly the case.
Such chins may be made to appear normal, and even ideal, by the subcutaneous injection method. The type of chin most favored by American men is the square angular, now so plentifully seen in pen-and-ink illustrations.
The tissue of the chin lends itself readily to the building-up process. Almost any form may be attained by the judicious employment of the method under consideration.
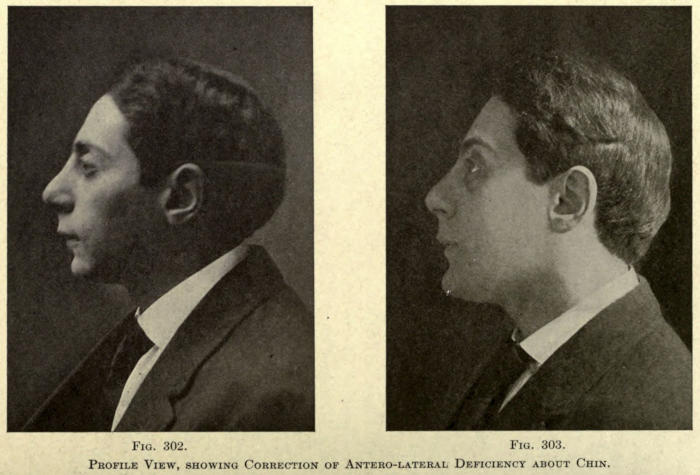
Fig. 302. Fig. 303.
Profile View, showing Correction of Antero-lateral Deficiency about Chin.
While it is true excellent results may be obtained with hard paraffin, used in liquefied form, it can often be shown, however, that the paraffin injected under pressure will run down in narrow, pencil-like streams underneath the chin and skin of the anterior aspect of the neck, where they may be felt afterward as hard oval cysts or of elongated form. This is not possible when the cold mixture of vaselin and paraffin is used, since the position of the mass can be easily followed with the eye or felt with the fingers.
The injections should be made from either angle at the first sitting. Enough of the mass should be introduced to leave a ridgelike formation across the anterior chin, varying in thickness according to the shape of the chin previous to operation and the form desired.
It is not well in chins of very deficient type to attempt to make the anterior contour as it should be in the first sitting. Too much pressure would be required, and unless the skin was freely movable considerable reactive inflammation would result, with possible necrosis of the skin in part and consequent expulsion of the injected mass.
The anterior line of such chins should be rebuilt in several sittings, always waiting for the parts to become normal in appearance and sensitiveness.
This method helps to stretch the skin, allowing of further injections and the introductions of a greater quantity than could be introduced at one time only.
The author advocates making two or three sittings of the anterior restoration of contour and two for each angle.
The angles of the chin are injected at a point about midway between the mental process and beginning of external oblique line. The mass is injected as near the inferior ridge as possible, and somewhat above the attachment of the platysma myoides muscle.
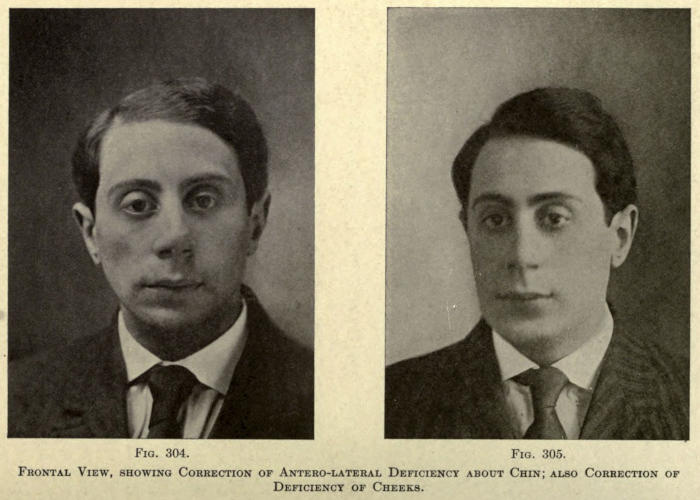
Fig. 304. Fig. 305.
Frontal View, showing Correction of Antero-lateral Deficiency about Chin; also Correction of Deficiency of Cheeks.
Only one needle insertion is made at each angle, and the mass is injected until a round elevated tumor is attained, which is pinched or squeezed with the fingers into the desired angular form, one finger being placed over the needle opening to avoid squeezing the mass out.
It can be readily seen that with this puttylike mass much better results than with the comparatively soft vaselin could be obtained while with the liquefied paraffin the operator would be at a loss to know just what had been accomplished until the mass had become fairly solidified, and then often finding the semisolid mass, which required rapid molding to give the desired shape before it would become hard and unmanageable, in a different position and much more distributed than he had expected.
For the latter reason repeated small injections have been advised, but the author believes oft-repeated injections of paraffin in a small area are prone to set up considerable disturbance, and that the resultant tissue replacement is interfered with. Furthermore, the injected mass would eventually be in grape-bunch like form, and in that condition not as manageable or inducive to the establishment of contour angulation, such as is required in the chin. The final appearance of chins thus rebuilt is heavy and rounded, lacking the concavity above the inferior prominence along the anterior line as well as the angulation laterally.
With the cold mixture advised a considerable mass may be injected at one sitting, which is easily molded into form and which retains that form unless the reactive inflammation is severe. This should not follow unless actual hyperinjection has been done or an unclean product has set up an infective cellulitis.
When the chin is uncommonly peaked, or small, it may be found necessary to inject both sides of the chin beyond the angle and in an upward direction slightly below and following the external oblique line.
Such deficiency may be found decidedly unilateral as a result of lack of development of one half of the lower[334] maxillary bone, a resection of either maxilla for whatever cause, imperfect union following fracture or disease of the bone early in life.
In such cases the lateral deficiency must be first restored, using the same method, before the chin proper can be built up. Ofttimes the lower cheek of the affected side must also be injected. This should be done after the site overlying the former body of the maxilla of the affected side has been rebuilt. The cheek should then be built out above this hard linear mass by the injection of cold white vaselin, as heretofore referred to.
The following illustrations show a chin deficient anteriorly and laterally before and the result after correction.
The post-operative treatment should be collodion dressing, followed by cold antiseptic applications for at least two days. The latter ameliorates the inflammation and helps to retain the molded shape of the mass. Subsequent sittings may be made one a week or ten days apart.
Pro-auricular Deficiency (Unilateral and Bilateral).—A deep furrow in front of the ear may be found unilateral in hemiatrophy of the face, but the condition is usually a bilateral one, due to malnutrition or the fatty degeneration of past middle age. In the latter case the depression is accompanied by a redundancy and wrinkling of the skin.
Owing to the close proximity of the large temporal vessels a hard mass should never be injected subcutaneously for the relief of this condition. Even the mixture of vaselin and paraffin has caused considerable reaction when injected to overlie these vessels.
The author advises the injection of white sterile vaselin or sperm oil for this form of correction. It should be carefully injected, since the vessels lie close to the[335] skin with the anterior auricular crossing transversely about the center of the furrow.
Every precaution should be taken, one injection only being made from below upward at each sitting if more than one is necessary, and then only after the needle has been unscrewed from the syringe to make sure vessel bleeding does not follow the puncture.
The reaction is usually severe, with considerable edema and ecchymosis.
The resultant tissue formation likewise is active, and hyperplasia at this site is not uncommon, especially if the mixture or hard paraffin has been employed.
A cellulitis following such an injection is exceedingly troublesome, the injected mass being thrown off usually at the base of the furrow, which is followed by a low type of inflammation with a protracted oozing of serous exudate. Should such a case come under the care of the surgeon, thorough cleansing of the affected site under scrupulous antisepsis should be done at once, and wet antiseptic dressings be applied daily until the wound is entirely healed.
A plastic skin operation must be done in most of these cases to overcome the ragged cicatrix formed upon healing of the wound. This should never be undertaken until the wound has been healed for several weeks at least.
After the injection of the parts cold antiseptic dressings should be applied at once, and kept up until every sign of reactive inflammation has subsided. At no time should the subsequent injection be undertaken before a month has elapsed from the time of the former operation.
Post-auricular Deficiency.—This defect is invariably unilateral, and then the result of a mastoid operation.
The skin about the depressed site will be found to be more or less firmly adherent, necessitating subcutaneous dissection before an injection for correction can be undertaken.
In this case the cold mixture of vaselin and paraffin[336] is indicated, since the softer products will hardly suffice to elevate the tense skin. If the former surgical operation has been done some time previous to the required injection the parts may at one or two sittings be restored to a fairly normal contour, depending entirely upon the amount of ungiving scar tissue at the site. If the parts are tender and not reduced to normal, the injections should be made frequently, about ten days apart, injecting a small mass across and through the subcutaneous scar attachment at each sitting.
The reactions following such injections help to tease the scar away from the bony tissue, but should not be sufficient to cause extensive inflammation.
The same mode of post-operative treatment as has been given with pro-auricular corrections should be followed.
Deficiencies about the base of the neck and the shoulders are very commonly found in women. These defects are usually bilateral, except in rare cases. The much-desired contour is readily restored by the subcutaneous-injection method, and since the technic for one part is the same as for the whole there is no need to dilate specifically upon the treatment of each part.
The author advocates the injection of cold sterile white vaselin only, for the restoration of the contour about the neck, anterior and posterior shoulder, and the mammæ, except in the unilateral correction of a flattening of the breast following amputation for the removal of neoplasms, when the mixture of white vaselin and paraffin should be used, owing to the tenseness of the skin following the excision of a large part of the integument covering the diseased gland.
In the restoration of the contour about the neck and shoulders it is well for the surgeon to familiarize himself[337] thoroughly with the superficial veins of the parts, since the vessels here are larger, and the introduction of foreign matter into them is liable to lead to serious and even fatal results.
The injections should never be made until the operator has assured himself of the fact that a vessel has not been entered into, and then only should a small quantity of the mass—i. e., about two or three drams—be injected at one point.
The easiest mode of introducing the needle is to pinch up the skin between the fingers of one hand, introducing the needle into the fold thus raised. As the mass is injected the skin should be raised by aid of the needle, so as to allow all the immediate room possible for its reception.
The mass injected is at once molded down flat with the thumb or forefinger.
A number of such injections may be made at both sides at the one sitting. The ethyl-chlorid spray may be employed to render the parts less painful. At no time should the entire shoulders be filled at one sitting, for fear that the reaction may be severe or that for any unforeseen cause infection results which would in such instance be indeed difficult of treatment, eventually leaving the parts scarred and unsightly.
Nor should the mass be injected intracutaneously, a fault sometimes observed about the base line of the neck anteriorly and laterally where the operator has been timid in avoiding the exterior and anterior jugular veins. Such injections invariably result in abscess, or when not extensive enough to cause necrosis the skin assumes a more or less permanent red or yellow discoloration over the site so injected.
The treatment for the partial or total removal of such spots has been referred to.
In the average case of contour restoration of the shoulders about eight sittings are required, two sittings[338] being given each week, and as many injections made as is deemed necessary or advisable at each.
All the precautions of technic heretofore given should be employed. The reaction following such injections is never severe, and little or no treatment is necessary.
The needle openings are covered with aristol collodion or the isinglass adhesive plaster.
At the end of six months or more after the injected matter has been quite thoroughly replaced with new connective tissue it is often found necessary to inject small quantities here and there about the shoulders, owing to the contraction of the new tissue and its ultimate fixed disposition about the parts more than to the absorption of the mass injected.
Furthermore, a certain amount of edema or swelling follows the injection of any foreign matter under the skin which is not, in cases of this kind, so readily absorbed, giving during that period of time a more pronounced contour or fullness, which, passing away in the natural course of events, does not imply the absorption of the matter injected—a statement so often made by those not in favor of using paraffins of low melting points for subcutaneous protheses.
Such result, however extensive, as it might be in some cases for the lack of proper injection or in the case with oil injections is at all times correctable, while the hyperplastic knobs, so often following the injection of paraffins of high melting points about the shoulder, can only be removed by surgical means, which leave the parts more unsightly than before anything had been done for the patient.
Rhinoplastic operations serve to correct deformities of or restore the nose. Such operations may involve only a part of or the entire organ, hence may be termed partial or total. Furthermore, a fine distinction may be drawn between general rhinoplasty as applied to such deformities when caused by traumatism, the excision of neoplasms or destructive disease, whether such correction be partial or total, and cosmetic rhinoplasty when such corrections are made purely with the object of improving the nasal form when the deformity is either hereditary or the result of remote accident.
For some unaccountable reason the latter art has not met with the general favor the profession should grant it, yet the results obtained by such specialists as have undertaken this artistic branch of surgery have been all that could be desired, and have consequently added much to the comfort and happiness of the patient.
Without a comparatively thorough knowledge of the extent of cosmetic rhinoplasty it would be difficult to draw any conclusion as to the value of this art. If it has not met with the favor it deserves it is solely due to the fact that the art has been limited to the few, and the literature on the subject is so meager, indeed, that the surgeon has been compelled in many cases to trust to his own originality in undertaking an operation of this nature.
The limitation to rhinoplasty is due primarily to the artistic skill required to obtain results; secondly, to the risks involved by loss of tissue due to gangrene, imperfect healing or accidental interference, post-operatio; and thirdly, to scarring about the face as a result of the primary and secondary wounds; in fact, so much so that many surgeons prefer to allow a small defect to remain, to escape the risks involved in correcting them.
The author believes such fear misplaced, because with the methods of surgery of the present day and the proper knowledge of the art there need be little risk involved and the result expected should be as near perfect as human skill can make it.
True, a surgeon cannot be expected to build an entire nose from the skin or other tissue of the forehead or cheeks and make it a thing of aforethought beauty and shape, but if the result be no more than a curtain of skin to hide the hideous deformity he has done his share, and such result is the worst he might look forward to.
For the correction of nasal deformities the author will consider first such operations as involve the entire loss of the nasal organ or total rhinoplasty; thereafter partial loss of the nose, and lastly such cases involving no loss of tissue and dependent on malformation only under cosmetic rhinoplasty.
It is not here intended to lay down a law for the surgeon for the restoration of the entire or part of the nose for the reason that each case differs more or less; that in each case there is more or less tissue that may be utilized, and that there are many methods advanced for such procedure, but the author does desire to give to the operator a concise and comprehensive treatise on rhinoplasty and to illustrate the best of such operations as have been placed on record as a ready guide and for immediate reference—a matter of no small moment when this literature can be gained only by searching through innumerable[341] medical journals and short references and in all languages of the civilized world.
In the chapter on history some idea of the time in which rhinoplasty has been practiced may be obtained. It is not deemed necessary to go into further historical facts here, except, perhaps, to divide the subject into the three most important schools or countries that have given individuality to the art.
The loss of the entire nose may be due to traumatism, actual amputation, the bites of man or beast, duels, the removal of neoplasms, gangrene after freezing or disease, rhinosclerosis, syphilis, the application of caustics, tubercular disease, lupus, cancer, and rarely congenital absence of the organ. The loss may be total or partial.
The extent of loss of substance in each case differs, and it is for this reason that surgeons have been compelled to originate many methods of operation, each having for its object to correct the deformity as neatly and as near to the normal as possible.
To give correctly a classification of nasal deformities would simply mean to mention each anatomical part or division of the nose referring to the deformity involving the same. For this reason such an arrangement would be uselessly extensive, but for the proper recording of such cases the author advises a systematic method of nomenclature in which the deformity is stated, as: left, unilateral deficiency of inferior lobule; or right, median third deficiency of nasal dorsum of the parts destroyed and mentioned as such.

Fig. 306.—Deficiency of Superior and Middle Third of Nose. (Saddle Nose.)
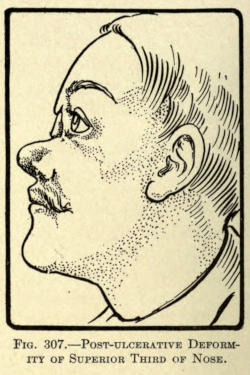
Fig. 307.—Post-ulcerative Deformity of Superior Third of Nose.
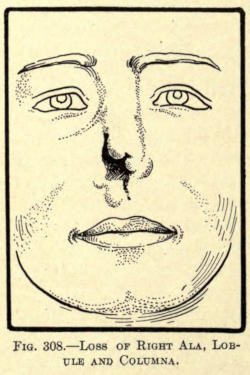
Fig. 308.—Loss of Right Ala, Lobule and Columna.

Fig. 309.—Loss of Lobule, Inferior Septum and Columna.
A fair idea of typical deformities may be obtained from the following illustrations in which deformities from the milder to the most extensive extent are shown. The types here shown are all pathological with the exception of Fig. 306, in which a saddle nose is illustrated[343] which may or may not be the result of disease or traumatism.

Fig. 310.—Ulcerative Loss of Right Median Lateral Skin of Nose with Involvement of Ala.

Fig. 311.—Loss of Nasal Bones and Partial Ulcerative Destruction of Dorsum, Lobule and Septum of Nose.
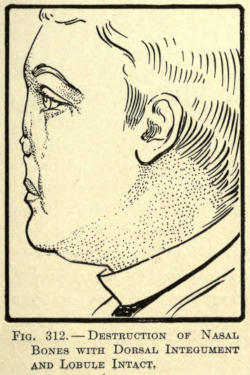
Fig. 312.—Destruction of Nasal Bones with Dorsal Integument and Lobule Intact.

Fig. 313.—Total Loss of Nose.
Many other deformities of the nose exist, of course, such as lateral deviation, twists, etc., but as in most of such cases cosmetic rhinoplastic operations and subcutaneous injection are required for their correction, inasmuch as in these cases the skin is healthy and intact, they will be considered under that part of the chapter that has to do with purely cosmetic rhinoplasty or under the chapter on subcutaneous protheses.
Before going into the individual methods involved in the correction of deformities of the nose, it is well here to go into the special details required for the performance of operations about the nose proper.
Anesthesia.—It may be well here to state that many of the smaller or cosmetic operations can and should be done under local anesthesia, and that the anterior nares should be plugged to prevent the blood from running into the pharynx, but in operations of greater extent the posterior nares should be plugged by Bellocq or other method, and that since the patient must be placed under a general anesthetic, some special plan must be followed to give the same.
The author has found no special apparatus on the market for this purpose. A most practical apparatus may be made as follows: A medium hard piece of rubber is cut into such shape as will fit into the patient’s mouth between the lips and the teeth. In its center a hole is made, into which a metal tube is fixed to which a rubber tube of three-fourth-inch diameter is securely fastened. This tube is connected by its distal end to the anesthetic container, which should be so constructed as to permit the required amount of air to be given with the anesthetic at the desired time.
Such an apparatus practically seals the oral orifice, and prevents blood from flowing into the mouth, gives[345] the operator a free field to work in without the encumbrance of large external mouthpieces, and is one that in case of vomiting can be easily removed for the time being, and be replaced without interference to the surgeon.
Preparation and Cutting of Nasal Flaps.—Under a division of skin grafting some preliminary steps in the preparation and cutting of a nasal flap has been referred to, but the author thinks it timely to repeat here the necessity for a systematic method of procedure.
It is well for the surgeon to have fully decided upon the certain operative plan he is to follow several days prior to the operation. He must, especially in total rhinoplastic cases, prepare a paper or oiled silk model of the flap or flaps he has decided upon to take from the forehead or cheek, and to fold and bend this model into the place of the deformity to be overcome, to make sure of the result to be attained, allowing for the loss, if any, of mass by reason of the torsion of the flap at its pedicle.
If the hair of the frontal scalp lies within the flap outline, it should be shaven away well beyond the border to permit of unhindered work.
Thoroughly cleanse and keep clean with a suitable antiseptic the parts to be operated upon for at least twenty-four hours.
Place a rubber cap over the hair of the head, or a fixed gauze or waterproof arrangement to keep it in place.
If there be any hair adornment of the face remove it.
The surgeon should remember to get the flaps to be utilized on forming the lost parts of the nose, at least one third larger to overcome the consequent retraction.
Sterilized sutures, preferably silk of suitable size, should be ready and be cut of such length as will facilitate quick action.
Rubber tubes of proper diameter for insertion into the nares should be at hand if required.
When all is ready the operator is to proceed quickly[346] and accurately, never changing his prearranged idea of the operation. His assistants should be ready to control by torsion or pressure the bleeding occasioned by cutting, since it covers the field of operation and hinders rapid work.
The surgeon in making flaps should use the greatest gentleness in handling them to prevent pressure gangrene. His finger tips are far better than fixation forceps. Sharp tenaculi may be employed with gentle traction only. Never permit the use of serrated forceps in autoplasty.
In cutting, employ the rules laid down under the principles of plastic surgery, and in dressing flap operations such methods as have been heretofore described.
Dressing.—Do not be too hasty in dressing such wounds, as early interference often results in partial if not total loss of the flap.
The author has found that in flap operations blood dressing under perforated rubber tissue is best. This helps to give nutriment to the parts and permits of free removal of the dressings. Never apply the blood treatment on gauze, since the latter is liable to become hard and attached to the suture lines, requiring undue force for its removal.
Care of the Nares.—Remove all packing from the nares before fixing the lobular section of the flap, and have all bleeding controlled before suturing the part of the flap intended for the columna. Blood clots tend to pressure and infection. If nare tubes are used rather let them remain in place for some time than to drag them forth forcibly.
The interior nose and nares can be kept clean by gentle irrigation through them.
Number of Operations.—Instruct the patient as to the probable outcome of the operation, and advise him that more than two or three operations may be necessary to correct the deformity.
Von Esmarch has said that twenty operations about the nose are none too many if the desired result can be obtained. Dieffenbach has said that it is more difficult to restore smaller nasal defects than those of greater extent.
The latter applies particularly to cosmetic operations in which the surgeon is compelled to work through small openings or incisions always with the view of leaving little if any scar, and to place such scar where it may be least observed.
The best cosmetic surgeon is he who can accomplish results with the least secondary disfigurement.
When for any cause there is a loss of the entire nose, and the patient is unwilling to undergo surgical operation for its restoration, the surgeon may resort to the use of protheses or artificial noses.
Such noses are made of papier-maché, rubber, wood, or light metal, and painted to imitate the color of the skin of the individual. They should be made after a model previously prepared by molding the new organ upon the face of the patient or after such patterns as the surgeons may have to choose from, fitting the skin juncture accurately in such cases.
If the surgeon lacks such artistic ability, a sculptor should be employed to model the proper organ suitable for and on the face of the patient, from which a plaster cast or mold may be made from which the maker of protheses can work.
With the model in hand and no expert on protheses within reach, a skillful surgeon-dentist could easily make a vulcanized rubber nose, which may then be painted to suit.
Some method of attachment must be provided for, such as one or two soft rubber plugs or stems to fit into[348] the nasal orifice or permanent fixture to the bridge of a pair of spectacles. Gums or pastes as advised with aural protheses may be of service.
Celluloid protheses should never be used because of their inflammable nature; furthermore, they are easily damaged or cracked. Wax noses are of little use, although resembling the normal very closely; they crack easily, and when soiled by dust or friction soon have to be replaced with new ones.
The following list of authorities shows the various materials employed by them for nasal protheses:
Martin—Porcelain.
Richter—Wood.
Debout—Rubber or silver covered with colored wax.
Mathieu—Aluminum.
Charrière—Silver.
The plastic surgeon is often, especially in later years, called upon to attend to traumatic injuries of the nose. Sometimes there is a total severance of the nose; often a partial loss or injury, practically involving a loss of a part of the organ. Since the advent of the automobile such accidents are not unusual.
The author has found that a remarkable history lies back of the replanting of parts or all of the nose when found detached by accident or intent.
If the part cut from the nose or face has been not too severely bruised, it should be cleansed gently in a normal salt solution at about 100° F., and be sutured in place as quickly as possible. Partly separated sections should be treated in the same way. It is remarkable how Nature will take care of these traumatisms. So well did the executioners in India, where nasal amputation is a criminal sentence, know this that they destroyed the amputated organ by fire, so that the victim could not replant it upon himself.
Chelius successfully replanted a nose after it had been severed about an hour.
Hoffacker has replanted a number of noses cut off in the duels of Heidelburg students. In one case one and a half hours intervened between the accident and the operation.
In partial separations about the nose the flap, still hanging by a slight pedicle, should be brought in place by suture, and because of the peculiar hypertrophy that always follows the wounds one or two intraflap sutures should be employed to fix the part centrally to the deeper tissues, if any, to prevent the formation of clots that are liable to organize and encourage such enlargement.
Such sutures are only to be made when the flap is of sufficient size to necessitate them. If the hypertrophy or hyperplasia cannot be prevented by this means later cosmetic operations should be employed to make the parts heal into normal contour.
Blood dressings should be employed after the parts have been fixed by a number of fine silk sutures, the coaptation being made as neatly as possible to get the best results.
The making of a nose or part thereof from a nonpedicled flap of skin taken from the patient has met with more or less success in the remote past, but of later years such methods have fallen into disuse because of the many and better methods of modern times involving the use of flaps with nutrient pedicles.
Branca is said to have made a nose for a patient out of the skin of the arm of a slave.
Velpeau states that “In the land of the Pariahs the men in power had no scruples in having the nose of one of their subjects cut off to replace the lost organ of another.”
Van Helmont is said to have made a nose for a gentleman from the skin of the buttocks of a street porter.
Bünger, of Marburg, in 1822 made a total nose from the anterior thigh.
Several surgeons later than the above date have successfully restored parts of the nose by transplanting skin flaps from remote parts of the body, the method involved being practically what is now accomplished by the so-called skin-grafting methods of nonpedunculated flaps heretofore referred to.
While for small defects such procedure has proven quite successful, the employment of large flaps for nasal reconstruction has been exceedingly discouraging, although the author advises trying transplanting of such flaps when the patient hesitates giving up sufficient facial skin for rhinoplastic purposes for fear of disfiguring scars, or when there are untoward reasons.
In such event there is only the secondary wound to be considered apart from the death of the flap, and the minor operation about the remains of the nasal organ to permit of the fixation of the latter.
A thorough and practical knowledge of skin grafting is of the greatest necessity to the surgeon, because he must be ready to cope with any emergency in such cases, and thus be able to save a flap graft from death or partial gangrene, when he would otherwise fail.
The most practical and safe methods of rebuilding the nasal organ have been those in which flaps having nutrient pedicles have been employed, whether these flaps be taken from the skin of the forehead, cheek, or both. These procedures are autoplasties, and may be grouped according to their peculiar differentiation into three classes, as follows:
The Indian or Hindu Method, in which the flap is made from the forehead.
The French Method, in which the flap is made from the tissue about the borders of the deformity.
The Italian Method, in which the flap is taken from some distant member or part of the body.
Furthermore, there are the combined methods of one or the other in which inverted skin flaps are used, or those lined with an osseous and cartilaginous support, and in some rare and rather unsuccessful cases by metallic supports.
The method of rebuilding the nose by taking one or two flaps from the forehead dates back to the Koomas, from whom the art of rhinoplasty has come down to the present time, all of the methods of to-day involving the utilization of the pedunculated flap being a result of their early surgical ingenuity.
Originally, their operation consisted of cutting an oval flap, having its pedicle as the root of the nose, and extending over the forehead, and upward vertically into the hair line. The flap thus made was dissected away from the bone and brought down by twisting it to the extent of a hundred and eighty degrees on its pedicle in front of the nasal deformity, the edges of which had been prepared to receive it. To hold the flap in position they resorted to some kind of clay, sutures being unknown to them.
The pedicle was cut after the flap had thoroughly united to the freshened borders of the deformed nose.
The steps of the operation as performed by them are shown in Figs. 314, 315, and 316.
Naturally, many improvements in the above method have been evolved, principally to overcome the extreme and injurious torsion of the pedicle, and from the desire on the part of the surgeon to bring about a better cosmetic[352] result. Therefore, not only the position of the pedicle and its shape were altered, but also the size of the flap itself, as will be shown in the specific methods of the various authorities mentioned hereafter.
The author does not consider it necessary to go into chronological details of the evolvement of the art, and begs the surgeon to be content to learn of those operations and methods that have given the best result.
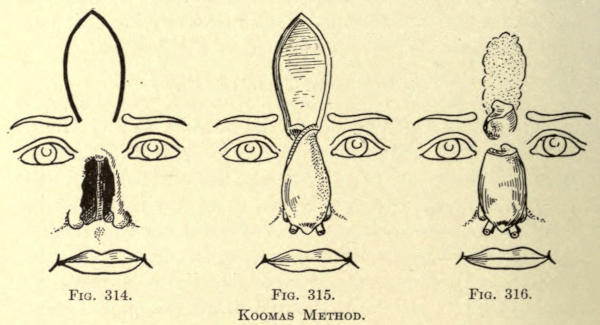
Fig. 314. Fig. 315. Fig. 316.
Koomas Method.
Where one surgeon has changed his incisions in the slightest direction and another has advised increasing the number of sutures is of little import to the operator of to-day; the gist of it all is the successful method for the successful outcome.
The first to be considered will be those methods wherein the vertical direction and the position of the pedicle have been similar to that of the Koomas. It will therein be noted that the principal change has been in the formation of the distal end of the flap with the object solely of forming a better base to the nose.
Graefe Method.—The flap was made in the shape of a heart with a rectangular addition at its upper or scalp border. The pedicle is made to lie between the inner limitations of the eyebrows (see Fig. 317).
The flap is twisted into position and sutured into the freshened remains of the nose, the pedicle being cut at a second operation after the flap has healed into place, which was about the tenth day.
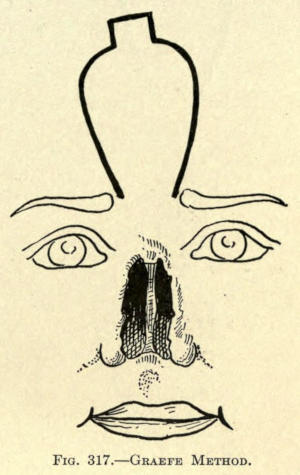
Fig. 317.—Graefe Method.
Delpech Method.—The shape of the frontal flap was cut in the form of a trident, as shown in Fig. 318.
The object of the arrangement was to give a rimlike lining to the two nostrils, the raw surfaces of the outer points being brought into contact with each other.
He also hollowed out a groove at the root of the nose, to better accommodate the pedicle when twisted. The steps are shown in Figs. 319 to 321. The pedicle was later severed when the conditions warranted it.
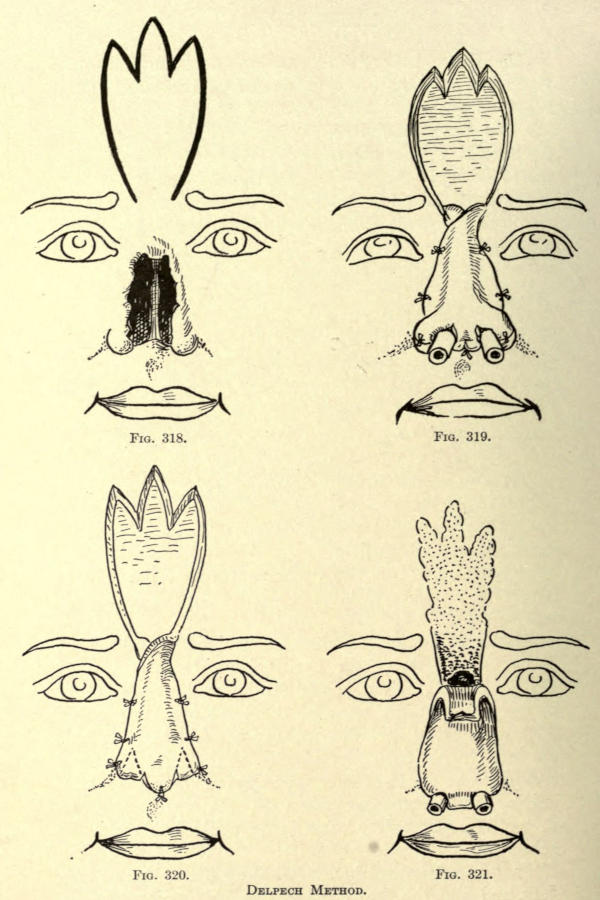
Fig. 318. Fig. 319. Fig. 320. Fig. 321.
Delpech Method.
Method of Lisfranc.—Lisfranc conceived the idea that if he carried down the one incision for the flap at the root of the nose somewhat lower than the other he would overcome some of the torsion at this point. This he consequently did, making the left incision half an inch lower than the right. The lateral incisions ascend at an angle of forty-five degrees (see Fig. 322), uniting in rectangular form at the scalp line, as shown, the rectangle of skin being utilized to make the subseptum.
Instead of sutures he dissected up the old nasal borders and slid the flap borders into this groovelike arrangement, holding it in place with the aid of sticking plasters.
With the above method the pedicle was allowed to remain intact. Fig. 323 shows the position of the flap, and the treatment of the subseptal section.
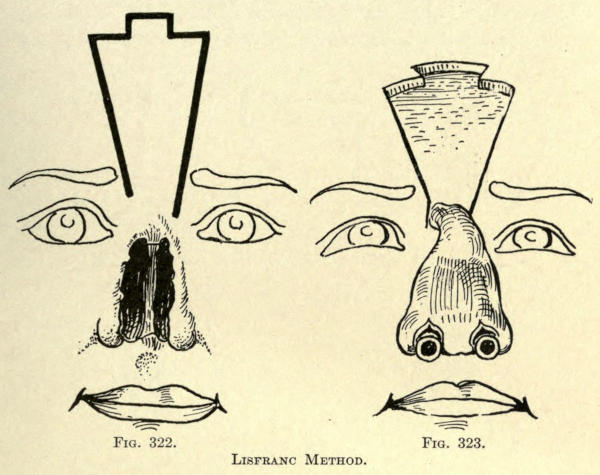
Fig. 322. Fig. 323.
Lisfranc Method.
Labat Method.—Labat uses a frontal flap shaped as in Fig. 324. The left bordering incision is carried down one half inch below the point of beginning on the right and carried downward in such manner that its lower point lies in a line with that of the right above it.
The object of this was to overcome torsion, and, where obtainable, the small triangle of healthy tissue at the root of the nose, as shown in the illustration, was dissected off from above downward, and turned downward with the cutaneous side facing the nasal chasm and its dissected side facing that of the flap. He avoids injury to the angular artery, as should be done in all cases. The pedicle was replaced at a second operation.
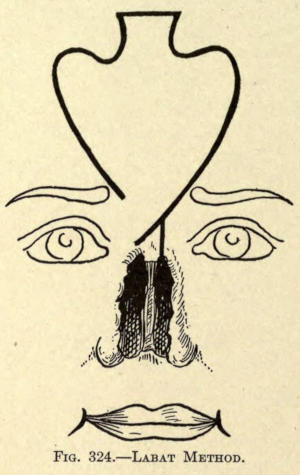
Fig. 324.—Labat Method.
Keegan Method.—Utilized a flap, shaped as in Fig. 325. The pedicle occupies the internal angle of the eye, care being taken to preserve the angular artery. The flap is mapped out obliquely, not perpendicularly. To get the best results he advises pasting a paper model upon the forehead to guide the operator in making the flap, which includes all the tissue down to the periosteum. Horsehair sutures are employed to approximate the parts accurately. The pedicle is divided in about twenty days, and a wedge-shaped piece of skin is excised at the root of the nose to prevent the tuberosity at this point of the new nose, so commonly observed with Indian-flap methods.
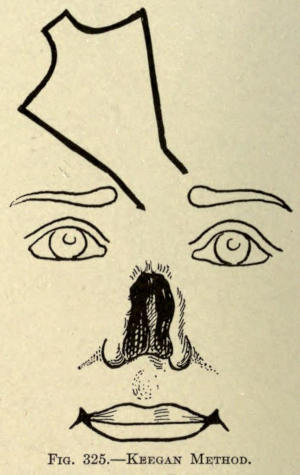
Fig. 325.—Keegan Method.
Duberwitsky Method.—The flap at its root resembles that of Labat, but at its superior border it formed an oval with an elongated point running into the hair line, which he divided, as shown in Fig. 326, to form the subseptum and nasal wings.
At the root the pedicle was about half an inch wide made in the oblique.
The middle section of the superior pointlike projection and intended for the subseptum was folded upon itself or doubled, as it were, to give support to the nasal point. The same was done with the alar or lateral sections, so as to line the nares with epitheliar surface to prevent contraction. The lower part of the nose was fixed into position by a harelip pin inserted transversely after all parts of the flap had been sutured into place.
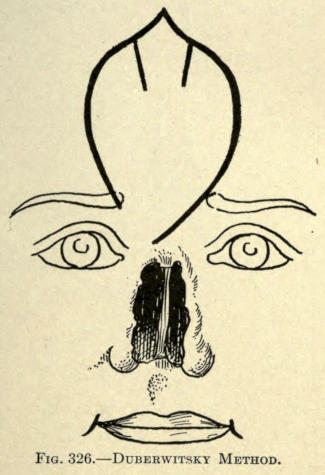
Fig. 326.—Duberwitsky Method.
Dieffenbach Method.—The flap is cut very much like that advised by Lisfranc, being wider only at its upper extremity, as shown in Fig. 327.
He advocates removing the remains of the old nose, almost circumscribing the nose, as shown in the illustration, except for the deep linear incision at the base of the nose on a level with the oval fissure,[358] leaving a bridge of skin at either angle into which the square or septal part of the superior frontal flap is affixed.
The flap is made so that the right oblique line lies an inch above that of the left, the latter incision running into the angle formed at the root of the old nose caused by the ablation.
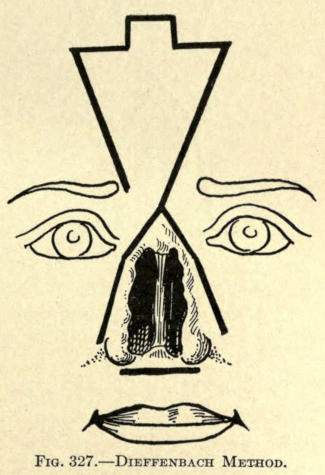
Fig. 327.—Dieffenbach Method.
Von Ammon Method.—The flap is cut at its superior border, similar to that of Keegan, but made in the perpendicular; the point of beginning, at the end of the right eyebrow, lies about an inch above the end of the incision of the opposite side, but in line with it (Fig. 328). The same method of removing the remains of the old nose advocated by Dieffenbach is followed as well as the lobial incision to receive the septal section.
The shape of this flap permits of bringing the secondary wound on the forehead more readily than where square exsections are resorted to.
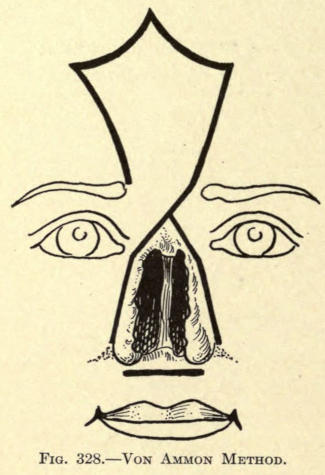
Fig. 328.—Von Ammon Method.
Auvert Method.—Like the method of Keegan, the frontal flap is made at an angle of forty-five degrees instead of the perpendicular, the flap being cut to the left of the median line. Its outline is shown in Fig. 329, and differs little at its superior extremity from that of Labat, except that it is made longer and narrower. The left lateral incision runs into the superior border of the old nose at the median line.
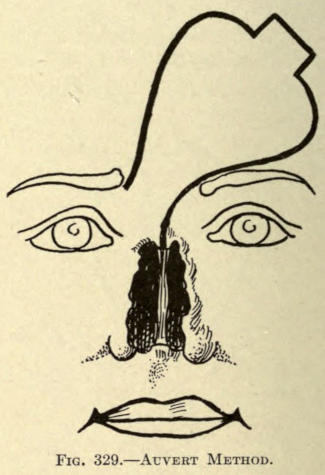
Fig. 329.—Auvert Method.
Von Langenbeck Method.—The flap is fashioned like that of Duberwitsky, but the left lateral incision enters the remains of the old nose, as Dieffenbach advised. The superior border was shaped, as shown in Fig. 330, to form the alæ and columna.
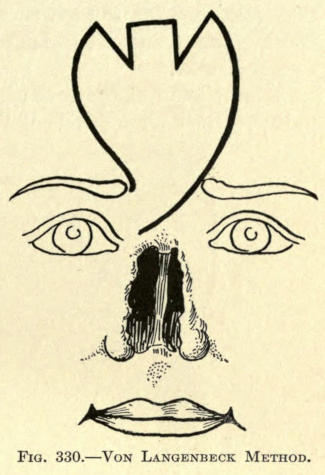
Fig. 330.—Von Langenbeck Method.
Petrali Method.—The shape of the flap is cut in ovate form with its rounded base near the hair line of the forehead. Petrali likens it to the form of the mulberry leaf. The left lateral incision dips down into the median line of the old deformity at its upper border.
The flap, after having been cut free, is folded upon itself along the median line, bringing the raw surfaces together along the dorsum of the new nose, thus giving body to the whole anterior nasal line. Presumably he introduces several sutures through the side of the flap to facilitate union along this line.
The method is illustrated in Figs. 331 and 332.
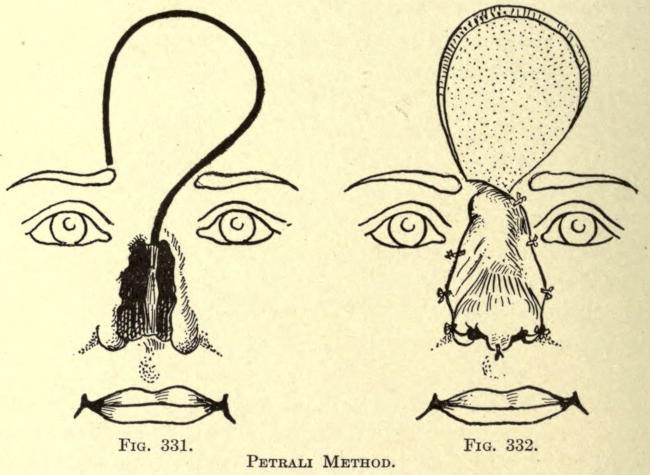
Fig. 331. Fig. 332.
Petrali Method.
Forque Method.—Herein the right lateral incision of the frontal flap is begun at a point above and corresponding[360] to the middle of the eyebrow. The base is fashioned as shown in Fig. 333, and the left lateral incision is carried down to the median line of the old nasal defect, coming within the inner border of the eyebrow.
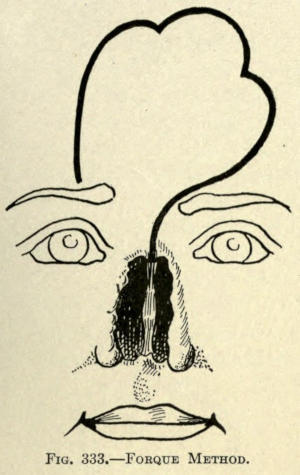
Fig. 333.—Forque Method.
D’Alguie Method.—This author conceived the idea of further relieving the torsion of the pedicle by making the frontal flap transverse along the forehead, instead of perpendicular.
The incision at the root of the nose is on a level and in line with the inner ends of the eyebrows. The left lateral incision is made to lie just above the eyebrow and the right sweeps upward and outward, as shown in Fig. 334.
The base is made with a rectangular projection to form the columna.
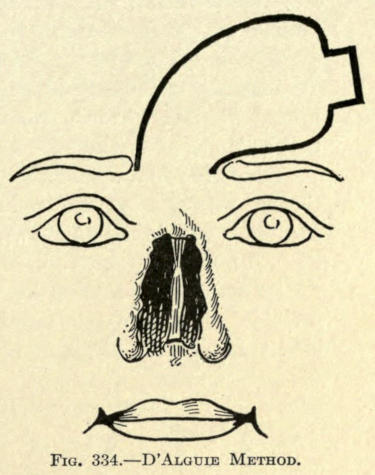
Fig. 334.—D’Alguie Method.
Landreau Method.—The direction of the frontal flap is transverse, but the root of pedicle, instead of having a downward direction, is so cut as to have its attachment upward, as shown in Fig. 335. This position of the pedicle thus overcomes to a great extent the torsion at this point. The flap must be cut somewhat longer in its transverse axis to allow for the higher position of the pedicle on the forehead.
The distal end of the flap is trident-shaped, as shown.
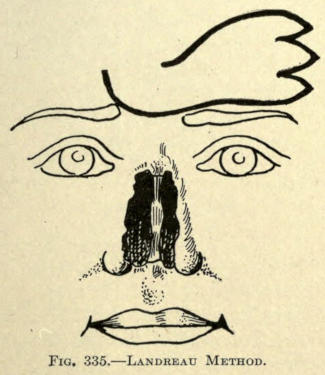
Fig. 335.—Landreau Method.
Langenbeck Method.—The flap is cut on an oblique line along its left border, running the incision down and across the root of the nose to the right while the right incision begins just under the eyebrow and extends less obliquely upward, as shown in Fig. 336. The base of the pedicle is fashioned as shown. The bordering remains of the old nose are removed.
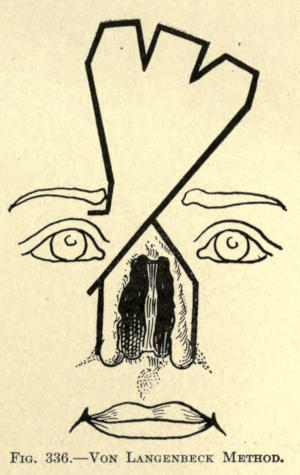
Fig. 336.—Von Langenbeck Method.
In another operation by the same operator the right incision was begun at a point above the eyebrow and carried transversely along to the rising point of the lateral. The left lateral incision was so made that it left an area of skin over the root of the nose, as shown in Fig. 337, which he dissected away, giving that part of the flap to cover it an opportunity to adhere, at the same time furnishing a nourishing area for its future life.
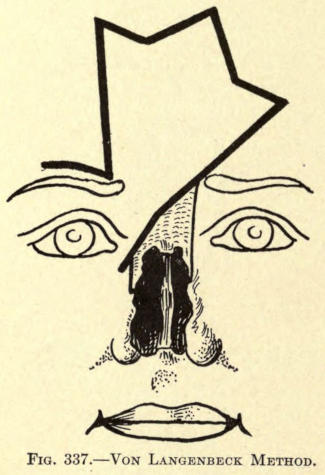
Fig. 337.—Von Langenbeck Method.
Szymanowski Method.—The flap is formed as shown in Fig. 338, the pedicle having its upper incision just below the end of the right eyebrow and the lower below the inner canthus on a line with the first, giving it an oblique position.
Just below the curvature of the basal incision two short incisions are made on either side into the forehead tissue with a view of rendering more flexible the skin to be utilized in correcting the secondary wound. The margin of the old nose is freshened.
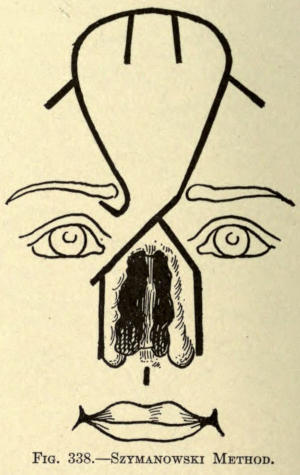
Fig. 338.—Szymanowski Method.
Labat, Blasius, Linhart Method.—These operators performed their operations in two sittings. In the first the incisions were so made at the base as to permit of that part of the flap intended for the rim of the nares to be tucked in, as it were, where these two triangular little folds were held in place by silk suture. When the parts had become thoroughly united, or at the second sitting, the entire flap was cut away and brought into place for the new nose. The object of this procedure was to give body to the wings of the nose and to overcome the consequent curling and contraction of the skin so commonly found with the single sitting operation.
This step marked the first advancement toward attaining much more successful results in total rhinoplasty by using skin-lined flaps, which not only added to the better nutriment to the part, but also gave support and firmness to the new organ.
This method, per se, is not in itself sufficient to bring about a satisfactory result. The fundamental principle is that of the sliding flap of Celsus, and in which the two flaps intended to form the new nose are taken from the tissue of the cheek at either side of the remains of the old nose.
The total outcome is simply to bring before the opening a curtain of skin with a median scar running from[364] the root to the lobule, which in itself is sufficient upon contraction to mar the result; furthermore, there are the two lateral wounds which have to be covered by skin grafts which, upon healing, have their tension of contraction, added to that of the median scar, with the result that the anterior nose becomes flattened and ugly, practically amounting only to an unevenly contracted curtain of marred skin.
The author would not advise resorting to such method, but, owing to the fact that a step in the advancement of the art was conceived under this particular method, space is given to the subject. This step, first introduced by Nélaton, consisted of allowing all of the cicatricial tissue of the old nose to remain with which the new nose could be built. As the possibility of this is rare in total rhinoplastic cases, the method is more useful in partial rhinoplastics, where it forms an important factor, as will be shown later under that subdivision.
Nélaton Method.—Two lateral flaps of triangular form, having their pedicles below the internal canthi, are cut from the cheeks, each flap containing all of the remains of the old nose. The entire inner borders of these flaps were freshened throughout their whole thickness.
In making the flaps, dissection is made down and through the periosteum, thus giving firmness and thickness to the new nose. The flaps are slid forward and sutured along the median line, leaving a triangular wound of the cheek on either side, as shown in Fig. 339.
To keep the raw surfaces in contact with the newly dissected area and to retain the nose in place as far as possible, a silver pin is inserted through the base of the new nose, going through the skin and remains of the old nose. It should be of sufficient length to permit holding a disk of cork at either end, beyond the skin and for the retention of the metal ring ends of a hook bent in inverted U-shape. The diameter of the latter bent wire is equal to that of the pin.
He claims for his method a perfect and fixed cicatrization of the newly placed parts.
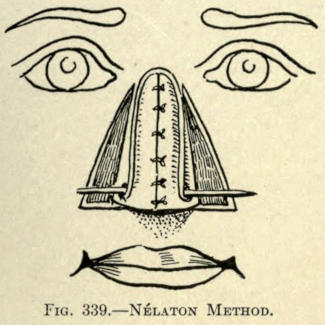
Fig. 339.—Nélaton Method.
Heuter Method.—The cheek flaps are cut from the cheeks, as shown in Fig. 340, leaving intact a triangular piece of skin with the object of giving support to the new nose. The inner and upper borders of the two flaps were stitched to the rim of this triangle, and then along the median line. The flaps are not made to include the periosteum, as in Nélaton’s method. The results thus obtained are not equal to the latter’s procedure.
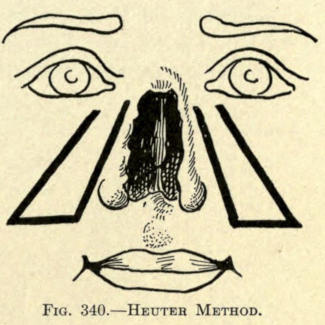
Fig. 340.—Heuter Method.
Bürow Method.—The cheek flaps are made as in Fig. 341. The projection intended for the subseptum is an elongated strip at the inferior border and inner angle of the left flap.
The shaded triangles at either extremity of the outer incisions show the removal of the skin at these points, to facilitate sliding of the flaps, adding, however, to the[366] extent of cicatricial contraction upon final healing, with the resultant flattening of the new nose. The lobular prominence takes an upward position eventually, and altogether the extensive secondary wounds and the effect of their behavior does not warrant the use of this method.
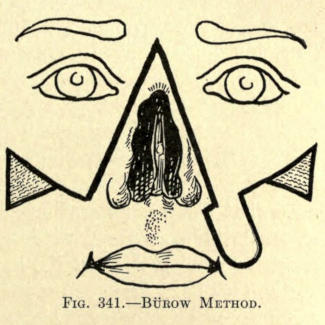
Fig. 341.—Bürow Method.
Szymanowski Method.—His method is an improvement on that of Bürow. The flaps, inclusive of considerable cellular tissue, are fashioned in Fig. 342, except under the two narrow extension flaps, which are to be utilized in building up the subseptum. Their raw surfaces are sutured together with silk. The flaps are united along the median line.
If the tissue from the cheeks do not permit of free sliding forward of the flaps, further incisions shown by the dotted lines over each malar prominence are made. The skin of the shaded irregular areas on either side is removed, as in the Bürow method.
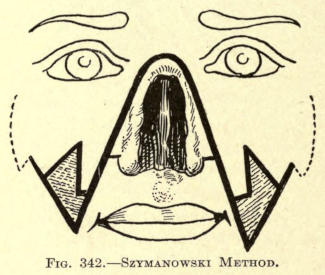
Fig. 342.—Szymanowski Method.
Serre Method.—The flaps are made to either side of the remains of the old nose, each leaving its pedicle about one fourth inch below the inner canthus of the eye. The flaps were cut rather obliquely, their bases extending somewhat below the nasal orifices. The remaining skin of the latter was dissected downward and folded down upon the median third of the lip. If cut in two sections their inner borders were sutured so that their raw surfaces faced each other. The object of the latter step was to form the subseptum, according to Lisfranc. The sections of skin lying with their bases on a level with the nasal orifices were dissected downward and united[367] in the median line to assist in forming the end of the nose. All along the borders of the old nose were also dissected up where possible and folded inward, so that their raw surfaces would adhere to the new dorsum of the nose, and thus give it stability and form. These pieces of skin were united at the median line when possible.
The cheek flaps with indented bases were now brought forward and united, as shown in Fig. 343. The skin of the cheeks was dissected up to the extent of the dotted line in the former illustration, and when necessary two lower curved incisions were made to permit of free sliding. The skin of the cheeks was retained by three sutures at either side, as shown in Fig. 344. The subseptum may be made at the same sitting, or at a later operation.
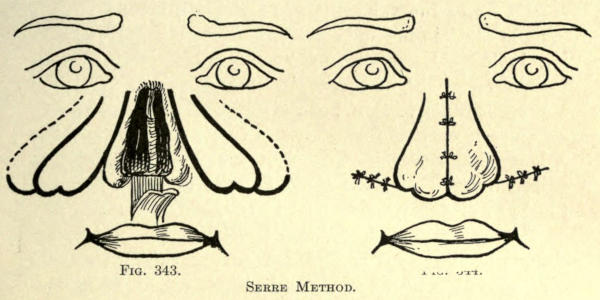
Fig. 343. Fig. 344.
Serre Method.
Syme Method.—The procedure is very like that of Heuter, except that the somewhat curved line making the inner borders of the flaps extended over the root of the old nose. The lower ends or bases of the two cheek flaps were stitched around and to the orifice to form the end of the nose, rubber tubes being used to form the nostrils, where they were retained until healing was complete.
Blasius Method.—He forms the cheek flaps in triangular form, including all of the tissue making up the buccal[368] cavity. The outer or cheek incision is made through all of the tissue and extends to a point corresponding to a point a given distance beyond the angle of the mouth. The inner incision is made from a point just below the angle of the ala downward and through the thickness of the lip. A third incision unites the angle of the mouth with the outer incision. Both cheek flaps are made alike, each remaining attached along all of the remains of the old nose. They are now raised upward and inward, with their mucosa facing outward, and united along the median line. The raw cheek borders are now brought forward and held in place by suturing them at either side to the remaining rectangular flap of the upper lip. The formation of the subseptum is left for a second sitting. This method is not only too extensive, but too disfiguring to make its employment practicable. The mucous membrane would, of course, in time take on the function and appearance of skin, but the shape of the mouth never assumes a normal form, especially since there is quite a loss of the vermilion border at either side which is raised upward with the cheek flaps to assist in forming the base of the nose.
Maisonneuve Method.—Where there is more or less occlusion of the nares and yet an integumentary covering corresponding to the nose, as it might rarely be in congenital cases, Maisonneuve utilizes the sliding flap method to overcome the abnormality. In the case presented, the nasal orifices were hardly three sixty-fourths of an inch in diameter and about one inch apart. The correction was accomplished as follows, and shown in Fig. 345: An incision was made transversely outward from each nostril, then two converging incisions were made from both nares downward, meeting at the vermilion border of the lip in the form of a V, which were made to include the whole thickness of the lip. This flap was brought upward to form the subseptum. The skin to form the nasal lobule was now slid forward from either end of the[369] incision and the subseptum sutured in place. Rubber tubes were employed to keep the nares distended and permit of the wings of the nose to form.
The defect in the upper lip was brought together as in a median harelip operation, the parts appearing after operation as illustrated in Fig. 346.
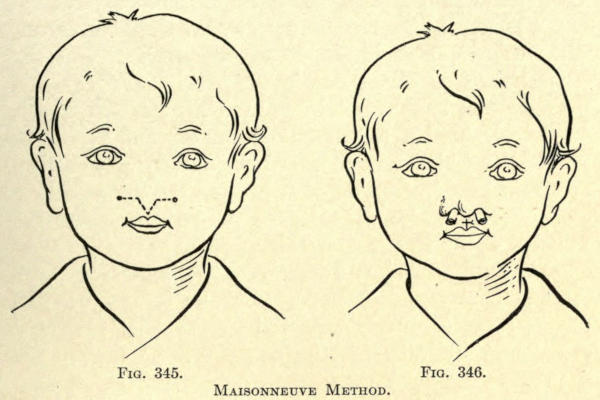
Fig. 345. Fig. 346.
Maisonneuve Method.
In this classification of total rhinoplasty the skin flap is taken from another part of the body and not from the face. The integument of the arm is usually employed, the pedicle remaining intact until the flap has healed into place.
The method has been accredited to the Italian author-surgeon Tagliacozzi, but it was practiced long before his time; yet he was the first to fully describe the steps of the successful operation. It has been referred to quite fully under skin grafting.
The flap having an attached pedicle is cut from the entire thickness of the skin of the arm. The free end of the flap is sutured to the freshened borders of the old[370] nose, and the arm is held in place until union has been established, when the pedicle is cut. There are no special advantages in this method, since the outcome is no better than that obtained with the Indian method; at best the result is merely the curtain of skin covering the defect, with the one thing in its favor—the avoidance of the frontal scar. Against this is the great discomfort the patient must suffer in having his arm retained in the necessary position to prevent movement and strain on the flap, to which may be added the danger of embolism occasioned by freeing the arm at the time the pedicle is cut. There is also difficulty of properly dressing the wounds, owing to the constrained position which consequently invite sepsis and imperfect healing. Hence, for total rhinoplasty, this method may be termed unsatisfactory; yet for certain partial rhinoplastic results it supersedes all other methods, as will be hereinafter shown.
To make the flap a pattern is laid upon the skin, from which it is to be made; it should be one third larger than the actual size of flap needed, to allow for contraction. The incisions should go through the entire thickness of the skin, leaving an attachment or pedicle, what in this case would be the part of the flap intended for the base of the nose, and directly opposite to those described heretofore.
The flap may be sutured in place immediately after the cutting, or it may be allowed to remain upon the arm until contraction has taken place in the flap, or the flap may first be modeled into nose shape and then sutured upon the freshened margins of the old nose.
The arm must in any of these methods be held in place during the days required to have the flap heal or unite with the facial tissue. The various operators have devised means to accomplish this. There is the linen network of bandages of Tagliacozzi, the harness of Berger, the starched linen and book-board affair of Sedillot, the[371] one-piece suit of Lalenzowski, the leather sleeve and helmet of Graefe and Delpech and many others.
Having determined upon the method to be followed in securing the flap, the surgeon is advised to consider such apparatus as he may be able to procure to retain the parts, or to use his own ingenuity to construct one of plaster-of-Paris bandages to meet the requirements of the case at not only less expense, but with greater comfort to the patient. At best, any apparatus employed will do little to overcome the agony of the retained member, which must be held in position.
Various operators give this period between six and twenty days. The apparatus should be so constructed that dressings can be easily made without discomfort to the patient, and without doing damage to the parts, and also to expose the face of the patient as much as possible. The various operations employed to perform total rhinoplasty by the Italian method may now be considered.
Tagliacozzi Method.—This surgeon resorted to four steps to accomplish his operations, which were:
I. Massage of or stretching the skin of the part from which the flap is to be made.
II. Cutting the flap, and allowing the same to cicatrize.
III. Freshening the flap and suturing in place, and use of apparatus.
IV. Cutting the pedicle and making the subseptum.
The various details of these steps should be considered here, since the methods are practically the same for all other operations of this kind, except in certain particulars as to time and mode of procedure.
I. Massaging the tissue of the arm to render it supple. This is of some consequence, in some cases, where the skin is tense, but requires no especial description.
II. He then compressed a fold of the skin with a large forceps at the lower half of the biceps. Upon opening these forceps he forced a bistoury under the skin fold[372] and cut down toward the elbow-joint a distance sufficient to form a flap. This gave him a piece of raised skin, attached at either end, double the size of that required to make the nose. Under this he introduced linen mesh dressings in the form of a seton, with the object of irritating the skin to encourage the circulation, and render it thicker by consequent suppurations and granulations. This was continued for fifteen days, when the skin was detached at its upper end, leaving it attached by the lower or wider pedicle intended for the base of the nose. The flap was now turned down and both flap and wound were allowed to cicatrize.
III. When the flap had become dry he fitted the linen bandage apparatus to retain the arm. Then the borders of the old nose were freshened. Thereafter he cut a paper pattern as a model for the new nose, upon which the margins and shape of the flap were cut. The flap was finally sutured in place, and the apparatus was tightened to prevent movement of the parts.
IV. After twenty days he cut the pedicle. The latter was then cut into, to divide it in three parts, which he formed into the subseptum and nasal wings, which were sutured in place, metal tubes being employed to keep the nares open.
Dieffenbach Method.—This surgeon followed seven steps to complete the operation, as follows:
I. The pattern of the new nose, cut one third larger, is fixed upon the skin of the arm, with the basic pedicle just above the fold of the elbow. Skin is now raised sufficiently to permit of its being incised, the incisions being made laterally, as shown in the dark lines in Fig. 347.
This gives a triangular flap, the apex lying upon the biceps and having two adherent pedicles at apex and base.
The base is now incised at one angle, transversely and again vertically, as shown. This incision liberates the part of the flap intended for one of the ala of the nose.
II. Diachylon plasters are placed under the flap to[373] contract the arm wound immediately the bleeding has been arrested. The free angle of the base of the flap is now turned inward and under the attached part of the flap, as in Fig. 348, so that its margin protrudes from the other lateral incision, and its skin surface lying above the plaster. The edges of the flap are now stitched together, and the flap is allowed to lie cushionlike upon itself while the arm wound heals. This requires about six weeks.
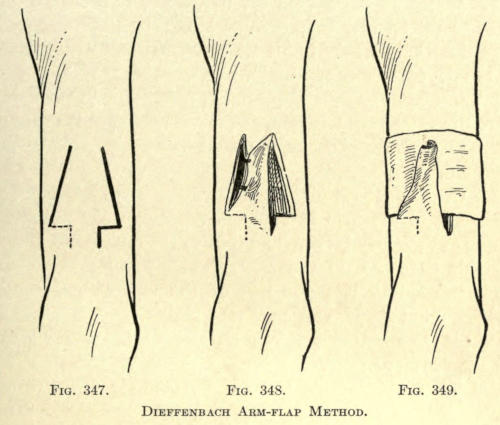
Fig. 347. Fig. 348. Fig. 349.
Dieffenbach Arm-flap Method.
III. The holding of the flap cushion in place by the use of splints of leather held in place by three needles. The latter are moved about, as the shape of the cushion becomes modeled, about every three weeks. The process ends when cicatrization of the flap or the newly formed nose has been accomplished, shown by firmness and contour.
IV. The margins of the old nose are freshened; the lateral incisions extend to the root of the nose, where[374] they are united with an upward convex incision. The skin is well raised, gutterlike, from the deeper tissue, to assure of the best vascularity.
V. The upper or apex pedicle of the flap on the arm is cut (see Fig. 349), and the thickened roll of skin, or what may now be termed the new nose, is turned down toward the elbow. It is divided along the line where the two margins of skin had been sutured; in other words, it is laid open longitudinally.
VI. The nose thus prepared is brought into place before the freshened margins of the old nose and is sutured into place beginning at the root before the sides are coapted.
VII. At the end of fifteen days the pedicle attaching the nose to the arm is severed, the angle for the wing being cut slightly larger than that of the other side, which by this time has, of course, undergone full contraction. The subseptum is made out of the square projection folded upon itself, raw surfaces facing, and is brought into place by suturing it into an incision made in the lip at the required point.
Graefe Method.—This surgeon devotes six steps to his operation, as follows:
I. The borders of the old nose are freshened.
II. Sutures are passed through the raised skin of the borders of the old nose.
III. The flap is cut from the arm after a pattern made one fourth larger than the new nose required, leaving it attached by the small pedicle intended for the subseptum.
IV. The sutures where required are now passed through the flap, having already been placed through the old nasal borders and left untied. The forearm is drawn against the forehead and the arm is fixed in place with the retention apparatus. The sutures are now tied. They are allowed to remain in about four or five days, not long enough to irritate.
V. About the tenth day the head apparatus is removed and the pedicle of the arm flap is divided. The arm may now be carefully lowered to its normal position.
VI. The subseptum is not formed from the free end of the attached flap for several weeks. It is then divided by two parallel incisions directed outward. The septal section is folded upon itself, and inserted and sutured in place into an incision made into the upper lip.
Szymanowski Method.—This author advises making the base of the flap sufficiently wide, and of the form shown in Fig. 350, to permit of the three sections of skin of this part of the flap to be folded upon themselves before being sutured in place at the base of the nose, so as to form lined nares and a thickened and supportative subseptum.
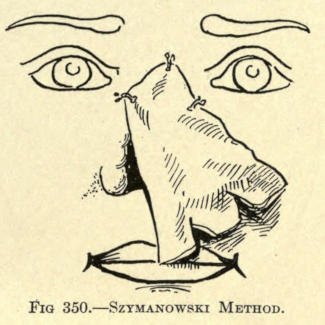
Fig. 350.—Szymanowski Method.
Fabrizi Method.—This author utilized the immediate method of flap fixation, but makes his flap of triangular form from the inner and upper skin of the forearm.
The transverse base is made to lie one half inch below the radio-ulnar space. The flap should be about three inches long and of about the same width. It is cut while the forearm is relaxed; bleeding is controlled by gentle pressure. In the meantime the cicatricial tissue of the old nose margins has been removed and the skin freshened to receive the flap.
To approximate the parts, the hand is laid palm down upon the shoulder; the resultant position of the arm and forearm are retained by bandages. The parts are now sutured. On the thirteenth day the line of division is[376] traced out upon the arm with nitrate of silver, at the same time giving the flap somewhat the form required to give the nose its contour.
The next day the pedicle is cut and the arm is brought back into its normal position. With the division of the pedicle he advises including a portion of the aponeurosis and a few fibers of the supinator longus muscle.
The flap is allowed to remain free at its base until contraction and cicatrization have been established, when the subseptum and wings are made.
The position of the arm and the attached flap at the root of the nose is shown in Fig. 351.
He advises, when possible, to dissect up a flap of the cartilage of the old septum, letting it adhere at its lower border and turning it from below upward with the skin which covers it to form the subseptum. This will help to hold up the point of the nose firmly (an important matter because it is at this point that all noses constructed of skin flaps alone sink down for the want of suitable prop of tissue).
This cartilaginous flap he held in place with two pins thrust through the latter and the skin flap proper, and held them in place with a figure twist of silk. He removed the needles about the sixth day.
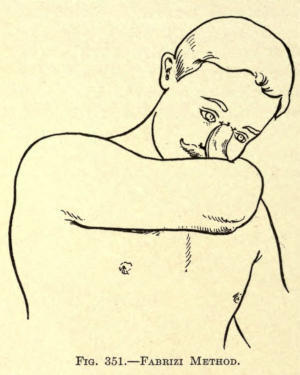
Fig. 351.—Fabrizi Method.
Steinthal Method.—This authority made the flap for the nose from the skin over the sternum, proceeding as follows:
“From the sternum I cut a flap of skin and periosteum in the form of a tongue whose lower base was five centimeters wide, and the summit forming the pedicle three centimeters wide; its length was twelve centimeters.
“I could have taken away with this flap some of the costal cartilage to utilize in making the wings of the new nose.
“I dissected up this flap and closed the wound over the sternum with sutures. The flap was then stitched to the forearm by its base into an incision of appropriate length made near the radius. (See Fig. 352.)[378] The arm was properly fastened in a plaster apparatus and the flap enveloped in a dressing of borated vaselin. The forearm was held in front of the breast, an attitude easily retained. Twelve days later I cut the pedicle.
“I let a few days pass by, and then stitched the pedicle end of the flap to the root of the nose. A new plaster apparatus was put in a suitable position. The hand was placed on the forehead.
“Ten days after, I detached the flap from the arm and reformed the nose with the flap, which hung down like an apron. It is necessary to have a flap sufficiently long to fold in for the nostrils. I used bronze aluminum wires for all the sutures.”
The position of the hand while the flap was healing to the root of the old nose and the slight twist of the flap is shown in Fig. 353.
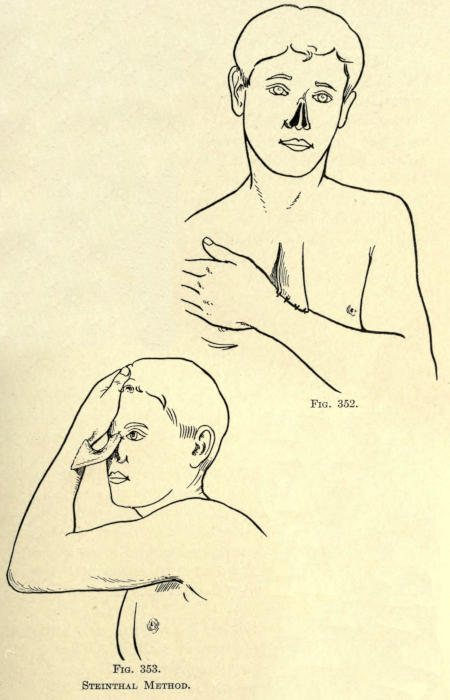
Fig. 352. Fig. 353.
Steinthal Method.
To overcome the consequent cicatricial contraction and falling in of the flap used to make the new nose by either of the three grand methods given, various surgeons have resorted to lining the flap with skin flaps, bringing their raw surfaces together so that the nose actually received in this way an integumentary lining.
While this had the tendency to thicken the new nose, it did not give the support necessary to it, especially at the lower third, and the lobule, at first quite satisfactory, resulted only in the appearance and form of a small tubercule of tissue, with a decided saddle effect above it. This combined method did overcome, however, the slow process of cicatrization, and its accompanying suppuration.
The raw surfaces of the two flaps, if properly brought together, healed upon themselves readily, as has been referred to in the lining or doubling in of the basal sections to form the nostrils and subseptum.
The method of lining the nasal flap in this manner is never sufficient to give a satisfactory result in total rhinoplastic cases, but may be of great service in restoring parts of the nose, as will be shown later.
The requirement is that of support, whether it be organic or inorganic, and these methods will be considered presently.
Volkmann Method.—This surgeon fashioned the frontal flap as shown in Fig. 354. This resulted in leaving a triangle of skin at the root of the nose, which he dissected up, down, to and inclusive of the periosteum, and turned downward so that its raw surface faced upward, as in Fig. 355. The flap was sutured into place to retain it.
The frontal flap was brought down, so that the two raw surfaces came together.
This method overcame the contraction of the flap over the nasal bridge or superior third of the new nose, and an excellent adhesion of that part of the flap to the denuded bone and flap resulted, but the same faults about the base were not mitigated.
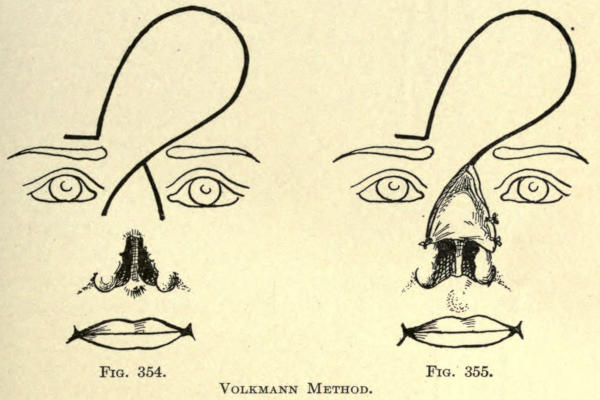
Fig. 354. Fig. 355.
Volkmann Method.
Keegan Method.—The frontal flap method of Keegan has been referred to. For the lining of the upper nose he cuts two flaps from the skin above the old nasal orifice, as shown in Fig. 356, which he turns down, raw surfaces out. This gave a lining to either side of the median line; the skin remaining intact between the two flaps gave additional prominence and support to the upper third of the new nose.
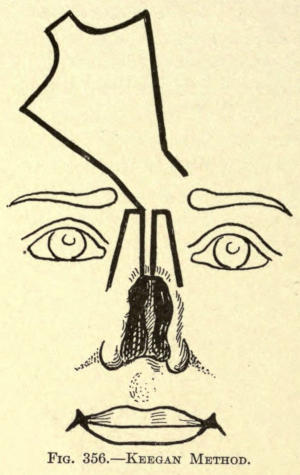
Fig. 356.—Keegan Method.
Verneuil Method.—Contrariwise to the methods just given, Verneuil, after cutting out the frontal flap, cuts the flap from the remaining sides of the old nose somewhat involving the skin of the cheeks, as in Fig. 357. This done, the frontal flap is simply[381] turned down, raw surface out, and the cheek flaps are slid over it, bringing the raw surfaces together. The inner borders of the flaps were sutured in the median line, as shown in Fig. 358. The base of the nose is made from the frontal flap by any of the methods already given.
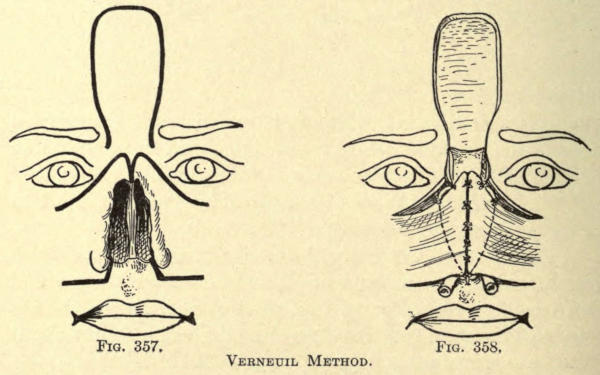
Fig. 357. Fig. 358.
Verneuil Method.
Thiersch Method.—The frontal flap is cut from the skin of the forehead in the shape shown in Fig. 359. Then two quadrilateral flaps are raised from the cheeks, as also illustrated. These are made wide enough that, when they were brought together, their inner borders could be made to face each other. In this position they were sutured along the median line, so as to give a double-gun-barrel form to the nose, with a septal wall between.
From the lower border the nostrils were formed, giving to the new nose a normal appearance, the continuous septum curving downward to form the subseptum, the whole being sutured to the remains of the old nose.
The frontal flap was now brought down over it, the raw surfaces facing each other, and sutured in place, as shown in Fig. 360. Later, Thiersch replanted the sides of the nose, to give it better contour, and attained a very[382] satisfactory result. The frontal wound was covered with skin grafts, but the cheek wounds were allowed to heal by granulation. The cicatrization of the latter was not sufficient to effect the lower eyelids nor the angles of the mouth.
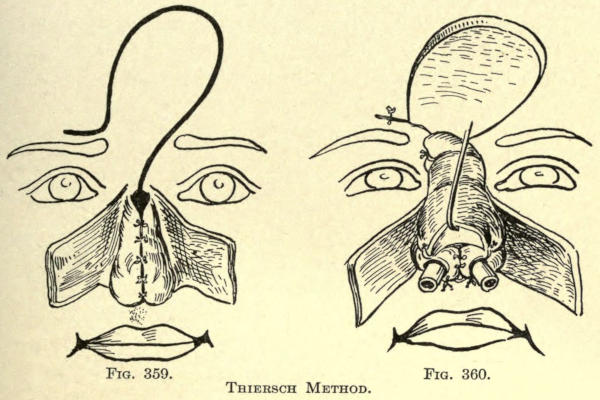
Fig. 359. Fig. 360.
Thiersch Method.
Helferich Method.—His is an ingenious application of the French method. Both flaps are cut from the cheeks; the lining flap was made from the left and the covering one from the right cheek. The shape of the flaps is shown in Fig. 361.
The lining flap is stitched along the freshened margin of the right side of the nose. The flap should be wide enough to give convexity to the nose, as shown in Fig. 362.
The covering or right flap, cut much larger, is now slid over this. It should be cut amply large to cover the flap just sutured in place. It is sutured on both sides of the nose to hold it in place, also at the inferior margin. The nose is lightly packed with iodoform gauze.
The pedicle of the right flap was cut after two and a half weeks and brought into place across the root of the nose, and sutured in place to give better contour to the part after freshening the skin about the left side of the nose at this point. He does not make a subseptum, but thinks the inferior base of the nose of sufficient size to hide the absence thereof.
The subseptum could, however, be readily made from the upper lip, as will be shown later.
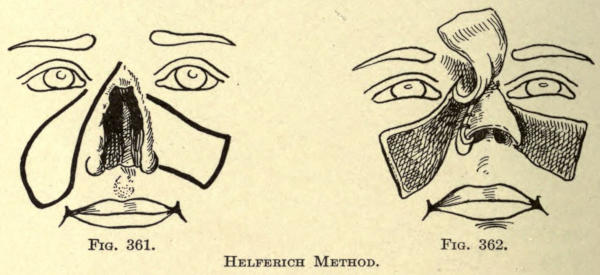
Fig. 361. Fig. 362.
Helferich Method.
Sedillot Method.—This operation is particularly efficacious in giving a splendid subseptum and support of the point of the nose, but does not overcome the falling-in of the whole anterior line, so common with all Indian-flap methods. A flap one centimeter wide and extending downward almost to the vermilion border is cut from the thickness of the upper lip, not including the mucous membrane, however. It is turned upward, as shown in Fig. 363.
The frontal flap is fashioned as shown, care being taken to cut a subseptal rectangle of greater length than usual, since it is intended to overlie the raw surface of the flap taken from the lip. It is rotated downward and sutured into place at both sides, and also to the lip flap, to assure of accurate union.
A lateral view of the nose as formed in this manner is shown in Fig. 364.
The free end of the septal flap is fixed into the superior lobial wound with a harelip pin. The lobial wound is sutured as in ordinary harelip operations. This method is particularly valuable in total rhinoplasties involving the columna and alæ in conjunction with flaps obtained by the Italian method.
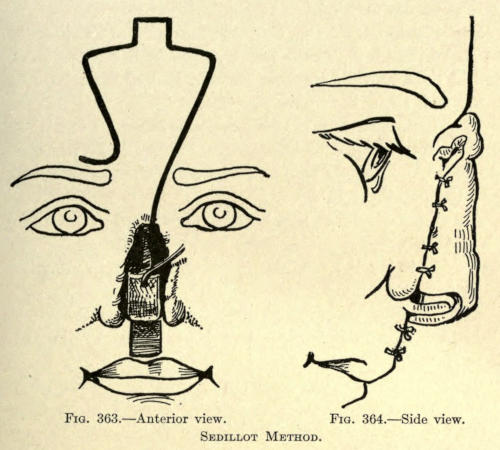
Fig. 363.—Anterior view. Fig. 364.—Side view.
Sedillot Method.
Küster-Israel Method.—A flap was taken from the arm by the Italian method, which was sutured to the remains of the old nose so that its raw surface looked upward, not downward, as in the ordinary case.
The flap was made sufficiently large to permit of building the wings and subseptum. After it had healed into place the pedicle was cut, and a frontal flap was cut from the forehead to cover it.
An unusually large flap was required to do this, since it had to overcome the greater curvature already given and added to by the arm flap, necessitating an extensive secondary wound.
The reverse order of procedure would be the more advisable for this reason, and is resorted to by the following:
Berger Method.—This surgeon makes the lining flap from the forehead. The secondary wound is at once closed. A flap is then made from the arm by the Italian method, and brought into place before the one just made. It should be of sufficient size to allow of building the base of the nose, which is done not later than three weeks after the pedicle of the arm flap is severed, which may be done at any time between the eighth and the twelfth day.
All the precautions are used as already given in the description of the Italian method. The arm is held in the position shown in Fig. 365.
Berger sutures the arm wound before bringing the flap into place upon the face to overcome the discomfort of suppuration to the patient.
The apparatus is fixed definitely after the patient has recovered from the anesthetic. Great care is exercised to prevent coryza from exposure. Dressings are made twice daily.
The pedicle is cut under local cocain anesthesia.
To make the subseptum and wings of the nose, the base of the flap is cut into three sections. The posterior surface is freshened and the parts are folded upon themselves and sutured into position.
Instead of employing rubber tubes, he resorts to a specially devised apparatus to retain two metal tubes in the nares, and at the same time make gentle pressure to the sides of the nose to mitigate the columna contraction. The latter is planted into a V-shaped incision made into the tissue of the upper lip at the proper place of attachment. The subseptum may be lined with[386] a flap of mucosa dissected up from the floor of the inner nose.
For the wings of the nose, such tissue as may be of service to give them stability and structure is taken from the remains of the old nose.
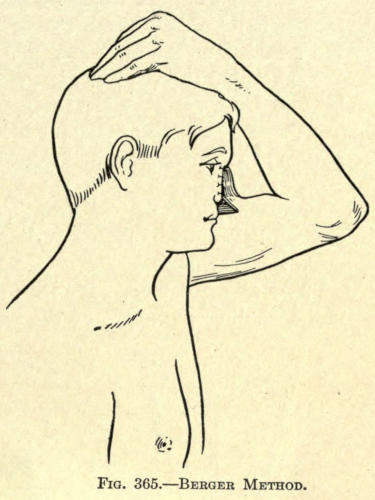
Fig. 365.—Berger Method.
The apparatus just mentioned and shown in Fig. 366 is used from the very first day until total cicatrization has taken place, and even for a longer period to aid in shaping the entire nose and the tendency to collapse has been overcome.
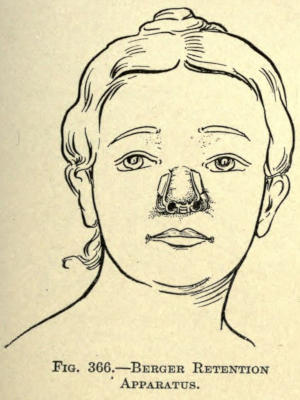
Fig. 366.—Berger Retention Apparatus.
Szymanowski Method.—A frontal flap, divided along the median line and shaped as outlined in Fig. 367, is made from the forehead.
Two triangular flaps are then raised from either side, and including the angle of the nose as shown. The divided frontal flap is now brought down in such manner that their raw surfaces meet, thus forming a vertical septum. The margins are united by suture, and the lower[387] ends are fixed into a wound made for the purpose at the base of the nose, as shown in Fig. 368, to form the new subseptum.
The lateral triangular flaps are dissected up so that they can be readily slid forward toward the median line. Their inner freshened margins are sutured to the raw edge of the septum just made, and to themselves. The objection here is that there is a liability of considerable contraction of these lateral flaps, with a tendency to fall in and drag with them the new septum; and again, in total restorations, the upper third of the nose is only partially covered, and necessitates later upbuilding. The author finds difficulty in making the four margins thus brought together unite evenly throughout, and that a vertical contraction is caused by the cicatrization of the median marginal wound.
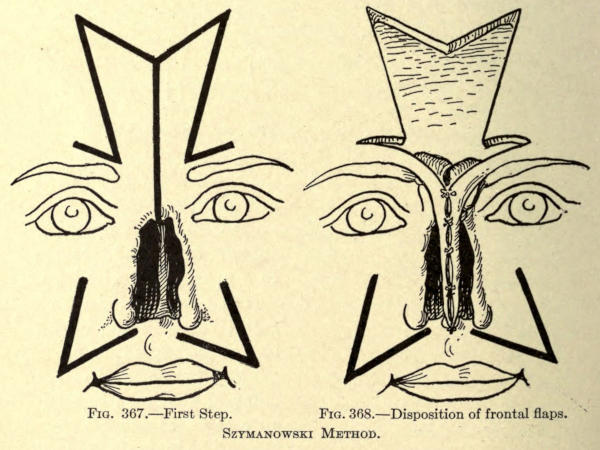
Fig. 367.—First Step.
Fig. 368.—Disposition of frontal flaps.
Szymanowski Method.
Goris Method.—The operation is performed as follows, having given very good results, according to the author:
I. The frontal flap is divided lengthwise so that its raw surfaces face each other. The resulting fold, representing the bridge of the nose, is held in place by catgut suture.
II. The skin to make the wings of the nose is folded in, as in the Langenbeck method.
III. A flap, half the thickness of the upper lip is brought up to form the new subseptum.
IV. Dissection and turning down the triangular flap of skin which surmounts the orifices of the old nose, and making it serve to line the lower part of the frontal flap.
V. Suturing the frontal flap thus modeled into two grooves made into the margins of the old nose along both sides to its base.
It soon became evident to the rhinoplastic surgeon that without some support to the flap or flaps used for[388] the construction of the new nose all of the preceding methods, as far as æsthetic results were concerned, were useless. Truly, the deformity lost its hideous appearance to a great extent, but the general results obtained hardly warranted a patient to undergo restorative operations of the nose. In fact, many surgeons advised against total rhinoplasty when practically all of the old nose was lost.
Langenbeck says “that total rhinoplasty, or even operation as to repair partial loss of the nose by the use of soft flaps, should not be undertaken. It is better to rely upon some prothesis.”
All that could be expected of utilizing the flap and making it heal into place had been accomplished up to about the year 1879. Thereafter many surgeons proceeded to evolve and use some kind of intranasal prothesis made of various inorganic materials. It may be stated, however, that Rousset in 1828 wrote: “Perhaps some day surgeons will give whatever shape they desire to the reconstructed nose. Then a frame of gold or silver, cleverly shaped and solidly fixed in the nose, will give the patient, at his own option, a Roman or Carthaginian nose, and to the ladies a choice of a roguish type, and to our Sultans a nose a la Roxelane.”
But it was after 1878 that such prothesis came into use, and these were at first made so that they might be removed at night and be replaced in the morning.
The intranasal supports were made of all kinds of material, such as gutta percha, gold plates, leaden devices, amber, silver, porcelain, celluloid, aluminum, platinum, etc.
With all due respect to the ingenuity of these inventions, especially that of Martin, which was made of platinum in the form of a St. Andrew’s cross, having at the four ends sharp pins which were driven and fixed into the skeleton of the nose, the use of these protheses resulted in nothing but failure.
The movable devices were a source of irritation and pressure, and could not overcome the consequent contraction of the flaps whether placed below a single flap or between two flaps, and the fixed protheses of whatever form or material caused so much pressure that gangrene resulted, and they had to be removed sooner or later.
Before the discovery of Gersuny, the author had many occasions to utilize such movable protheses in the correction of saddle noses. These were generally made of a silver shell, gutta percha, and later of decalcified bone, as advised by Senn. The former remained in place from six months to two and a half years, and then were thrown off or had to be removed because of irritation. The bone chips soon became absorbed, leaving the nose as before, or a thin median strip that became broken with the least violence, and then was absorbed.
In several cases where other surgeons had resorted to such protheses, the author was called upon at a later period to remove them.
While the immediate result is very gratifying, the ultimate result is worse than useless, since in the elimination of the foreign body the flap of the nose was married by cicatrices that added still further to the contraction and falling-in of the nose.
Some other method had to be devised, and organic supports became known. These organic protheses were made of the tissue in the near vicinity of the flap, and at first formed a part thereof. The earlier method included only the periosteum; later bone and periosteum were added to the flap to give it shape and support, and lastly cartilage was employed for the purpose.
Of the methods employing only the periosteum, it may[390] be said that what the surgeon expected of this membrane—namely, the springing up of bone cells—did not take place; at least, not to the extent desired. The very best to be attained was a thickening of flap in the membrane, but not sufficient to add necessary support to the nose.
The inclusion of the periosteum-lined flap was soon abandoned, and recourse was had to such bone additions to the flaps as could be obtained from the vicinity of the nose.
The bone was removed with its periosteum, adherent or nonadherent to the flap, as will be shown by the methods described hereafter.
Both single and combined flap methods are employed as might be expected, following the procedures of the Indian, French, or Italian schools. The greatest credit for the methods herein involved belongs to the surgeons of Germany.
The earliest operation on these lines was that of König, who published his first successes in 1886.
König Method.—Extending upward from the root of the old nose, a flap is outlined in vertical ending at the hair line of the scalp, as shown in Fig. 369.
This flap was made about one centimeter wide, and is made to include the skin and periosteum. With the chisel a thin strip of bone is raised from the frontal bone to nearly the full length and width of the flap, making it an osteoperiostitic cutaneous section attached by its pedicle at the root of the nose.
This flap is brought down with bony surface outward, and the distal or skin end is fixed by suture into the upper lip at the point of the intersection of the subseptum.
Any of the soft parts of the old nose remaining are now dissected up toward the median line, and are folded[391] upward and inward and sutured by their freshened margins to this median flap.
An Indian flap in oblique direction and of the form shown is cut from the skin of the forehead and rotated down into position before the bone-lined flap, and sutured into place.
He advises not to include the periosteum in the flap making up the subseptum, as it is likely to interfere with respiration. In fact, he deems it best to make the tegumentary flap sufficiently long to build the bone of the nose, doubling the raw edges upon themselves with a celluloid tube apparatus that may be removed for cleansing, and be kept in place long enough to give contour to the nares.
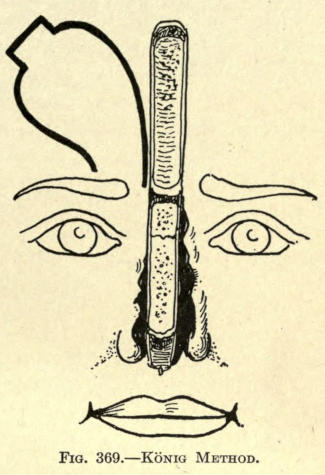
Fig. 369.—König Method.
Von Hacker Method.—The frontal flap was cut in the ordinary Indian method, and of the shape shown in Fig. 355. The skin at either side of the median line was dissected up to within four millimeters, leaving a strip eight millimeters wide from the root of the nose to the distal or scalp end. The two loose lips of the flap were brought together at the anterior median line by a few sutures to keep them in place.
This was done to give freedom to the surgeon while he detached a strip made of the periosteum and bone chiseled from the frontal bone. At the root of the nose or below the pedicle the bone was not included to the extent that it would interfere with torsion of the flap, and yet sufficient to allow the raw bone surface to fall upon what remained of the bony bridge of the old nose.
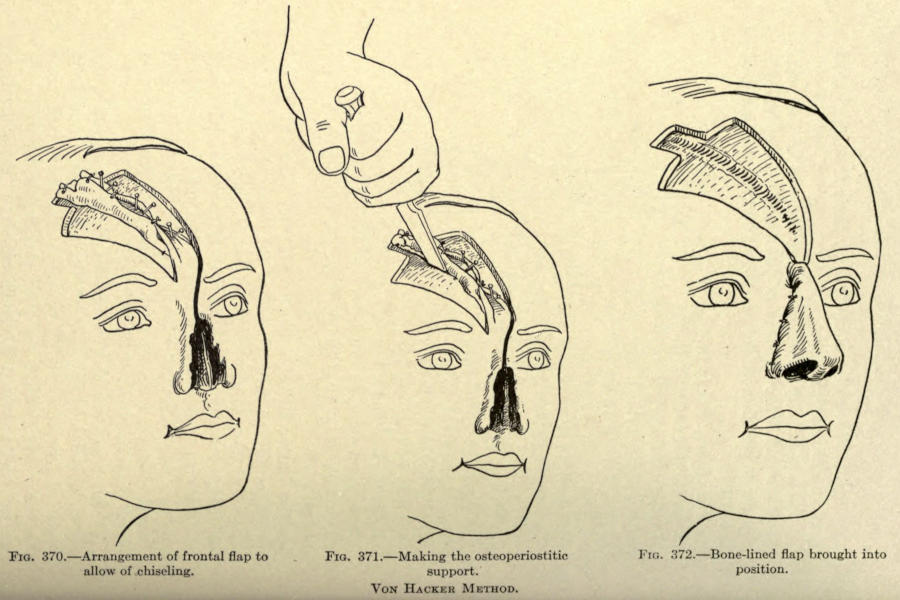
Fig. 370.—Arrangement of frontal flap to allow of chiseling.
Fig. 371.—Making the osteoperiostitic support.
Fig. 372.—Bone-lined flap brought into position.
Von Hacker Method.
He utilizes pins driven into the bone to outline this bony section, as shown in Fig. 370.
The latter is done in an oblique direction. See Fig. 371. The septal section is made to include the bone strip.
The bridge of bone holding the flap at its inferior end was now broken, leaving, however, the periosteum as part of the pedicle hinge.
The whole flap thus outlined was rotated downward into position and sutured, as shown in Fig. 372.
The margins at the base intended to form the subseptum were sutured behind the osseous structure, or, in other words, were doubled inward and fixed by suture. The bony strip was broken at the proper point to give prominence to the lobule.
The margins for the nostrils were turned inward and doubled on themselves, and sutured with silk.
Rubber tubes were left in the nares, for drainage and to keep them distended.
Rotter Method.—The frontal flap is made in the shape shown in Fig. 373, containing a section of the frontal bone and its periosteum. The width of the flap is about three and a half centimeters wide.
This flap is turned downward so that its raw surfaces look outward.
Owing to the loose adherence of the bony section to the skin flap, he allows the raw bone surface to granulate over for four weeks, to fix it more solidly to the soft parts.
The bone plate is then sawn into three sections made by two vertical incisions, made as shown in the illustration.
The median section forms the bridge and dorsal prominence of the nose.
The adherent skin of the lateral bony plates is dissected[394] up sufficiently to permit of the proper formation of the sides and wings of the nose.
This gives a shape to the nose, as shown in Fig. 374.
The lateral margins of the integumentary flap are now sutured to the freshened margins of the old nose, and the remaining skin, if any, is made to cover the granulating surface; if this is lacking or insufficient, skin grafts are utilized to cover it completely.
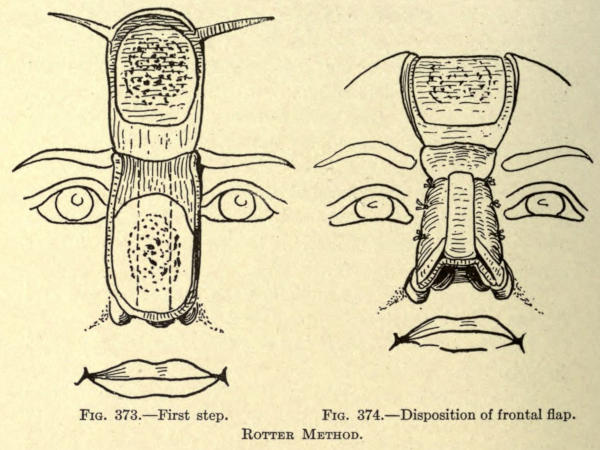
Fig. 373.—First step.
Fig. 374.—Disposition of frontal flap.
Rotter Method.
Schimmelbusch Method.—The principle herein is to give an osseous wall to the whole length of the restored nose, covering well the skin inside and outside, and, if possible, to fix the new nose solidly at the pyriform opening.
“I cut an osteo-cutaneous flap from the middle of the forehead, of a size proportional to the size and shape of the nose. Its pedicle between the eyebrows is two or three centimeters wide; it widens out superiorly to form seven to nine centimeters. It is triangular, and its base lies near the hair line. In cutting it out, preferably a little large, it goes at first to the bone, through skin and periosteum. With a large, sharp chisel, a thin bone plate throughout the whole extent of the cutaneous flap is detached.[396] It is not always possible to make this a plate in one piece; it often breaks or gives off splinters. This is of no consequence, if care be taken not to lose them and to keep them adherent to the periosteum. They are attached as well as possible to the cutaneoperiostitic flap by passing threads crosswise from one edge of the flap to the other over bony surface, as in Fig. 375. The whole flap is then enveloped in iodoformed suture.
“The frontal wound I close at the same sitting by sliding large lateral flaps whose upper border follows the margin of the hair as far as the ears. These are freed completely, brought down and stitched, leaving eventually only a linear cicatrix on the forehead. The lateral loss of substance which results is healed by granulation, and the scars concealed by the hair.
“At first parts of the bone die; they ought to be expected to fall out; after four, six, or eight weeks the bone is completely covered with fleshy granulation, and adheres solidly to the flap. The prominent granulations are then scratched, or, better, trimmed away with the knife, and the whole surface is covered with Thiersch grafts.
“When the flap is thus furnished with skin within and without, it is put into place. I saw the bony plate with a fine-toothed saw from the grafted side; then I model the flap and place it on the loss of substance freshened by turning the grafted surface toward the interior of the nose by twisting its pedicle, as in Fig. 376. The osseous rim of the pyriform opening is uncovered at the moment of this freshening, and the bony edges of the flap are placed exactly on the bony edge of the aperture. The skin of the flap is then stitched at its lower margins to the skin of the cheeks. To preserve the height of the nasal profile and avoid displacing the bones of the nose, the nose is kept in place with a pin thrust through the nose, and furnished at each end with a rubber button. This aids to form the wings of the nose. If a subseptum[397] is needed, it is made by taking from the skin that covers the circumference of the pyriform opening two small flaps, which are dissected from without toward the median line as far as the point where the septum is normally found.
“These are stitched at this point, first upon themselves, then to the end of the nose. Three weeks later the pedicle of the frontal flap is cut; it is turned, put in splints, and the stitching is finished.”
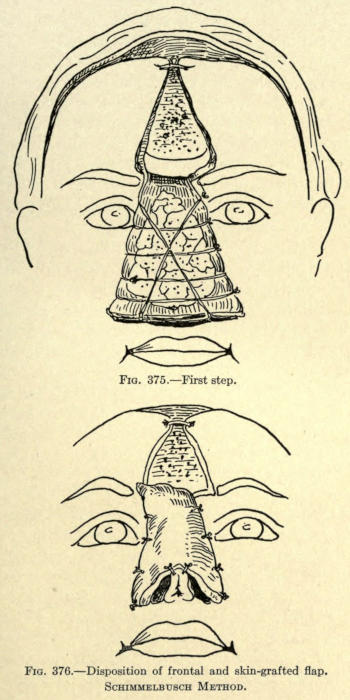
Fig. 375.—First step.
Fig. 376.—Disposition of frontal and skin-grafted flap.
Schimmelbusch Method.
Helferich Method.—A lining flap is made, according to the French method, from the one cheek, which is dissected up and turned over to bridge most of the loss of nasal tissue, and sutured to the opposite freshened margin, as showed in Fig. 377.
A frontal flap, as outlined in the same illustration, is now cut from the forehead, leaving a pedicle as shown, and containing a section of bone at its median line. This is rotated downward and into place, and sutured along the same margin to which the genian flap is fixed, as shown in Fig. 378.
When the frontal and genian flaps have become well united, the latter’s pedicle is cut when the freshened lateral margin of the frontal flap is sutured into place.
A subseptum is now made or deemed necessary by this surgeon.
At a later period the pedicle of the frontal flap is cut, and fixed by suture and some cutting, to reduce the resultant prominence thereof.
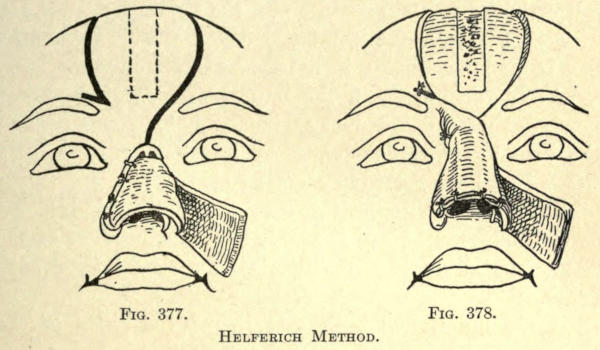
Fig. 377. Fig. 378.
Helferich Method.
Preidesberger Method.—This author cuts away the skin surrounding the arch of the old nose, and turns this flap downward to form the lining to the flap made from the forehead made in the same manner as Helferich.
The bone section is made in the median line, and is one centimeter wide and four long.
The frontal flap should be made long enough to permit of building a subseptum and the nostrils.
Krause Method.—This frontal cutaneo-osteo-periostitic flap is made according to the method of König.
After turning down the flap it was covered with a nonpedunculated skin flap taken from the upper part of the arm by transplanting after its subcutaneous fatty tissue had been removed. (See Fig. 379.)
This method necessitates a long-continued dressing of the forehead before the pedicle is cut, because of the needed nutrition to make the two flaps heal upon each other.
After union has been established the sides of the transplanted flaps are raised by dissection, as shown in Fig. 380, to expose the bone plate of the frontal flap. A median strip is left intact.
With a fine saw the bony plate is cut into three sections, making the narrowest the median.
The margins of the old nose are now freshened, and the combined flap is sutured along the sides, preserving what tissue the surgeon can use to add support to the nose, which is done by dissection and turning or folding, as heretofore described.
The lower or forehead flap is sutured to the soft parts of the old nose, and the transplanted lateral margins to[399] the marginal skin of the cheeks, giving to the nose the appearance as shown in Fig. 381.
At a later period the pedicle is cut and the wound that cannot, at this time, be overcome by sliding of the adjacent skin, is covered by skin grafting.
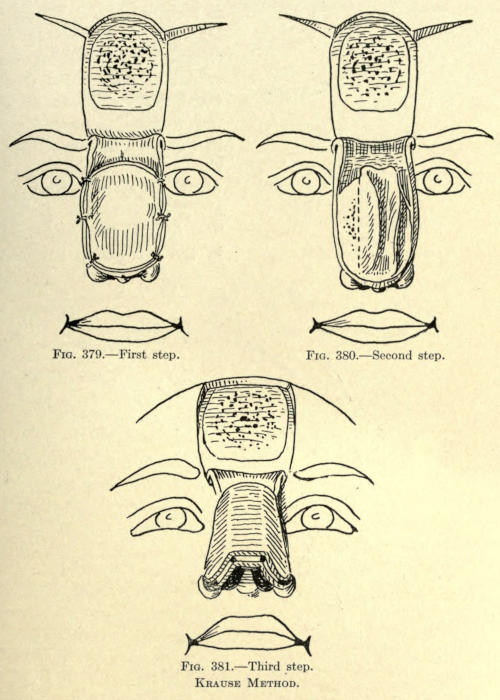
Fig. 379.—First step.
Fig. 380.—Second step.
Fig. 381.—Third step.
Krause Method.
Nélaton Method.—A lateral flap of skin is taken from the cheeks, beginning on a line with the root of the nose and as low as a point two thirds of its normal length. These flaps are made wide enough, so that when dissected up and folded inward they will meet on the median line, as shown in Fig. 382, having their raw surface facing outward. They are sutured along the median line. The frontal flap was cut in the form of a horse-shoe having its pedicle at the root of the nose just above the eyebrows, and being about three centimeters wide and six long.
The skin at the outer margins was dissected up from the bone, leaving sufficient attachment at its center to allow for a bony plate.
With a fine saw, and in the manner shown in Fig. 383, this plate was made from the frontal bone, being about two and a half centimeters wide and four long.
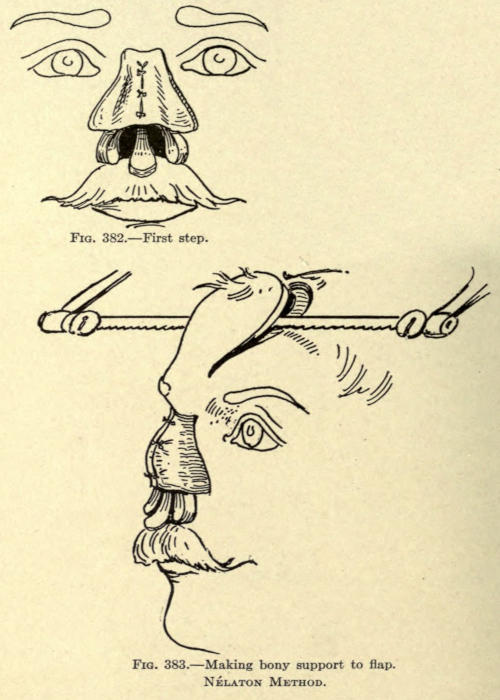
Fig. 382.—First step.
Fig. 383.—Making bony support to flap.
Nélaton Method.
There is some difficulty associated with the making of the flap, which ends at the superior border of the frontal, leaving the pedicle composed only of skin.
The flap is now turned down, exposing its raw surface. The[402] bony plate is sawed through at the median line, as shown in Fig. 384, and the skin of the flap is also divided along this line, giving two partly bone-lined flaps.
The two flaps are now rotated downward before the lost nose, so that their raw surfaces face inward, and in this position they are sutured along the median line and the sides, as shown in Fig. 385.
The method gives an angular dorsum of satisfactory consistency to the new nose, but furnishes a serious drawback, in that the cicatrization along the median line is liable to affect the shape of the organ and leaves a prominent scar line. The use of two small pedicles is another objection in that the danger of gangrene is greater as the nourishment to each flap is less.
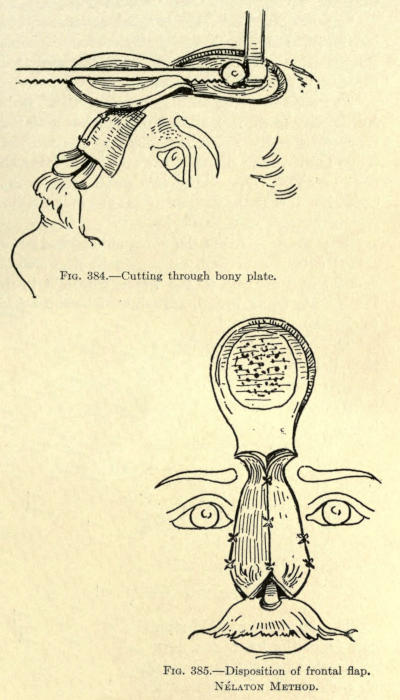
Fig. 384.—Cutting through bony plate.
Fig. 385.—Disposition of frontal flap.
Nélaton Method.
Israel Method.—From the ulnar side of the left forearm Israel cuts a skin flap, as shown in Fig. 386, with its smaller end nearest to the wrist, where it is detached, the pedicle being broad, assuring of better nourishment to the flap.
The narrow end of the flap is cut down to the bone, then the sides are dissected up until the borders of the ulna are reached on both sides, reserving an adherent strip about eight millimeters wide and six centimeters long.
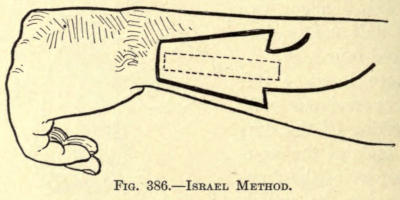
Fig. 386.—Israel Method.
The bone below this strip is now removed with the saw from the lower end upward, and ending about one centimeter beyond the base line of the flap, where the strip so made is left connected to the bone proper.
The flap is now raised gently and bent upward without breaking the bone. It is sawed half through, transversely, at a point corresponding to the lobule of the nose.
The flap is then enveloped in iodoform gauze, and the head, forearm, and arm are fixed in plaster of Paris, the forearm being bent at a right angle to the arm (see Fig. 387).
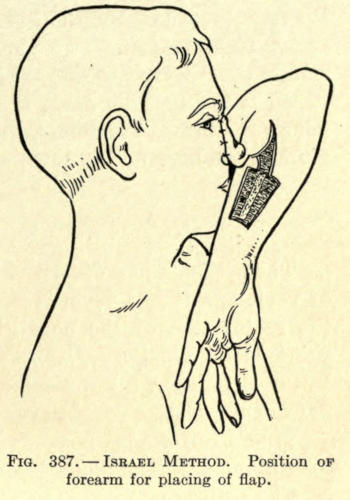
Fig. 387.—Israel Method. Position of forearm for placing of flap.
After nine days the osseous connection still remaining is severed, and the nose is modeled upon the forearm, as heretofore described in these operations, this surgeon using silver wire to retain the parts. The raw skin surfaces are allowed to heal upon each other and the flap is permitted to come in contact with the wound on the forearm temporarily, to which it might adhere, the gauze being now removed.
After twelve days the newly modeled nose is freed from such adhesions and kept from healing to the parts by using dressings between the flap and wound.
Five days after, the margins of the old nose are freshened in the form of an inverted V. If there be sufficient cicatricial tissue it is turned down, raw surface out, to line the new nose.
A prolongation of the pedicle is now cut, widening out toward the radial side of the arm, made obliquely, as shown, so that its pedicle now corresponds to a width of seven centimeters.
The whole flap except this newly formed pedicle is cut free of this forearm. The arm is put into the position shown in Fig. 387, and the freshened flap margins at the root, the whole length of the left side, and part of the upper right lateral. The plaster dressing to hold the arm in the proper position until complete union is established is used. This done, the pedicle is cut, and such minor operations are done to fix the remaining free margin and the base of the new nose.
The methods just described in which an osseous plate of various size and form is included with skin flaps for the restoration of the nose give undoubtedly the best rhinoplastic results. The new nose is given not only better shape, but a permanency of such form that skin flaps of themselves could never give.
The unfortunate factors in these osteo-cutaneous operations are the many difficulties experienced.
The cutting or making of the bony plate is no simple task.
The skin is an uncertain agent to employ, because of the peculiar contour of the bony surface from which the plate is to be removed. The chisel, no matter how dexterously used, is liable to cut through the entire bone thickness, which has occurred in several recorded cases.
There is also the possibility of necrosis of a part or all of the bony plate thus obtained, and where the latter is not lined interiorly there is the added danger of infection.
Furthermore, the secondary wound is more extensive; the bone exposed requires about a month’s time to granulate over before skin grafts can be successfully applied over it.
With the employment of a cheek-flap lining there is[405] the added objection of cicatrization. The use of a flap from the arm is complicated and requires considerable time for the completion of the operation, and there is always the added danger of infection and consequent death of the osseous plate.
To overcome these many difficulties von Mangold advocates the use of a section of cartilage to support the anterior prominence of the nose.
It has been found, since the first attempt of and the successful result obtained in 1897 by this surgeon, that cartilage to be used for this purpose should be taken from the costal cartilage, where a strip of the required length and width can be obtained.
The results thus far recorded are excellent, and much is hoped for from this method, especially in the reconstruction of loss about the wing of the nose in partial rhinoplasties, where the convexed contour may be reproduced to a nicety.
The first attempt to support the flap for a total rhinoplasty by this method was made in 1902 by Charles Nélaton.
The use of cartilaginous supports may be combined with any of the methods given heretofore. The flap containing the cartilage may be lined or unlined. All tissue found about the old nose should, of course, be utilized to give added support and to reduce as far as possible extensive secondary cicatrization.
The combined Hindu and Italian methods give splendid results, the frontal flap and its support being brought down from the forehead, raw surface outward, and the arm or forearm flap being placed immediately in front of it.
The frontal flap with the support requires a preliminary operation to permit of the attachment of the cartilage. Fortunately, this step requires but little time and shows a very slight disfigurement during this period.
The secondary wound at the site of the cartilage excision[406] requires little attention and heals readily, and the cicatrix involved is very small.
Steinthal proposes taking the flap and cartilage from the thoracic region, grafting it during the preparatory period to the forearm, from which it is transplanted to the face at a second sitting.
There is the objection to this method that it requires the arm to be retained in position for a very long time.
The author advocated the use of an arm flap made by the Italian method to line the one to be brought down from the forehead in cases of total rhinoplasty where little or no tissue can be obtained from the remains of the old nose. Such procedure reduces the time required by the Steinthal method to one half, and therefore greatly lessens the discomfort to the patient.
The fundamental principles as laid down by Nélaton are excellent, and may be applied to any modification of method the surgeon may decide upon where a section of costal cartilage is employed to support the flap, whether this be taken from the forehead, other parts of the face, or remote places.
The procedure of Nélaton is as follows:
Nélaton Method.—The method involved a preparatory and a final operation.
The preparatory operation has to do with obtaining and placing in position the section of cartilage under the skin flap wherever located.
The final operation may or may not consist of two sittings, the first being necessitated by the bringing upon the remains of the nose a flap of skin to line the one brought down in front of it and containing the support.
Preparatory Operation.—To begin properly, the frontal flap to be utilized is marked out on the forehead with nitrate of silver the day before the operation, so that its outline will be plainly discernible, and act as a guide for the placing of the cartilage. The shape of the flap is fashioned as shown in Fig. 388.
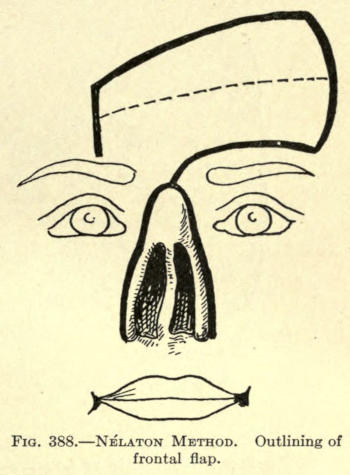
Fig. 388.—Nélaton Method. Outlining of frontal flap.
In the illustration is also shown the incisions later made to utilize the borders of the remaining nose to line the frontal flap. This is done by making an inverted V incision at a distance from the inner borders, corresponding to the lateral line of union of the frontal flap with the face. The resultant flap is turned down, raw surface outward, curtainlike, and is sutured to the frontal flap, where it falls into position.
The flap outline shows that its pedicle lies between the outer end of the inner third and above the right eyebrow and a little to the left of the median line at the root of the old nose. This will avoid considerable tension at this point, the rotation as made being ninety degrees.
Nearly horizontally, as shown in the figure, a line is drawn through the center of the flap, showing the position the strip of cartilage is to occupy.
This done, a pattern of the outline is cut from stiff paper or oiled silk to preserve as a guide for the making of the flap, it being understood that the outlining has been made to the measurement of the required nose, allowance being given for cicatricial contraction.
This done, the surgeon having prepared the skin about the costal prominences of the left thorax, he proceeds as follows:
A vertical line is drawn the width of two fingers to the[408] right of the nipple, as shown in Fig. 389, the length of the line being obvious.
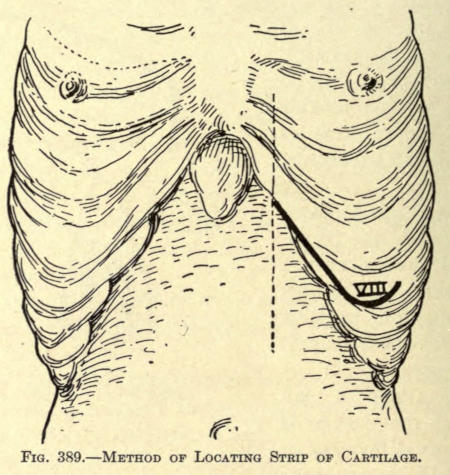
Fig. 389.—Method of Locating Strip of Cartilage.
Where the vertical crosses the eighth costal cartilage an incision is made downward over and not under the border of the cartilage.
The incision extends downward for a distance of eight centimeters, where it is turned upward at an angle, as shown, to a distance of three centimeters.
By separating the muscular aponeurosis made visible by this incision the lower edge of the eighth costal cartilage is exposed. The knife is moved along the lower edge of the cartilage, dividing the fibers of the insertion of the transverse muscle from without inward. The cartilage can now be grasped between the thumb and forefinger and be forced out of its normal position after a slight anterior dissection.
The union between cartilage and bone is exposed. The chisel is used to divide the cartilage about one centimeter[409] from the rib, after the costal or inner extremity has been made.
The position of the hands and the exposed cartilage is shown in Fig. 390.
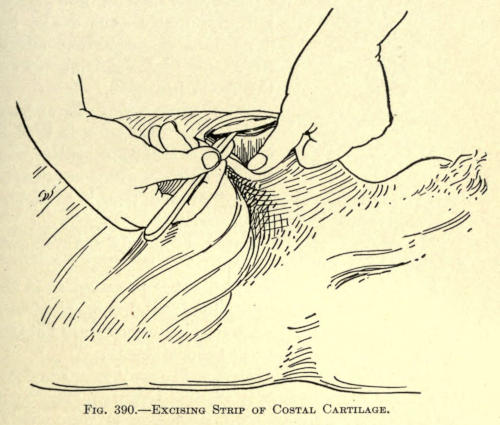
Fig. 390.—Excising Strip of Costal Cartilage.
This accomplished, the wound is temporarily dressed. The cartilage is then fashioned to suit the required size and shape.
It is thinned down on its lower surface to about three millimeters in diameter. This thickness is maintained to a length of two and a half centimeters, the part being intended for the subseptum.
A notch is made on the upper surface at this distance from the end, which marks the point at which it must be eventually bent to form the point of the nose. This notch is cut to two thirds of the entire thickness.
The required length, that of the nasal line and its added septal length, is preserved.
The cartilage being prepared is now ready for the insertion under the frontal periosteum at the site already marked.
For this purpose a vertical incision one and a half centimeters, extending down to the bone, is made, as shown in Fig. 391.

Fig. 391.—Cartilage Placed under Frontal Flap.
The periosteum is peeled away from the bone with the dull or rounded handle of a knife.
The cartilage is now thrust into the tunnel thus made, the thinned-down, notched-off section facing forward and lying toward the vertical incision.
The skin wound is sutured and a gentle compress is used to keep the cartilage in contact with the periosteum, which requires at least two months. A longer interval of time is advocated to give greater vitality to the cartilage.
The wound of the thorax is simply sutured and dressed as any surgical wound.
Final Operation.—The part cut is prepared as in the Hindu method. A lining for the frontal is made of such tissue as remains, and its freshened borders are sutured where possible, as shown in the last figure.
When this cannot be done, a flap may be taken from the arm, as already suggested, or a Krause nonpedunculated skin flap may be used, according to the methods given heretofore.
The epidermis is made to face inward. If either of these methods is used, the frontal lap is not brought down until healthy granulation has been established.
The frontal flap is made to include the periosteum, from which it is separated with a blunt instrument. The cartilaginous strip will be found to be attached to the periosteum.
The freed flap is now brought before the nasal defect and fitted into place. The cartilaginous strip should occupy the anterior median line.
The subseptal cartilage is bent inward and downward and the skin of the flap is sutured to it with catgut to form the subseptum, as shown in Fig. 392.
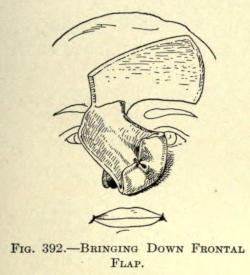
Fig. 392.—Bringing Down Frontal Flap.
The free margins of skin remaining at the septal bone of the flap are folded inward to line the new nostrils. Catgut sutures are used to keep these folds in position.
The nose is now ready to be sutured into place. The subseptum is inserted first and fixed into the upper lip, then the nose being held so that its median line occupies the proper position, both wings are sutured to the freshened margins, and lastly the sides (see Fig. 393).
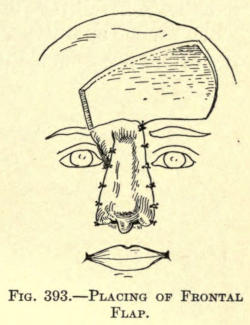
Fig. 393.—Placing of Frontal Flap.
The frontal wound may be drawn together as near as possible by suture.
Rubber drainage-tubes are kept in the nares for a few days, and are thereafter replaced by rolls of gauze.
Dry dressings are preferred for the nasal wounds, which heal in about five days.
A month after, Thiersch grafts are employed to cover the frontal wound remaining. They require about eight days to heal into place.
In this defect there may be a loss of the lobule and both alæ, including the subseptum, or there may be a lateral loss, involving more or less of the base.
There are many types of this deformity, so that to include all would involve considerable space, and at best most of the operations involved would be those utilizing the methods heretofore mentioned.
The earlier operations for the correction of lesions of large extent are founded upon the use of skin flaps, which have been shown to be unsatisfactory because of their consequent cicatrization. Reference is made, however, to several of these to exhibit the disposition of the remaining parts of the old nose.
Later will be considered the methods involving osteo-cartilaginous supports.
Steinhausen Method.—The inferior remains of the old nose are detached from the margins and brought downward; a Hindu flap is fashioned as shown in Fig. 394, and brought down to form the new nose; the size of the flap is given as being four inches wide and eight inches long.
The distal end of the flap is sutured to the freed flaps obtained from the borders, as shown in Fig. 395.
The method is purely of the Hindu type, and the results are not, therefore, very satisfactory.
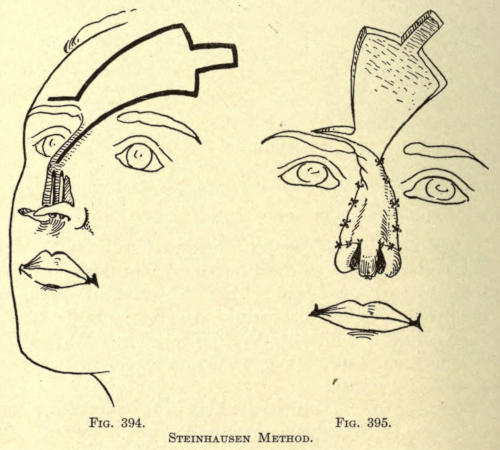
Fig. 394. Fig. 395.
Steinhausen Method.
Neumann Method.—This author cuts down the remains of both lower margins of the old nose, as in the Steinhausen operation. A wedge-shaped section is cut from the entire thickness of the upper lid and turned upward to form the subseptum, and is sutured to the[414] lateral parts brought down by the former incisions, to which it is sutured at the median line, as shown in Fig. 396.
Two lateral flaps are now made from the sides of the remaining nose retaining their cartilages, as shown in the illustration, A, B, C, D, showing one of them. The two flaps remain attached, anteriorly along the median line over the bridge of the nose. These two lateral flaps A, B, C, are turned down from the point A, which represents the pedicle, and are sutured at the median line by their lower borders, A, B, the borders B, C, being thus brought down, fall before the fresh borders taken from the margins of the old nose, to which they are sutured, as shown in Fig. 397.
This procedure will leave two exposed areas at either side of the nose, which are permitted to heal by granulation.
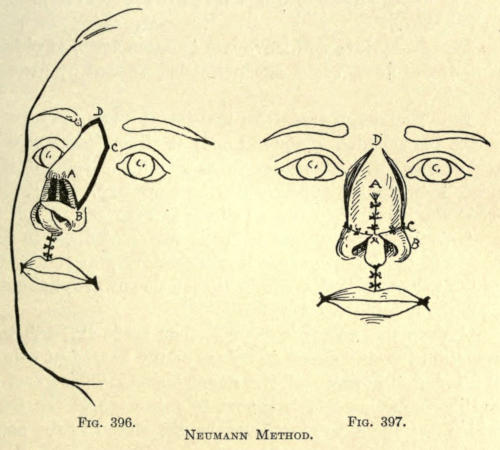
Fig. 396. Fig. 397.
Neumann Method.
Later Neumann Method.—An incision is made to circumscribe the remains of the old nose at either side, extending upward in rectangular form above the root of the nose, between the inner canthi and upward, and somewhat above the eyebrows, as shown in Fig. 398.
This flap thus outlined is freely dissected down to the bones of the nose, leaving it attached only at the roots of the wings, so that it can be turned downward, hanging over the mouth, like a curtain.
A deep transverse incision is then made through the remaining cartilaginous structure of the nose, just below the inferior borders of the nasal bones. This gives a cartilaginous, archlike support to this part of the flap, which is utilized to give firmness and shape to the base of the new nose.
The incision just mentioned is depicted in Fig. 399, in which is also shown the turned-down flap.
After the hemorrhage has been controlled the flap is turned upward and into such position as to form the new nose, utilizing the cartilaginous arch, above referred to,[415] to the best advantage to give the proper contour. This will lower the apex of the flap considerably. The lateral borders are sutured to the freshened margins where possible, but as a rule an opening is left at either side, communicating with the inner nose, which must be healed by granulation.
The wound on the forehead may be brought together completely by suture. The appearance of the nose assumes at this time the form shown in Fig. 400.
The objection to this method lies in the fact that the cartilaginous arch brought down with the flap is usually insufficient to give proper support to the base of the nose, permitting the lobule to contract and sink. In most cases there is an absence of sufficient cartilage to employ the method at all. An osseous arch would, therefore, preferably be incorporated with the flap, taken from the remaining nasal bones.
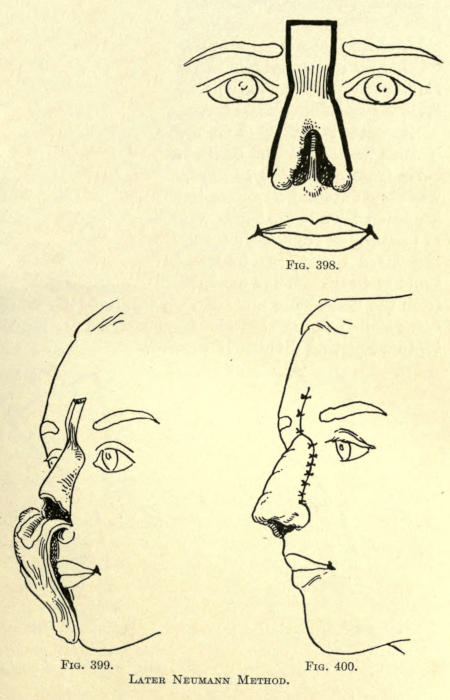
Fig. 398. Fig. 399. Fig. 400.
Later Neumann Method.
Bardenheuer Method.—This author makes a transverse incision across the root of the nose, and two lateral incisions from either end of the first, carrying them downward and outward, as shown in Fig. 401. These incisions are made down to the bone. With a chisel the nasal bones are separated from their frontal and superior maxillary attachments, giving an arch of bone to the flap, which is brought downward and outward, the bone being dissected from the underlying mucosa. To facilitate the bringing down of this flap the anterior border of the cartilaginous septum must be divided if present.
The flap thus made is attached only at the two points of skin at the inferior borders, the epidermal surface[417] looking inward. The archlike mass of bone is gently bent backward at either side to practically reverse its convexity. The position of the flap is shown in Fig. 402.
The raw surface of the flap above mentioned is now covered with a flap taken from the forehead in the form shown in the figures.
The resultant nose is entirely lined with skin, and contains sufficient bone to support it. The objection is that there must necessarily be a large secondary wound in the forehead, which must be covered with Thiersch grafts.
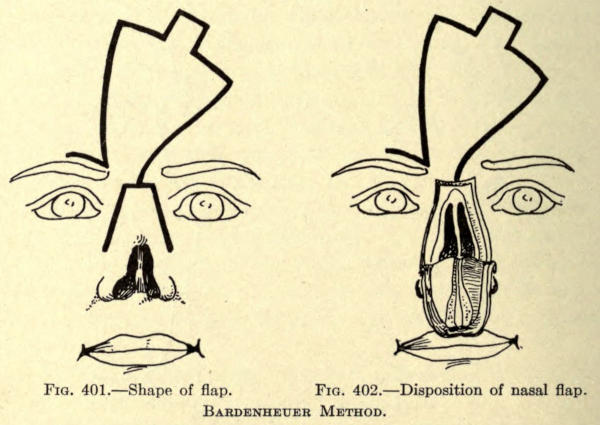
Fig. 401.—Shape of flap.
Fig. 402.—Disposition of nasal flap.
Bardenheuer Method.
Ollier Method.—This author uses an inverted V incision, beginning on the forehead at a point about three centimeters above the superior margin of the eyebrows. The diverging incisions are carried down to a point just above the base of what remains of the old nose, where it remains attached.
The shape of the flap thus made is shown in Fig. 403.
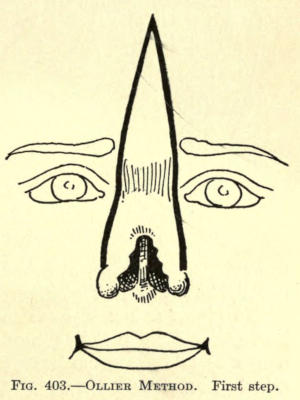
Fig. 403.—Ollier Method. First Step.
The flap is dissected up and made to contain the periosteum as far as the juncture of the frontal nasal bones.
The skin over the right nasal bone is now dissected up, without, however, including the periosteum. The left nasal bone, still adherent to the skin, is removed with the chisel, beginning at the median line, then at its frontal attachment, and lastly along its union with the superior maxillary bone.
On the right side what remained of the cartilaginous structure was divided so as to include it in the flap.
This gave a large triangular flap, periosteo-cutaneous above, osteo-cutaneous below that, and ending in a chondro-cutaneous border, attached to the face by a double pedicle, as shown in Fig. 404.
To give further support to this flap at the median line, Ollier divided the septum with the scissors in such a way as to form an antero-posterior cartilaginous flap attached by its lower base.
The flap was brought downward in the same manner as in the method of Neumann and sutured into position, the parts involved assuming the position shown in Fig. 405, in which the lateral nasal surface is left uncovered to show the space occasioned by the removal of the nasal[419] bone, and in dotted line the position that bone now occupies.
In five weeks the two nasal bones united, end to end, and three months after the operation the space made by the removal of the bone had become filled with hard tissue, that eventually ossified in about seven months.
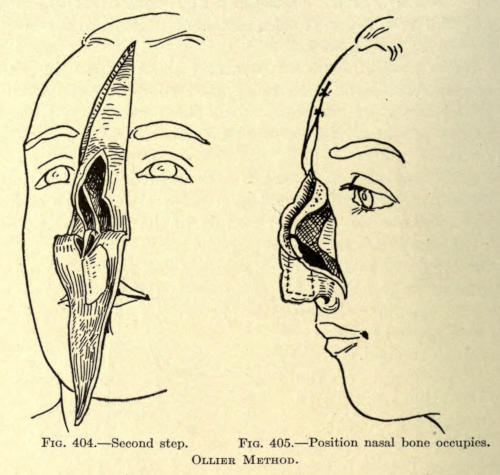
Fig. 404.—Second step.
Fig. 405.—Position nasal bone occupies.
Ollier Method.
Langenbeck Method.—A median incision is made through the remaining skin of the old nose, dividing it into halves. The incisions about the base and the shape of flap to be brought down from the forehead are shown in Fig. 406.
The skin over the nose is dissected up, moving toward the cheek, exposing the bony frame of the nose.
From the lower border of the pyriform aperture two elongated triangular plates of bone are made, being[420] attached posteriorly to superior maxillary bones. They should be made about one sixth inch wide.
By their subsequent displacement they are made to lie antero-posteriorly. With a saw the nasal bones are separated from their maxillary connection from below upward, making a median bone plate, which is raised with a levator to the height desired for the new nasal bridge, remaining attached to the frontal bone, as shown in Fig. 407.
A frontal flap is taken from the forehead and sutured to the freshened raw margins of the lateral flaps.
The bone plates are fastened to each side of the frontal flap by suture.
The nasal base is preferably made of the tissue remaining of the old nose, as depicted, to prevent closure of the nostrils, the only difficulty being to keep the poorly nourished tissue from dying. When used the raw surface is brought in contact with that of the frontal flap.
The objection in this case is that the median third anterior line usually falls in rapidly, leaving the nose dished or saddled, and unless there be sufficient tissue to construct the base, the objections so often referred to heretofore will occur.
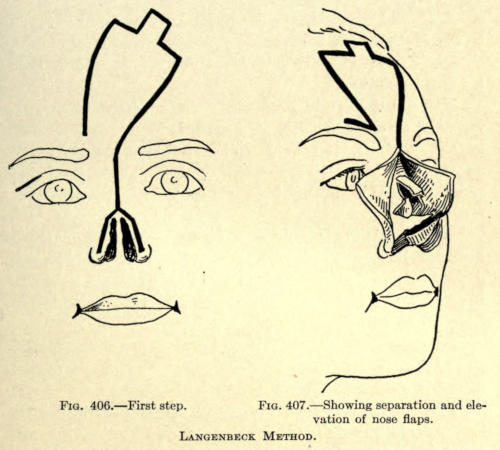
Fig. 406.—First step.
Fig. 407.—Showing separation and elevation of nose flaps.
Langenbeck Method.
Ch. Nélaton Method.—This author uses an osteo-cutaneous flap taken from the forehead. The shape of the latter is shown in Fig. 408.
The lateral incisions are to be made the width of a finger from the margins of the old nose, extending upward in curved fashion through the inner edge of the eyebrows and meeting at a point on the forehead, becoming slightly oblique near the border of the hair.
The flap is dissected up from the borders inward, including the periosteum, leaving a strip of bony attachment at the median line.
The dissected sides of the flap are held up by an assistant while the operator proceeds to chisel a thin bony[421] plate from the frontal. The bony plate ends just above the root of the nose.
The dissection is now carried on downward until the bones proper of the nose appear, and latterly, so that the saw does not injure the soft parts, and to act as a guide for the course of the latter.
The position of the flap and the saw in position is shown in Fig. 409.
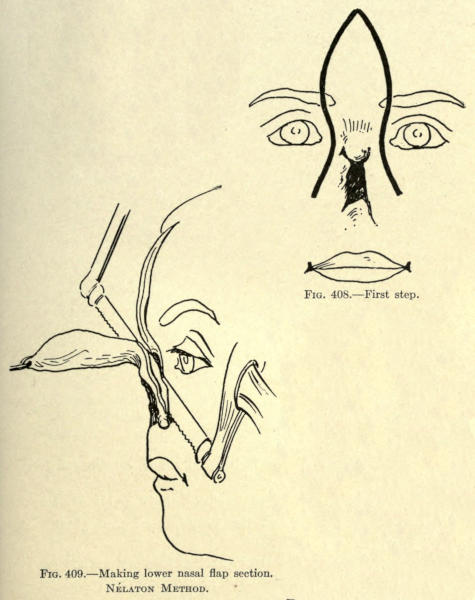
Fig. 408.—First step.
Fig. 409.—Making lower nasal flap section.
Nélaton Method.
The saw is made to sever the nasal bones from the apophyses of the superior maxillary. The blade follows a line starting one centimeter anterior to the anterior and superior nasal spine, and is directed downward toward the second molar, not going entirely through the apophyses.
The latter are broken with the chisel in such way that some of the bony border lies in contact with the nasal process of the superior maxillary.
This fracturing is made as the flap is still further brought down, as in Fig. 410.
The flap is now so adjusted that its median bone-lined section will form the median third of the nose, the base being made by folding the flap upon itself, as shown in Fig. 411.
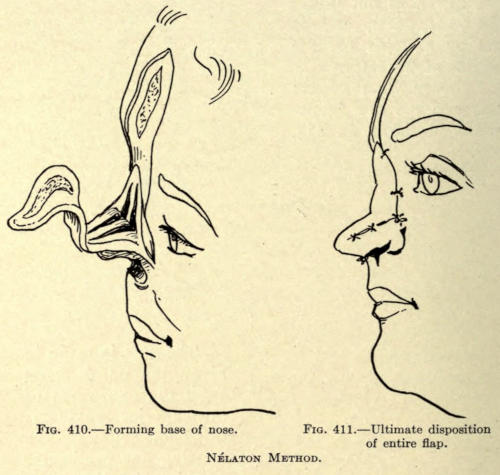
Fig. 410.—Forming base of nose.
Fig. 411.—Ultimate disposition of entire flap.
Nélaton Method.
The raw surfaces are sutured at their point of coaptation, laterally, and to the margins of the genian flaps.
The frontal wound is brought together by suture as closely as possible, and Thiersch grafts are employed to close any wound still remaining.
The objections to this operation is that of all bone-plate flaps. A flap containing a cartilaginous support[423] taken from the eighth costal cartilage, as previously described, would undoubtedly give the best results.
The defect being at a distance from the forehead, the employment of frontal flaps for the restoration of the lobule and alæ are to be eliminated; furthermore, such methods would involve the incision and dissection of the healthy skin of the nose to no advantage but disfigurement, and possible further loss of the organ.
The results with autoplasties about this part of the nose are usually excellent, and particularly gratifying are those obtained with the Italian method, in which the flap is made from the skin of the forearm.
French methods involving large nasogenian flaps are not to be used because of their consequent retraction and cicatrization of the cheeks. Small lining nasogenian flaps may be utilized where necessary, since they cause little scarring.
If the loss of tissue is very small, the flaps to reform the parts may be taken from the nasal skin and the septum be made of a flap from the upper lip. Both such secondary wounds could be drawn together by suture, leaving slight linear scars. Operations of this nature will be described separately later. Some of the methods referred to might be combined for small defects of this nature.
Defects of larger extent may be corrected as follows:
Küster Method.—A flap of considerable size is outlined on the skin of the arm and cut laterally, leaving it attached at both ends in bridge fashion.
Gauze dressings are inserted under the flap. Several days later the superior pedicle is severed and the flap is sutured to the freshened margin of the nose. An application of borated vaselin on gauze is used as the dressing.[424] The arm is held in position by a proper apparatus, a plaster-of-Paris fixture being used by the author.
Six days later the brachial plexus is divided to half its width, and totally divided three days thereafter.
Fifteen days later the free border of the flap is divided into three sections, the median one being made narrowest. The outer small flaps thus made are sutured to the remaining wings of the nose.
Five days later the septum is formed of the remaining unattached flap, which is sutured to the stump of the old septum. It is not folded upon itself, but allowed to heal by cicatrization.
Eight days later minor operations are performed to reduce the exuberant portions of the side flaps.
Berger Method.—This author makes a flap of the skin above the border of the nose, which he turns down, raw surface outward, upon which he immediately brings a flap from the arm. The object of the lining is to give stability to the base of the new nose as well as to prevent curling and contraction of the rims of the nostrils.
Bayer-Payr Method.—Two flaps two and a half centimeters wide are cut from the nasolabial furrow, extending down to the lower border of the inferior maxillary bone, as shown in Fig. 412.
The flaps are dissected up and brought forward and upward, their raw surfaces meeting in the median line, where they are sutured upon one another to the extent of three centimeters, as shown in Fig. 413.
The nasolabial wounds are brought together by suture except for a small triangular space near each pedicle, which are allowed to heal by granulation.
The superior borders of the flaps were then united by suture to the freshened margins of the nose, which have been prepared as shown in the illustration.
The septal ends of the two flaps are likewise sutured to the stump of the old septum.
The raw or outer surfaces of the flaps are to be covered with Thiersch grafts when ready for them, though this may not be necessary with small flaps.
The pedicles of the flaps are not cut until the end of the fourth week, when the fresh ends may be sutured to freshened surfaces of the wings made to receive them.
The disposition of the parts at this period is shown in Fig. 414.
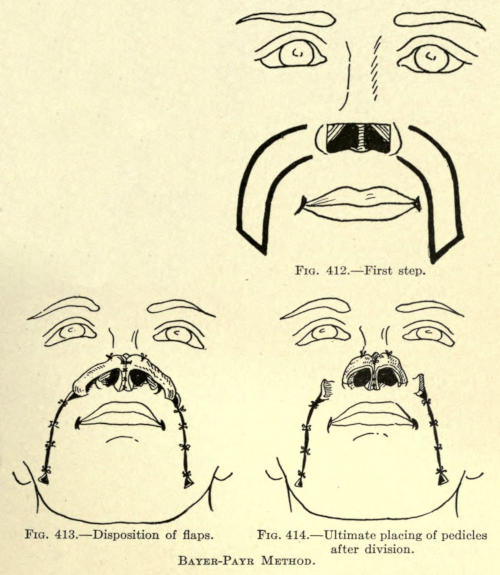
Fig. 412.—First step.
Fig. 413.—Disposition of flaps.
Fig. 414.—Ultimate placing of pedicles after division.
Bayer-Payr Method.
Ch. Nélaton Method.—This author in cases of extensive destruction of the point of the nose advocates the lining of an Italian flap with skin flaps made in similar manner, as in the foregoing operation.
The lining flaps are taken from the nasogenian furrow, placed and sutured as just described, without twisting of their pedicles, and are sutured at the median line and at their free ends to the freshened septal stumps.
The Italian flap is placed over those two flaps immediately, or the Italian flap is first made to unite to the raw margin of the defect, and the two nasogenian flaps are made and employed at a later sitting by subplanting.
The Italian flap may be taken from the arm or forearm, this surgeon preferring the forearm. The attached flap and position of the hand on the forehead where it is retained with an apparatus for the required time is shown in Fig. 415.
The adherent Italian flap and its subseptal addition and the outlines for the lining flaps are shown in Fig. 416.
The secondary nasogenian wounds reduced by suture and the flaps so obtained are shown in Fig. 417. The subseptal section of the Italian flap is raised to[427] show the disposition of the flap ends to form the new septum. The raised flap is brought down and sutured to the raw edges of the two septal flaps covering the median cicatrix, its own cicatrices falling within the rim of the nostrils.
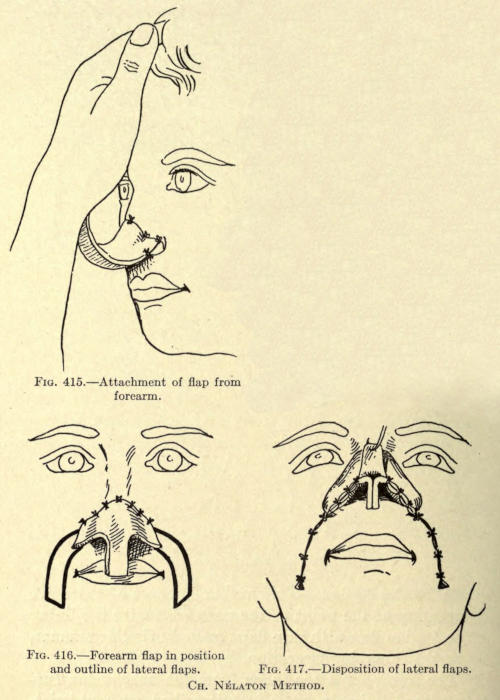
Fig. 415.—Attachment of flap from forearm.
Fig. 416.—Forearm flap in position and outline of lateral flaps.
Fig. 417.—Disposition of lateral flaps.
Ch. Nélaton Method.
This surgeon advises in less severe losses of tissue to do without lining the Italian flap, but to make the latter large enough to be able to fold in enough of its base sections to line the nostrils to the extent of the inferior line of the mucosa. The flap should be cut one fourth longer than the nasal deformity.
This procedure also overcomes to a great extent the shrinking of the nasal orifices.
The pedicle of the flap is cut close to the arm at the end of two weeks. The subseptum may be made at once if the flap shows good nutrition, as evidenced by marked bleeding at the time of cutting away the bridge tissue.
The method of restoration of the wing or wings of the nose depends largely upon the extent of the tissue loss.
The use of the Hindu method is not advisable, since the flap must be made with a long pedicle, which involves the making of a large wound and predisposes to consequent large cicatrices, although many surgeons have resorted to the method. The author does not see any advantage with this method, even if the loss of tissue about the lobule is great.
The best results, both as to the primary and secondary wounds, are those obtained with the Italian method, and in extensive cases the use of a combined flap, wherein the lining flap is taken from the nasolabial furrow or just above it. This leaves a linear scar that does not disfigure the face, and assures of better contour than when a single integumentary flap is employed which, as has been so frequently mentioned, is liable to curl inward and contract in an upward direction, adding little to the area of lost tissue.
The ideal operations are those which include cartilaginous supports, which may be obtained from about the border of the deformity or from some remote place, as of the ear. The surgeon is hardly justified to use the remaining healthy tissue of the nose, unless the case is such that the secondary wound can be corrected, so as not to add scars to the face.
Small defects can be easily corrected by sliding flaps taken from the vicinity of the defect, whether they include cartilage or not, and by granulation or dissection and approximation of the skin, the secondary wound may be entirely closed. It is remarkable how little linear[430] scars show about the nose when the lips of the wounds have been neatly brought together.
The author advocates the use of the continuous silk suture for this purpose, since it fulfills both the object of suture and splint and overcomes the corrugating effect, so often found with interrupted sutures; furthermore, a continuous suture is more easily withdrawn, and there is no danger of wounding the skin on removal, and the discomfort to the patient is greatly reduced.
From the foregoing descriptions of procedure, the surgeon has been sufficiently familiarized with such steps in rhinoplasty as are usually employed, and it would be a matter of constant repetition to rehearse these same steps for the following operations; therefore the author trusts the illustrations given will be sufficiently lucid to work from. All special features to be observed are given.
Denonvillier Method.—The secondary wounds made by the two methods here given may be allowed to heal by granulation or be covered with skin grafts, as heretofore described.
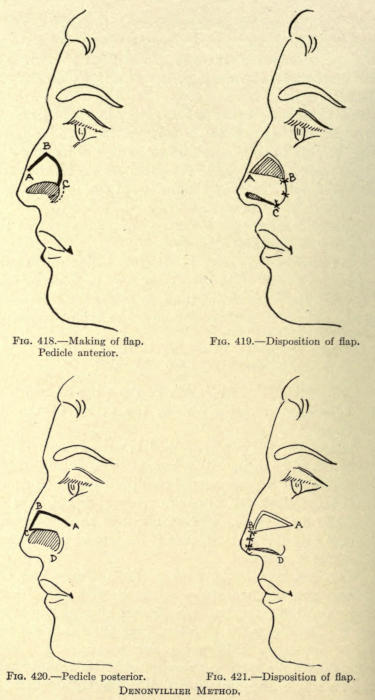
Fig. 418.—Making of flap. Pedicle anterior.
Fig. 419.—Disposition of flap.
Fig. 420.—Pedicle posterior.
Fig. 421.—Disposition of flap.
Denonvillier Method.
Mutter Method.—A skin flap is taken from the cheek and slid forward into the defect as shown.
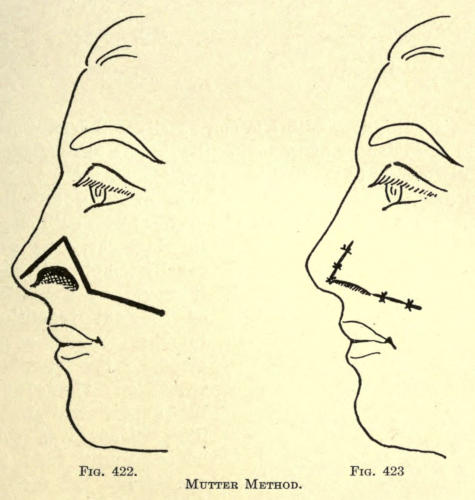
Fig. 422. Fig. 423.
Mutter Method.
Von Langenbeck Method.—The skin flap is taken from the healthy side of the nose and brought into the defect by sliding.
The secondary wound is allowed to heal by granulation.
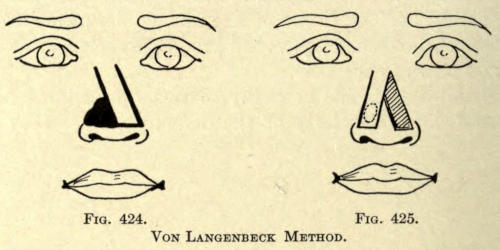
Fig. 424. Fig. 425.
Von Langenbeck Method.
Busch Method.—The same method as above is employed except that for the incision A, C, which, upon dissection of the skin in triangle A, B, C, allows the closure of a larger defect than could be corrected with the lateral nasal flap alone (see Fig. 426).
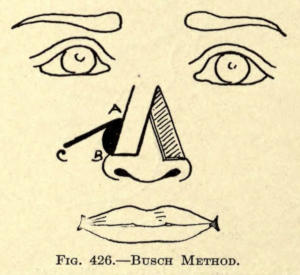
Fig. 426.—Busch Method.
The following illustrations are similar to those given and involve only the skin in the flaps made, as shown.[434] They are only of interest in portraying the position of the flaps and their pedicles.
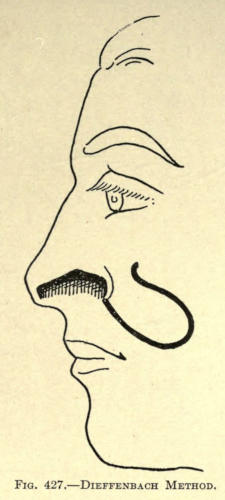
Fig. 427.—Dieffenbach Method.
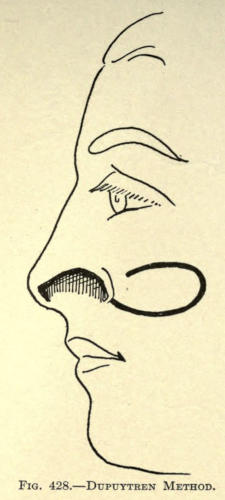
Fig. 428.—Dupuytren Method.
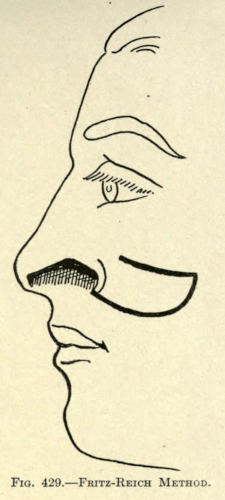
Fig. 429.—Fritz-Reich Method.
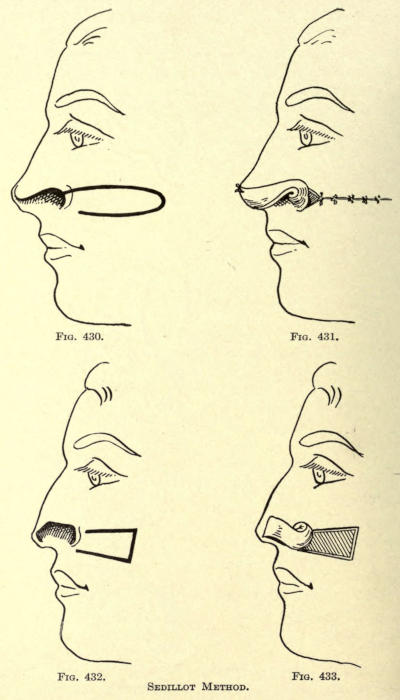
Fig. 430. Fig. 431. Fig. 432. Fig. 433.
Sedillot Method.
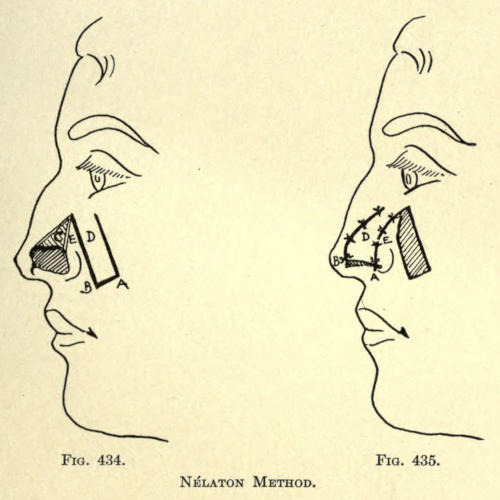
Fig. 434. Fig. 435.
Nélaton Method.
In the Bonnet method the flap is taken from the entire thickness of the upper lip and by twisting is brought into the defect. The pedicle must be cut at a later sitting.
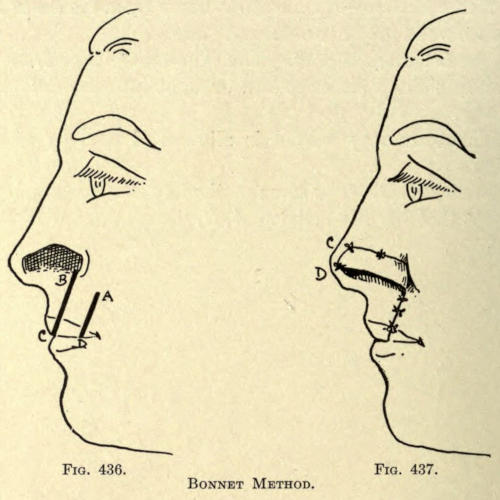
Fig. 436. Fig. 437.
Bonnet Method.
Weber Method.—The flap is made from half the thickness of the upper lip, as shown in Fig. 438, and brought into the defect, as in Fig. 439. The pedicle is cut later.
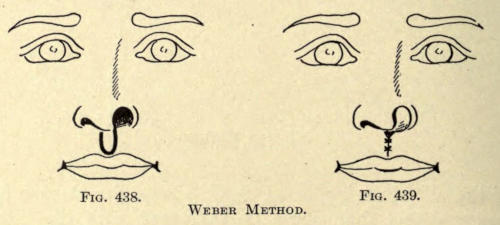
Fig. 438. Fig. 439.
Weber Method.
Thompson Method.—This author uses a lateral flap taken from the cheek, as shown in Fig. 441, and lines it with a flap of mucosa dissected from the septum antero-posteriorly, as shown in Fig. 440, disposing of the latter flap as shown. The raw surface meets the raw surface of the skin flap, as in Fig. 442.
At a later sitting the two pedicles must be severed and adjusted by small minor operations.
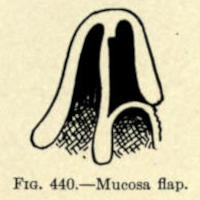
Fig. 440.—Mucosa flap.
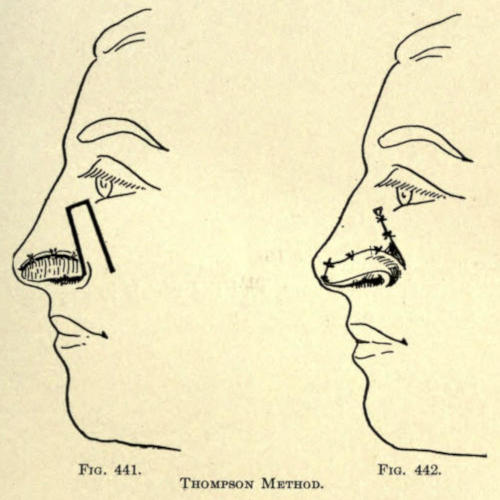
Fig. 441. Fig. 442.
Thompson Method.
Blandin Method.—The flap is made of the whole thickness of the lip. The pedicle is cut at a second sitting.
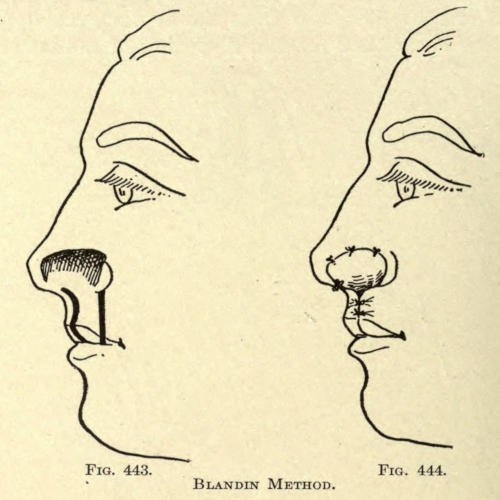
Fig. 443. Fig. 444.
Blandin Method.
Von Hacker Method.—This author adds a flap from the nasolabial region to line that taken from the healthy side of the nose, as shown in the Langenbeck method. There is little cicatrization here, and the result is excellent for defects of large area.
The procedure and shape of flaps as used are shown in Figs. 445 and 446.
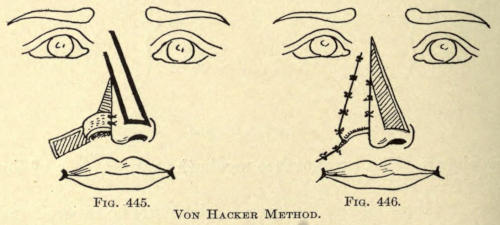
Fig. 445. Fig. 446.
Von Hacker Method.
Kolle Method.—The author dissects away the flap E, A, D when part of the mucosa and cartilaginous tissue remains, and where there is a loss, total or partial, of the alar rima, the transverse incision E being made as long as required to overcome the defect by sliding, as in Fig. 447.
The latter flap is freshened at its inferior border along the line D, and a second or bordering flap of sufficient width to line and face the nostril is taken up from the upper lip, skin only, as shown in area C.
The lateral or upper flap is now slid down to slightly overcome the loss of tissue and the flap C is brought upward by twisting slightly on its pedicle and sutured in place, as shown in Fig. 448.
The secondary wound lying between the lines E and E’, occasioned by the sliding downward and leaving the triangular defect F, is allowed to heal by granulation. The lateral flap is fixed along the line A.
Usually the pedicle of flap C need not be cut, as it adjusts itself under primary union.
The secondary lip wound is closed at once by suture.[438] The author has also used the inverted V incision of Dieffenbach, including the cartilage or part thereof that remains above the defect, and has moved this flap downward, suturing in Y fashion with good results.
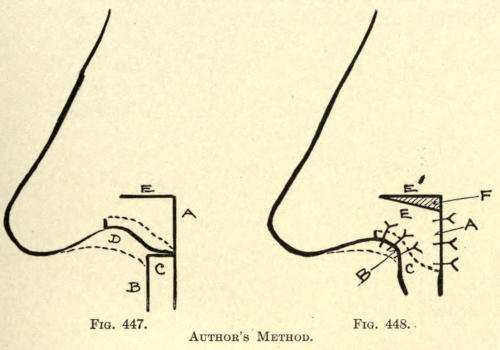
Fig. 447. Fig. 448.
Author’s Method.
Denonvillier Method.—The operation is similar to that of Dieffenbach and the author’s modification just mentioned. Its advantage, as in the latter, is that the inferior border or nasal rim remains intact, and contains what cartilage remains above the defect. The shape of the incision is as shown in Fig. 449.
The flap A, B, C includes the skin and such cartilage as can be used, while the rim below the line B, D retains its lower cicatricial border.
The flap is slid down until the defect has been overcome, and the resultant superior triangular wound is allowed to heal by granulation. The dissection of the flap is made down to the line including the skin or cartilage referred to. At the dotted line B, D the whole thickness of the tissue except the overlying skin is involved.
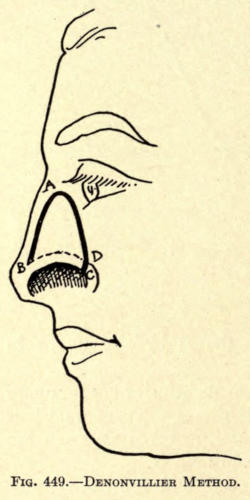
Fig. 449.—Denonvillier Method.
Von Hacker Method.—The flap A, F, C, as shown in Fig. 450, is cut from the entire thickness of the side of the nose attached by its posterior pedicle C.
This flap is moved downward, and its anterior border is sutured along the freshened line A, B, as in Fig. 451, leaving a triangular defect, A, F, C.
Two little triangular flaps of skin are dissected up, skin only, at D, E, C and H, G, C.
Next a rectangular flap, I, K, L, M, is dissected up from the cheek, as in Fig. 452, including some areolar tissue.
The flap should be made sufficiently long, so that when folded over it will fit into the defect without tension, at the same time allowing for contraction.
This flap is sutured into the defect made by the making of the first flap, as shown.
The secondary wound of the cheek is brought together by suture, except for a small triangle near the pedicle to avoid its constriction.
Its raw surface is allowed to heal by granulation. The pedicle is severed in about fifteen days, and may be cut in triangular fashion to make it fit smoothly into the slight defect in the skin just posterior to it.
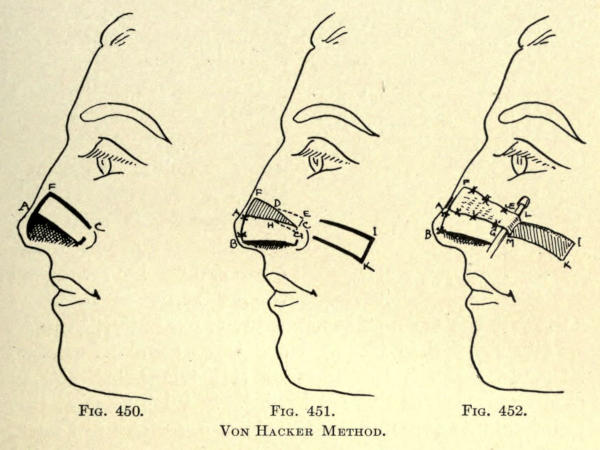
Fig. 450. Fig. 451. Fig. 452.
Von Hacker Method.
König Method.—In this novel method a flap somewhat of the form of the defect is taken from about the[440] entire thickness of the rim of the ear, as shown in Fig. 453.
This flap should be made slightly larger than the defect, since it contracts somewhat immediately after excision.
It is sutured rim down to the freshened wound in the wing.
The secondary deformity of the ear is brought together by suture. The author has found that this cannot be readily done without puckering the rim when the line of excision is made convexly, and advises making it triangular instead. The defect of the nose should be freshened to the same form. The flap from the ear now becomes ideal, fits better, is more readily sutured in place. No sutures should, however, be made through the apex of this triangular flap to avoid gangrene at this frail point. Silk isinglass at this point acts as a splint. Dry aristol dressings are used.
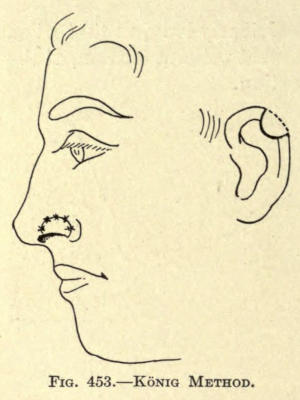
Fig. 453.—König Method.
Kolle Method.—When the defect of the ala is elongated and involves only part of the rim, the author has taken a cutaneo-cartilaginous flap from the back of the ear.
The flap is cut vertically, and is made to include a strip of cartilage of about the size and form of the defect.
The flap is immediately sutured to the freshened defect and folded upon itself with the cartilage facing the inferior margin of the defect.
The flap thus employed exhibits an epidermal face, both inside and outside as well as at the rim of the wing.
A case in which this method was used is shown in the[441] illustrations 454 and 455, in which the defect is shown in the former figure, and the result after the sutures were withdrawn on the sixth day in the latter.
The secondary wound is easily brought together by suture, as the skin is quite flexible at this point.
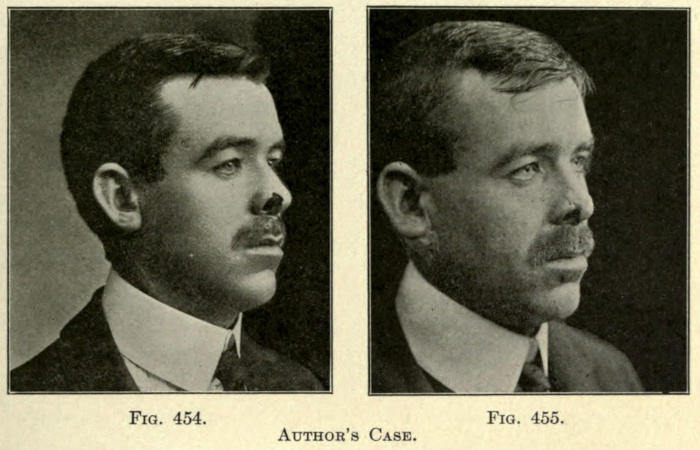
Fig. 454. Fig. 455.
Author’s Case.
This defect of the nose has been restored by the use of skin flaps taken from the forehead, the nose itself, or from half or the whole thickness of the upper lip. The author does not advocate the use of such flaps except those taken from the skin of the inner side of the forearm, just below the wrist, made according to the Italian plan, as heretofore described.
The pedicle of such a flap is cut about the twelfth day, and at a later period, when the inferior or free margin has cicatrized, the subseptum is formed and sutured to the remaining stump or into a wound in the upper lip made to receive it.
The skin of the forearm is nearer to the thickness of the skin of the nose; hence a flap from it is preferable to that taken from the arm.
The method of obtaining the flap has been fully described heretofore.
The results obtained are excellent in most cases. The resulting cicatrix is barely visible, and may be later improved by scar-reducing methods, later described under that heading.
The appearance of the flap after the pedicle has been severed and the subseptal section has been put into place may be observed in Fig. 456, and the final appearance after total contraction, in Fig. 457.
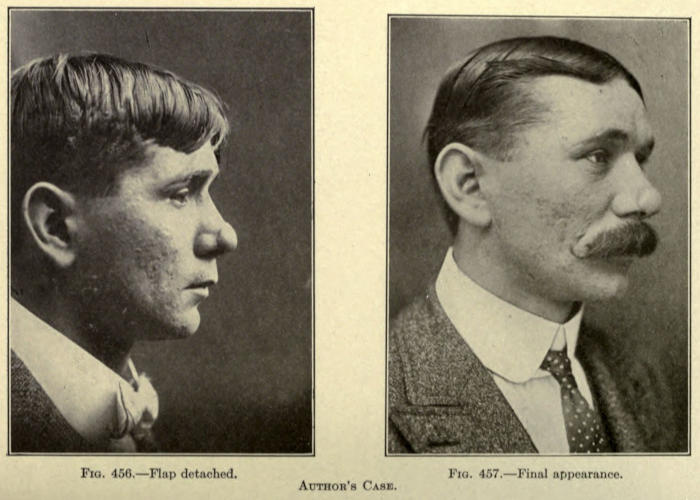
Fig. 456.—Flap detached.
Fig. 457.—Final appearance.
Author’s Case.
For very small losses of tissue about the lobule nonpedunculated skin grafts are to be employed. The author advises including some of the areolar tissue with them to avoid contraction.
These are to be dressed with the blood method referred to under skin grafting. Perforated rubber tissue is to be used next to the epidermal surface to prevent the dressings from tearing away the graft when changed.
Fine twisted silk is most suitable for suturing purposes. The loops must not be drawn too tightly and the knot be made so that it rests upon the healthy skin of the nose.
For the correction of this defect various methods are given, and all of these must be modified more or less, to meet the requirements or extent of lost tissue. In some cases the entire subseptum is absent, while in others there is more or less of a stump remaining. Again in some, the subseptum required is unusually wide and in others quite narrow.
While a number of surgeons prefer making the flap to restore it from part or the whole thickness of the upper lip, as will be shown, the author believes the best[444] results are to be obtained with the Italian flap method, if there be great loss of tissue, or to attempt to restore smaller defects with cartilage-supported nonpedunculated flaps taken from back of the ear, as heretofore described, or the cartilage to be used as a support may be taken from the nasal septum itself, having its pedicle posteriorly.
This strip of cartilage is brought downward, freed at either side from its mucosal attachment, and the skin flap to be used is then made wide enough to be sutured to the inferior mucosa margins as well as to the skin of the lobule.
The method of taking a sliding flap from the healthy skin of the nose is not advisable, because of the resultant disfigurement.
The tissue of the lip, on the other hand, can be used, since the secondary wound can be readily drawn together, leaving only a linear scar. In men, this may be hidden by the mustache.
When the Italian method is used, the method referred to in restoration of the lobule is to be followed.
Blandin Method.—The flap is taken vertically from the entire thickness of the upper lip, as shown in Fig. 458, having its pedicle at the base of the nose.
This strip of tissue is turned upward, mucosa outward, and its freshened free end is sutured to the raw surface of the lobule.
The secondary wound of the lip is sutured as in ordinary harelip, as shown in Fig. 459.
The mucosa soon takes on the appearance of skin, but in most cases remains pink in color.
The flap taken in this way should not be made too wide.
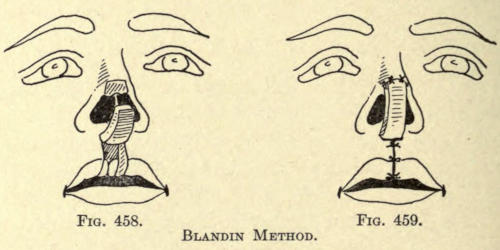
Fig. 458. Fig. 459.
Blandin Method.
Dupuytren Method.—The flap is taken vertically from the skin of the upper lip, reaching down at its free end to the vermilion border, as shown in Fig. 460.
The flap is twisted upon its pedicle and sutured to the skin of the lobule; to facilitate this the left incision is made higher than that on the right.
The pedicle may be cut as with all such flaps, and it may be allowed to remain, if not too disfiguring.
The secondary wound of the upper lip is drawn together by suture, as shown in Fig. 461.
The mucosa of the nose is to be sutured to the raw edge of the flap when that is possible.
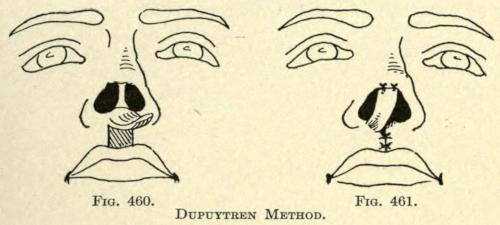
Fig. 460. Fig. 461.
Dupuytren Method.
Serre Method.—This author advises dissecting up a flap from the upper lip, including the skin only, leaving it attached just above the vermilion border, as in Fig. 462.
The free and upper end is sutured to the lobule. When union has taken place, the pedicle is divided and is brought upward and sutured into place. The secondary wound repaired by suturing finally. There is some difficulty in dressing the wound during the time required to have it unite to the skin of the lobule, because of the danger of pressure and consequent gangrene.
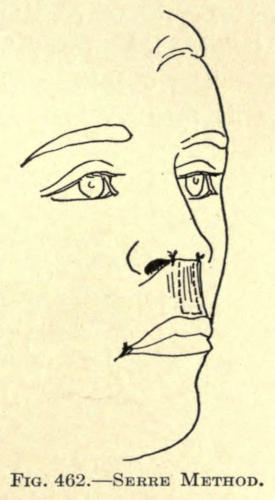
Fig. 462.—Serre Method.
Dieffenbach Method.—This author took up the skin flap transversely or obliquely, as shown in Fig. 463, and twisted it into position, as shown in Fig. 464.
The objection to the direction of making the flap in this manner is that the consequent cicatrization has a tendency to draw the mouth out of its normal position on the wounded side.
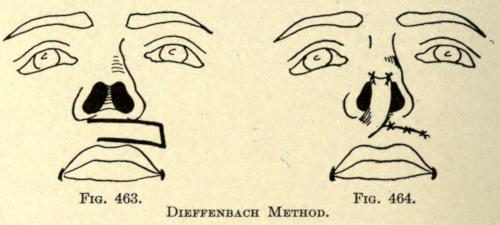
Fig. 463. Fig. 464.
Dieffenbach Method.
The following methods show the taking of the flap[447] from the skin of the nose itself. Unless the defect be very small such methods are objectionable.
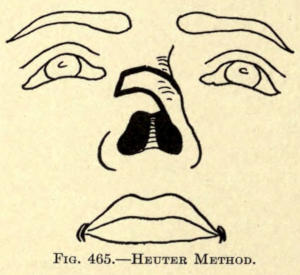
Fig. 465.—Heuter Method.
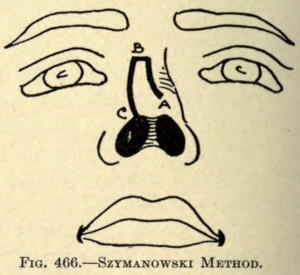
Fig. 466.—Szymanowski Method.
Szymanowski Method.—In the latter method of Szymanowski the flap must be stretched considerably, to close over a lengthy deformity, encouraging gangrene. The deformity is not so great, however, as with the two preceding methods.
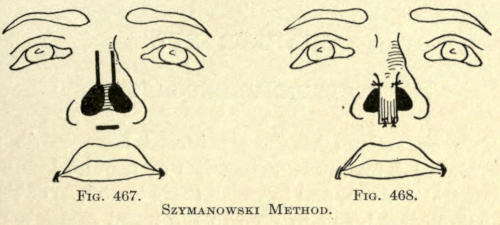
Fig. 467. Fig. 468.
Szymanowski Method.
The author believes a nonpedunculated flap with or without a cartilaginous support should be tried before other methods are resorted to, in all cases, with the hope of healing the graft in place. The fact that the mucosa can in some cases be sutured to the margins of the flap adds much to the possibility of its subsequent life by adding its nutriment to the graft.
The operations herein considered have to do with overcoming deformities, congenital or acquired, as a result of traumatism, and in which there is no loss of tissue, the sole object being to give to the nasal organ a more desirable size and contour.
There are many types of abnormalities involving both the size and shape of the nose. Some of these deformities may be readily corrected by subcutaneous or submucous operations, while others involve more or less cutting of the skin.
The object of the surgeon at all times is to accomplish the best results with as little disfigurement as possible.
Anesthesia.—All the cosmetic operations of the nose should be done under local anesthesia, unless there be serious objections to its employment.
The author advocates the use of a four-per-cent solution of β Eucain, in preference to all others. It is less toxic than cocain and harmless to the patient; no untoward symptoms are exhibited from its use post-operatio. Various patients complain of slight uneasiness about the epigastrium, and many speak of a peculiar weakness about the knees, but these symptoms pass away quickly.
More or less stinging is felt in the wounds made in this manner, immediately after the operations, especially about the lobule of the nose, as with blepharoplasties, but this usually subsides in less than an hour. It may persist,[449] however, in some cases, for several hours. It is well, therefore, to acquaint the patient with this fact to avoid worry or fear.
Where severe, hot applications, dry or moist, may be used to overcome it.
More or less edema follows the employment of local anesthetics, which passes away in various lengths of time, from one to four, or even five days, according to the amount used and the site and circulation of the part operated upon.
In over ten thousand hypodermic injections of eucain the author has observed only two cases of collapse, which responded readily to the usual treatment employed in such event, and has never met with a single fatality.
Sutures.—Twisted silk sutures are to be preferred, as they do not invite sepsis, as softening catgut does, and retain the parts during the entire time required for healing, while the latter is liable to become separated by uneven absorption, allowing the wound to gape at that point and causing more or less of a cicatrix, so intolerant to patients of this class.
Dressings.—Bulky bandages are not required; they heat the parts, and look unsightly. The author employs antiseptic adhesive silk plaster for covering all external wounds, except where the hair prevents its use. Moist dressings are never indicated, except in the later treatment of infected wounds.
This is, perhaps, the most common of all nose deformities. The nose is overprominent about the osseous bridge, extending outward and downward, hook or hump fashion. It may be congenital or the result of external violence.
There are various methods of reducing the redundant bones and cartilage; those involving submucous excision[450] are difficult to perform for the inexperienced operators, and the external means of reduction are advised to be followed. The resultant scar, if the skin has been properly incised and not damaged by retracting pressure, and, lastly, properly and neatly sutured, should be barely visible.
Monk’s Method.—This author made a small incision through the skin just posterior to the inferior edge of the lobule, as in Fig. 469a. Then with a dull instrument, introduced through the opening, he detached the connecting tissue that binds the skin along the anterior dorsum as far as the root of the nose, giving more or less width to this freed area about the nasal bones.
A dull-pointed scissors is introduced through the sublobular opening, and the bones and cartilage are reduced until the desired nasal line has been attained.
The method of procedure is shown in Fig. 469b.
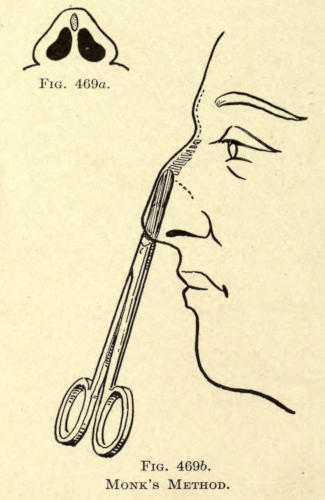
Fig. 469a. Fig. 469b.
Monk’s Method.
The wound is cleansed of all spiculæ of bone or bits of cartilage and the skin opening is closed by suture. Healing takes place with more or less ecchymosis in about six days.
The difficulty the author finds with this method is that it is practically impossible to do good work with the scissors in this position.
The use of an electric drill has been advocated to do[451] away with the scissors, but it is a dangerous instrument and requires great skill for its manipulation and reduces the bone particles to such fine fragments that much of it is left in the wound, which may induce sepsis or cause unevenness of the skin surface until later absorbed or removed. The same fault is observed with cartilage, which it grinds into pulpy pieces and for which it should never be used.
Anterior Median Incision.—This, perhaps the oldest method, has been extensively employed. The incision is made down the median line of the dorsum of the nose, beginning above the deformity, and ending slightly below the inferior bone line, as shown in Fig. 470. The skin is incised obliquely.
An assistant separates the wounds with hook tenaculi, exposing the osseous bridge, as in Fig. 471.
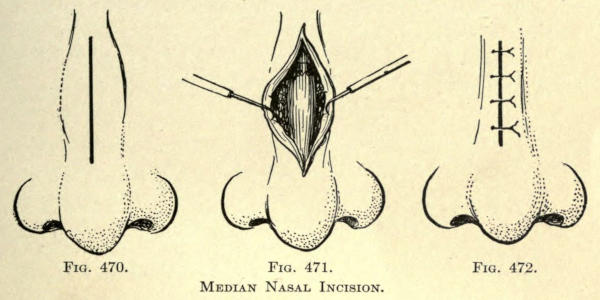
Fig. 470. Fig. 471. Fig. 472.
Median Nasal Incision.
The author advocates dividing the periosteum and dissecting it well back to either side of the bony elevation. By bringing it back over the denuded surface after the chiseling has been done, it aids materially in establishing a smooth surface and hastens the bone repair.
The periosteum being held aside, the straight chisel and mallet are used to reduce the bone. The operator may proceed to do this from above down or vice versa,[452] according to the formation and position of the protuberance.
The redundant cartilage is removed with the knife from above downward, cutting from side to side.
Usually the operator does not remove enough of the cartilage and a new angulation of the nose appears after the swelling has disappeared, necessitating a second operation.
The wound is closed as shown in Fig. 472.
Lateral Incision.—The incision in this case is made slightly posterior to the beginning of the lateral border, as shown in Fig. 473.
The skin is held back, as shown in Fig. 474, and the same mode of procedure is followed as that just given.
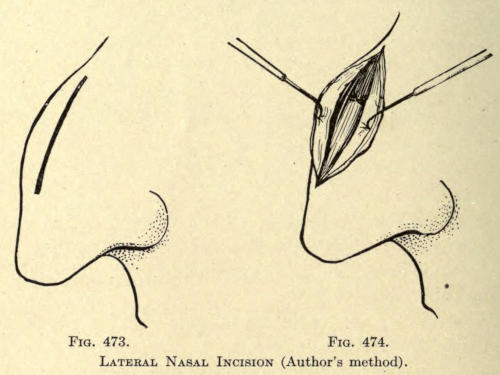
Fig. 473. Fig. 474.
Lateral Nasal Incision (Author’s method).
The operator will have some difficulty to reach the opposite anterior border of bone elevation, especially if the incision has not been made long enough. This should be done. At no time should the assistant employ too much force in retracting the anterior flap to better expose the field of operation; it is certain to cause gangrene of the skin.
To overcome a long scar line, and to facilitate the cutting away of the bone, the author had a special set of chisels made with curved cutting blades, one angular and the other straight-edged. There are two each for working from the right and left sides. The striking point lies midway between the blade and the end of the handle.
They are shown in Figs. 475 and 476.
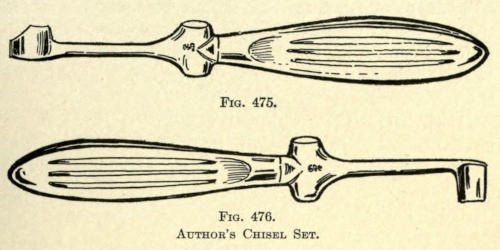
Fig. 475. Fig. 476.
Author’s Chisel Set.
To the set the author has added a suitable metal mallet, an instrument very hard to obtain for osteoplastic operating. All the mallets obtainable are too large and heavy for delicate work (see Fig. 477).
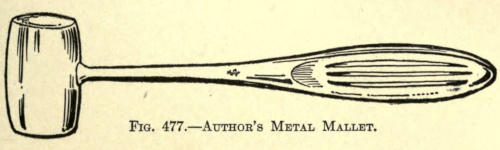
Fig. 477.—Author’s Metal Mallet.
After the bone is reduced to the proper level, the cartilage is cut away as before described, and the wound is sutured.
The resultant scar is much better than when made in the median line, and is not so noticeable in this position.
This operation gives the best results of all external methods employed for this purpose.
(Retroussé Nose)
This condition is frequently a deformity. The base of the nose is tilted upward, unduly exposing the nares.
The author prefers to bring the lobule down by excision of the anterior third of the subseptum in preference to submucous dissection of the cartilaginous tissue, causing the deformity.
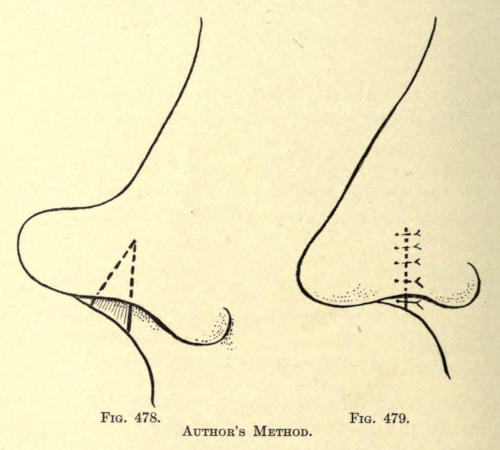
Fig. 478. Fig. 479.
Author’s Method.
With an angular scissors introduced through the nares, a triangular section of the septum is removed, as shown in Fig. 478. The apex of the triangle should be placed well up into the septum to break the elasticity of its structure, the base of the triangle being sufficiently wide to somewhat overcorrect the deformity.
Such noses are usually narrow at the lobule, and no interference with the lower lateral cartilages is called for.
The septal mucoid and the subseptal skin wounds are brought together by suture, as shown in Fig. 479, leaving only a slight transverse linear scar on the subseptum.
Roe corrects this deformity by making an incision, either vertically or horizontally, in the mucosa in one or both nares, through which he introduces the blades of a fine curved scissors, with which sufficient redundant tissue is removed to bring the lobule down into the desired contour.
The mucosa should be sutured to facilitate rapid cicatrization. The operation should be overdone to get the desired result.
Not infrequently the extreme convexity of the lower lateral cartilage must be overcome by either removal submucously or by excision of the cartilage itself, employing an elliptical incision in the mucosa for the purpose.
The alæ are kept in position after such ablation by compress dressings or by a suture made transversely through both wings of the nose and the septum, and tied over a quill or cork support placed externally upon the skin at either side of the nose. This is removed about the sixth day.
Sheet lead or a splint of aluminum of proper thickness and covered with gauze may also be used to retain the parts during cicatrization.
When the lobule is unduly broad at its base and is more or less concave above the rim of the alæ, it can be reduced by removing a diamond-shaped piece of tissue at either side of the subseptum.
The bases of the two triangles making up the diamond at its widest area meet at the anterior rim of the nostrils,[456] extending with their apices upward and backward, as shown in Fig. 480.
If there be a prominence of the cartilaginous structure of the lobule, this may be removed subcutaneously after the two ablations have been made.
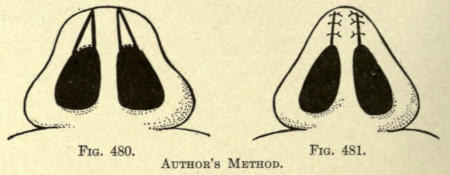
Fig. 480. Fig. 481.
Author’s Method.
Before suturing the wounds, it is advisable to free the skin of the inferior lobule to overcome tension.
The sutures are applied as in Fig. 481. None are used to unite the mucosa unless the interior wounds are large enough to permit of their use.
The operations herein described apply particularly to the correction or reduction of an overprominent nasal tip due to an excessive growth of congenital malformation of that part of the nose, giving the organ undue prominence and a hooklike appearance, usually associated with a narrow, sharply upward inclined upper lip.
Pozzi Method.—The same operation, on a larger scale, can be readily employed for the correction of hyperplasia nasi and rhinophyma.
In the operation of Pozzi (Bulletin et mémoire de Société de chirurgie, 1897, p. 729) an elliptical section of skin and cartilage are removed from the lobule with its widest part corresponding to the point of the nose; the cicatrices occasioned thereby are practically as bad, if not worse, than the unscarred overprominent nose, while[457] the submucous procedure of Roe (Medical Record, July 18, 1891) is not only insufficient in these cases, but, according to my experience, practically useless.
Roe Method.—Roe’s method requires a submucous extirpation of the redundant cartilage at the tip through a necessarily small opening within the nasal orifice, also the division in several places of the anterior fold of the lower lateral cartilage with the object of reducing the undue convexity of the alæ. The latter is, we might say, impossible, since the cartilages will be reduced by such a method, even under pressure dressings, which are likely to cause gangrene of the skin of the wings; or if this be avoided, the cicatrix resulting from such division usually restores the very fault that it is expected to overcome, while the mucous lining of the alæ becomes thickened and more firmly tied down than previous to the operation.
One is tempted to exsect the major curvature of the lower lateral cartilage, but this leads to a flattening of the wings of the nose, partial atresia of the nasal orifice, and a decided lack in its symmetry.
Secondly, in Roe’s operation there is always a lack of knowing how much or how little to remove of the cartilage of the tip, a second cosmetic operation being made necessary after the parts have contracted and healed, a common fault with most cosmetic plastic operations performed under local anesthesia, owing to the immediate edematous enlargement following its hypodermic use.
Operation as Commonly Practiced.—The operation heretofore most commonly practiced is one in which an elliptical piece of skin is cut from the tip of the nose, followed by the extirpation of the anterior prominences of the lateral cartilages, and amputation of the septal cartilages. Unfortunately, the result, at first quite satisfactory to the eye, culminates in the pulling apart of the cicatrix formed by bringing the sides of the wound together[458] along the median line with a later depression of the tip in this median line, occasioned by the outward traction of the lower lateral cartilages. Even a second or third operation does not overcome this result entirely, and at best leaves an ugly irregular gash in the median line of the tip and the columna.
In one of the cases here cited this same operation had been unsuccessfully tried twice by another surgeon, with very unsatisfactory and unsightly result. (Case II.)
The ideal operation for all of this type of cases from the view of the surgeon is to leave as little disfigurement as possible, and the method to be here considered, when properly followed, leaves no scar whatever, except for a slight white line across the columna of the nose, where it is out of view, and when contracted offers no objection on the part of the hypercritical patient.
Author’s Method.—The method of the author is as follows: Given a nose, typified by the illustration in Fig. 482, the skin above the site of the operation is thoroughly cleansed with soap and hot water, then rinsed with alcohol, ninety-five per cent, and vigorously scrubbed with[459] gauze sponges, dipped into hot bichlorid solution, 1 to 2,000, followed with a thorough lavage with sterilized water. Both nostrils are now cleansed with warm boric-acid solution by the aid of small tufts of absorbent cotton wound over a dressing forceps. The patient is then instructed to breathe through the mouth during the operation. A number of small round gauze sponges dipped into sterilized water and squeezed dry are placed within reach of the assistant. About one drachm of two-per-cent Beta Eucain solution is now injected about the tip of the nose, the columna, and the alæ, as far back as their posterior fold.
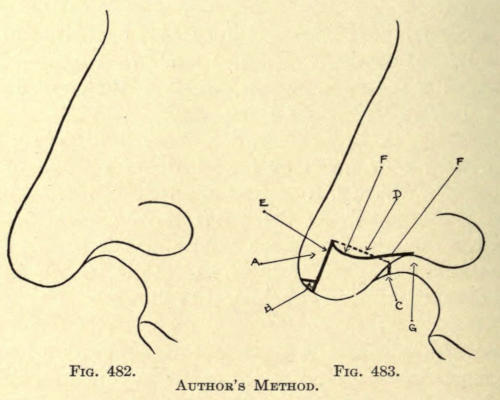
Fig. 482. Fig. 483.
Author’s Method.
A thin bistoury is then thrust into the nose from right to left, entering at the point E (Fig. 483), and brought down parallel to the anterior line of the nose, and emerging below the tip in a line with the anterior border of the nasal orifices. This procedure leaves a strip (A) about one quarter inch wide, laterally, rounded at its inferior extremity, and attached superiorly to the nose. Next the round inferior tip (B) is cut away obliquely, sloping inward toward the nose by the aid of a small angular scissors. Each blade of the angular scissors is now placed into each nostril, the tips of the blades inclined forward, and the columna or subseptum is divided at C, also the septum along the line D up to a point a little above the first incision made externally at E. The two arterioles of the columna are controlled by the use of mosquito-bill forceps. The two projecting folds of the lower lateral cartilage in the columna are next severed as deeply as possible to give mobility to the stump, a step necessary to overcome the changed position, otherwise resulting in a droop, which would have to be corrected at a later sitting.
The next step is to give the needed shape to both wings. This is accomplished with a specially designed scissors, so curved on the flat that its convexity facing upward corresponds to the normal curvature of the orificial[460] rim. A clean cut with these scissors, beginning at G and ending at the point E, is made, leaving the base of the nose, as shown in Fig. 484. The anterior flap A is now bent backward to meet the stump of the columna at C. If it does not fall readily into place a little more of the septal cartilage is removed along the line D until this is accomplished.
It may be necessary to shorten the flap A in cases where a very prominent hook is to be corrected.
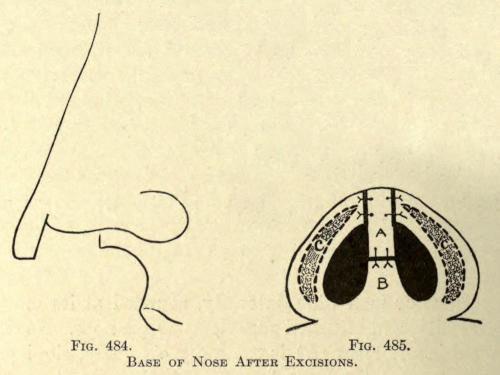
Fig. 484. Fig. 485.
Base of Nose After Excisions.
The free end of the flap A is now sutured with No. 4 sterilized twisted silk to the stump of the columna at B. Two stitches usually suffice (see Fig. 485). One or two sutures may also be taken across the angles of union of the alæ and the flap A. The inferior raw surface of each wing may be found to be too wide, owing to the presence of the thickened cartilage at this point of the wing. The skin and the mucous membrane are then carefully peeled away from the cartilage, and the latter cut away as high as possible, or a gutterlike incision is made along its edges as shown in C (Fig. 485), excising the elongated elliptical piece of tissue which includes the cartilage. The raw mucocutaneous edges of the wings are now brought together with a No. 1 twisted silk continuous suture, completing the operation.
An antiseptic powder is dusted over the parts operated on, and small gauze dressings are applied with the aid of strips of silk isinglass plaster. A small tampon of cotton, well dusted over with an antiseptic powder, is placed into each nostril.
The dressings are changed the second day, when the resultant swelling will have practically subsided. The sutures in the columna are removed the fourth day preferably, and those of the wings about the sixth day. Complete cicatrization follows in about ten days, when the patient can be discharged.
The following cases are given to show the types of cases thus far operated upon and to illustrate the results obtained:
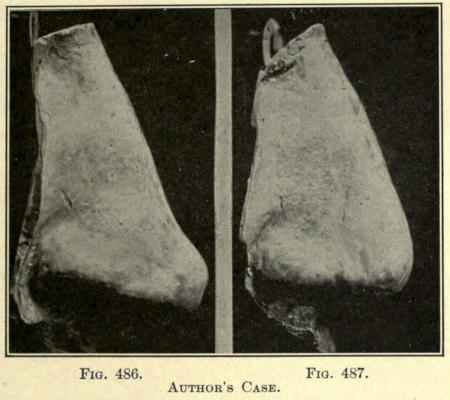
Fig. 486. Fig. 487.
Author’s Case.
Case I.—Mr. R., aged thirty-two; foreman mechanic. Had been operated upon for angular nose, also at point of nose by Dr. S. Presented himself for operation October 19, 1904, when cast was made (see Fig. 486). Bromides given during recovery. Patient had been subject to fits of depression on account of his nose for over a[462] year. Wounds healed in ten days, when second cast was made (Fig. 487). Complete recovery.
Case II.—Miss B. P., aged twenty-two; actress. Patient presented herself for operation March 22, 1905. A long, irregular depressed cicatrix showing at point of nose, the result of an attempt to reduce tip of nose by an elliptical extirpation of the lobule (Dr. N.). No cast was made of the case at the time, so that a second cast showing the result would be of no use. Recovery complete in twelve days. Patient returned to her profession three weeks later much pleased with the result.
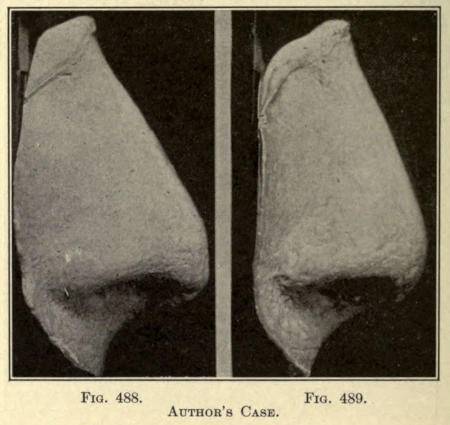
Fig. 488. Fig. 489.
Author’s Case.
Case III.—Mr. L. L., aged twenty-eight; broker. Presented himself, at the advice of Dr. T., for operation May 2, 1905. Cast of cast made and shown in Fig. 488. Uneventful recovery in twelve days, when case Fig. 489 was made.
Case IV.—Mr. M. B., aged twenty-eight; operatic baritone. Presented himself for operation June 4, 1906.[463] Photograph shown in Fig. 490. Uneventful recovery in fifteen days, when photograph in Fig. 491 was made; angular nose operated upon (at this time discharged; recovery complete).
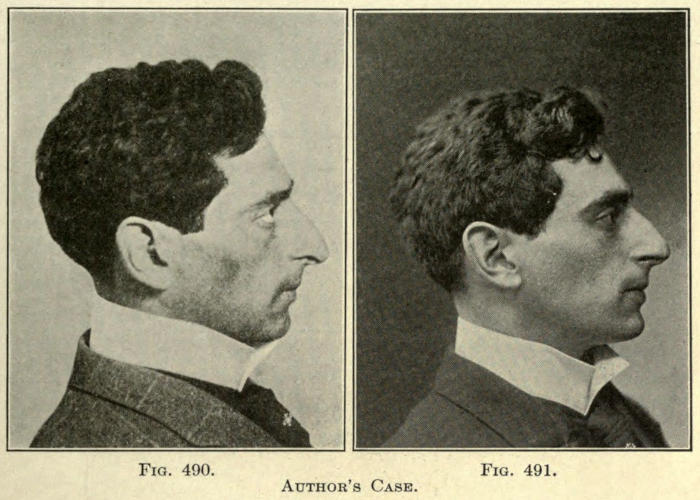
Fig. 490. Fig. 491.
Author’s Case.
Case V.—Miss L. W., aged twenty-seven. Presented herself for operation and cast (Fig. 492) made August 4, 1906. Uneventful recovery in ten days. Cast of result made August 18, 1906 (see Fig. 493).
In each of these cases the patient was discharged highly satisfied and well pleased with the result of the operation, although in Case V the patient was requested to return in about one month for an operation to reduce the width of the wings of the nose, which was not attempted at the first sitting, but could have been with little difficulty by beginning the primary incision at E, Fig. 483, higher up, and cutting out a triangular section on either side of the flap A, the apex of each triangle being at point E, and the base along the line D. The wounds are sutured along the dorsum of the nose with No. 1 twisted[464] silk, after exsecting much of the lower lateral cartilages of the wings, as can easily be reached in the triangular point formed by the raw dorsal border and the inferior edge (F). The latter method, however, would be likely to leave a slight cicatricial line on either side of the nose. This could be much overcome by making the incision from point E to B obliquely to the plane of the skin, likewise the posterior sides of the triangles mentioned, just as the incisions at B, and across the columna at C, are made. Recovery should be complete in five days.
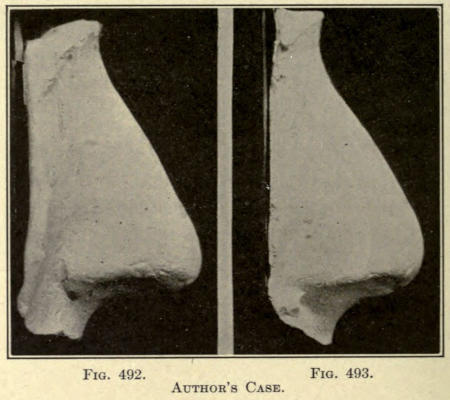
Fig. 492. Fig. 493.
Author’s Case.
Where there is a lack of lobular prominence it may be enlarged and brought forward by a subcutaneous prothesis if the skin is flexible enough to permit of injection, as has heretofore been described. If this cannot be done, the following operation may be employed to advance the point of the nose, and reduce the width at its base so commonly observed with these cases.
Gensoul Method.—A deep incision is made from the floor of each nostril downward and backward, meeting at a point just below the union of the subseptum with the upper lip, as in Fig. 494.
The deeper tissues are loosened from their attachments to the bone until the subseptum at its base, including the triangular appendage thus made, is freely movable.
The lobule is now drawn forward to its required prominence and the parts are sutured Y fashion, as in Fig. 495.
If the subseptum be too wide, an elliptical section is removed, including the cartilage, sufficient to give it the desired thickness when brought together, as illustrated. The lips of the wound are brought together as shown.

Fig. 494. Fig. 495.
Gensoul Method.
When the base of the nose at its juncture with the lip is too broad, the reversed procedure mentioned under correction of a broad lobule is to be employed.
The diamond-shaped section is removed from the posterior rim of the nares as shown in Fig. 496.
The tissues at either side are freed from their subcutaneous attachments so as to render them mobile.
The mucosa and skin wounds are sutured as in Fig. 497.
A retention splint or suture is to be employed to retain the parts as with the anterior lobule operation just described until healing has taken place.
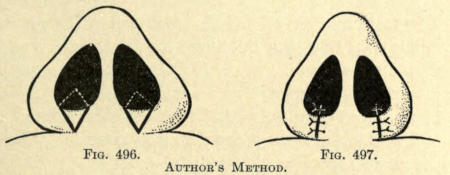
Fig. 496. Fig. 497.
Author’s Method.
When the alæ are thickened they add to the width of the nasal bone and cause more or less atresia of the nostrils. The cause may be due to superabundant connective tissue or a congenital enlargement of the lower lateral cartilage.
To overcome this deformity the following operations may be followed:
Linhardt Method.—This author excises an elliptical section of tissue from the inferior base of both nasal wings, as shown in Fig. 498.
A similar procedure has heretofore been described in Fig. 485 in connection with correction of the lobule.
The section removed includes as much of the cartilage as is necessary to thin out the wing of the nose and to overcome the atresia.
The parts are sutured as shown in Fig. 499.
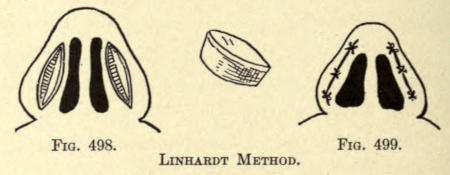
Fig. 498. Fig. 499.
Linhardt Method.
Dieffenbach Method.—In this method cone-shaped section of skin and cartilage are removed from the wings of the nose, as shown in Fig. 500.
If the septum is too wide, two or three of the same shaped sections are removed from it.
The skin wounds are drawn together by suture, as shown in Fig. 501.
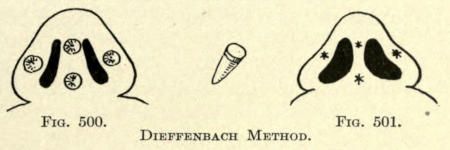
Fig. 500. Fig. 501.
Dieffenbach Method.
In this deformity the nose is bent or twisted to one side. The cause is usually traumatism, but may be congenital.
The interior cartilaginous septum is usually found malformed on one or both sides.
To correct the deviation, the redundant cartilaginous septum is cut or sawed away to clear both nares and the anterior nasal vestibule. After this has been done the nasal attachments are freed subcutaneously, until the nasal organ is freely movable from its attachment to the superior maxillary bones.
The nose is now placed in the position desired, somewhat overdoing the correction, and is held in place by gauze packs in the nares or by Roberts’ spear-pointed pins thrust through the lateral skin of the nose at either side and through the septum, as shown in Fig. 339, p. 365.
The use of the pins placed as shown allows of free drainage to the nares and gives little inconvenience to the patient.
Plugs of gauze contract and harden, thus overcoming the object of their use and cause a disturbance of the wounds and pain when reapplied.
The pins should not be withdrawn until the nose has[468] healed into its new position, or begin to cause irritation of the parts punctured.
Where the deviation is unilateral it should be corrected by subcutaneous injection, as previously described.
The protuberance of bone lies external to the middle meatus, involving an abnormal convexity of the nasal process of the superior maxillary. Its external removal or reduction involves considerable tissue and would leave a conspicuous linear scar, therefore the surgeon must attempt its reduction from the inner nose.
The author prefers to make a horizontal incision below the inferior border of the process, beginning anteriorly just before the articulation with the nasal bone and extending backward as far as the view from the nare will allow.
Through this opening, the skin overlying the bone is raised by dull dissection. A fine nasal saw is next introduced through the submucous wound and several vertical incisions are made into or even through the bone about three sixteenths of an inch apart, dividing the convexed osseous tissue into several sections adherent at their superior extremity which lies inferior to the insertion of the levator labii superioris alæque nasi muscle.
A forceps, such as Adams’s, is now introduced and each section of bone thus made is fractured from below upwards inwardly to produce a concavity of the osseous tissue.
The operation requires considerable dexterity. The amplitude of the sawing movement is very much restricted, because of the palpebral muscular attachment just above.
A frail bone cutting forceps may be employed and[469] the lower half of the process be removed to avoid encroachment upon the middle meatus, but this is rarely necessary, as that chamber is found unusually wide in this case. If the bone is removed, the remaining bone may be cut into sections, as described, or by the cutting forceps, and fractured backwards as described.
Retention dressings must be resorted to, to keep the fragments of the bone in their new position until cicatrization has been sufficiently established to keep them in place.
When possible Roe advises sawing off the convexity submucously and, after loosening the skin over the dorsum of the nose, to move the bony plate thus made over to the opposite side of the nose and into the concavity usually found there in these cases. If there be no deviation at the latter site the bone plate can be entirely removed through the inferior wound in the mucosa.
Several references have been made in the preceding chapter to the specific use of electricity without a description, however, of its source or application. The author does not deem it necessary in this volume to go into the principles of electricity, and takes it for granted that the practitioner is sufficiently familiar with a knowledge of the rudiments of the subject and that he understands the meaning of an electric cell commonly known as a battery.
The Electric Battery.—An electric cell or battery is made up of two poles which are named positive, designated by the + (plus) sign, and negative by the - (minus) sign. In the usual form of cell used the parts are made up of a carbon and zinc cylinder placed into a glass jar containing the electrolyte or actuating fluid. The latter is either an aqueous solution of potassium bichromate or salammoniac contained in a glass jar.
For continuous use or open circuit work the Le Clanche type of cell is most practicable.
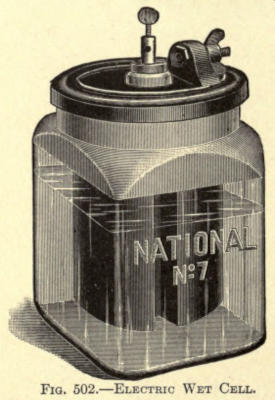
Fig. 502.—Electric Wet Cell.
In Fig. 502 a cell of this type is shown in which the positive pole or element is composed of a solid piece of carbon forming a cover to the glass jar as well, and the negative element is of zinc. The covering over of the jar prevents evaporation of the solution and adds much to its life.
The Voltage or Electromotive Force.—The voltage or electromotive force from such a cell averages about 1.5 volts. Voltage represents the force or propelling power of current known scientifically as the electromotive force and designated EMF. Owing to the great resistance of the body to the electric current, a proportionate force is required to attain therapeutic results.
The unit measure of the quantity of current is known as the ampère. As this is too great for therapeutic use, the thousandth part, or milliampère, is employed, and for the purpose of measuring the amount of current given the patient the milliampèremeter is included in the circuit or flow of current.
The unit of resistance is termed the Ohm, and to simplify the method of electrotherapeutic administration the practitioner may refer to Ohm’s law as a guide. He must remember the average resistance to the current of the parts to be operated on by this process. The law is as follows:
| EMF or Voltage | ||
| C or Current in Ampères | = | ————————— |
| R or Resistance, |
or commonly written
| R | ||
| C | = | ——— |
| EMF |
The Rheostat.—When we consider that the resistance between electrodes placed on the palm of the left hand[472] and the back of the neck is about 4,000 Ohms, it may be readily understood that considerable voltage is required to overcome this resistance before the proper amount of current can be employed. Since each cell, for quick reference, may be said to represent one volt, at least twelve and not more than sixteen cells would be required for electrolysis. Not all of the current given off by a battery of such number of cells should be used on a patient for electrolytic purpose. Some method must be employed to reduce this voltage and to control it at will. This is necessary since the life of a cell varies and its current capacity is limited according to the use the cell is put to. An instrument of this nature is called a rheostat and is usually made of graphite or metal wire. Water resistances are also used, but they do not permit of a constant current because of the consequent heating and decomposition of the water into its elements at the two metal poles exposed to the water. The proper instrument will be referred to later.
The electric cell represents a certain voltage; to add to this more cells are needed and connected with each other so that each adds its voltage to other or the circuit. The method of connecting cells in this manner is called series connection, in which the carbon element of one cell is connected with the zinc of the next, and so forth, until the last cell, leaving two free poles, one carbon and a zinc to which the wires to hold the electrodes for the patient are connected. As has been said, the carbon is the positive pole and the zinc the negative. The method of connection is shown in Fig. 503.
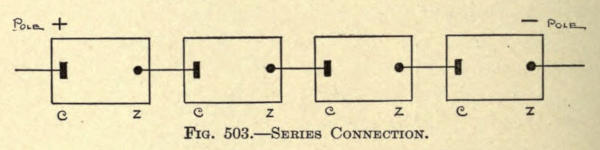
Fig. 503.—Series Connection.
These two poles when brought in contact with human[473] tissue exhibit different action and effect. Without going into electro-chemistry it may be said the current of the positive pole is sedative and that of the negative irritant or destructive. That oxygen and acids are freed at the positive pole and hydrogen and alkalies at the negative pole.
It is due to these properties of the current that it is employed therapeutically, but to properly employ it the current must be controlled so that the exact amount given or used can be estimated. This is accomplished first of all by the interposition of resistance within the circuit. This resistance should be such that the current can be increased or decreased at will. It has been referred to and is called a rheostat. Its position in the circuit is shown in Fig. 504.
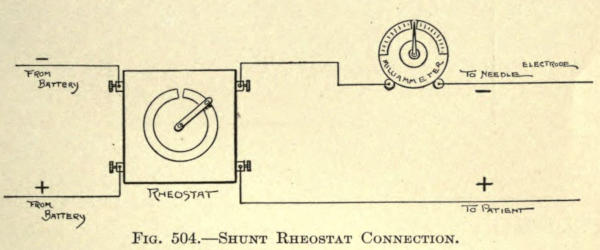
Fig. 504.—Shunt Rheostat Connection.
Cell Selector.—The physician may do without such a rheostat and use a cell selector with the object of adding one or more cells to the circuit at will. Such instrument is composed of a marble or wooden base with a number of disks upon it, each disk representing a cell of the battery. A metal arm is made to slide over these disks, and as it advances over each disk the current from that cell is added to the circuit. It may have a second arm which is used to cut out the current from the cell or cells at the beginning of the circuit—in fact, will permit of the selection of any cell in the circuit by proper manipulation. Such a selector is shown in Fig. 505.
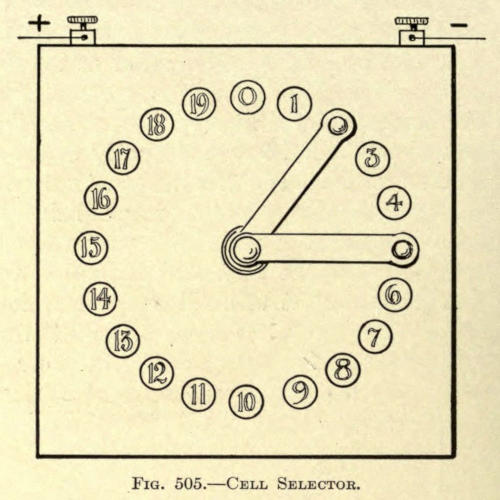
Fig. 505.—Cell Selector.
The connection of the cells of the battery when a selector is used varies from that just mentioned. The proper wiring with the disks of the Selector is shown in Fig. 506.
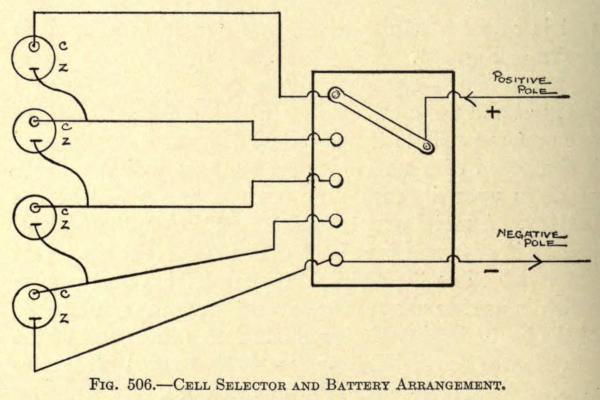
Fig. 506.—Cell Selector and Battery Arrangement.
Milliampèremeter.—The fact that a proper resistance has been forced in circuit is not alone sufficient to permit of the proper use of current for electrolysis. A measuring device should be included, as has been referred to and called the Milliampèremeter or Milliammeter. It is shown in Fig. 507.
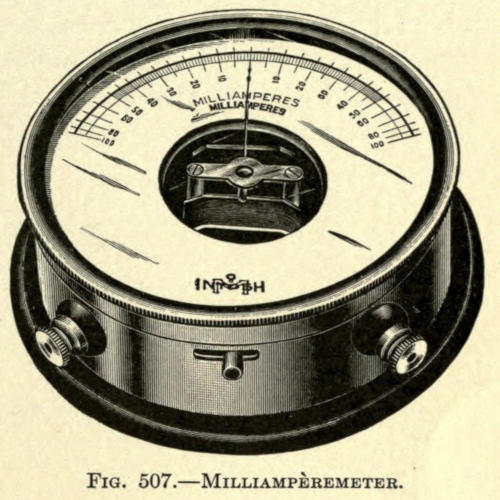
Fig. 507.—Milliampèremeter.
The method of connecting this instrument in series with the current from the rheostat has been shown in Fig. 509.
The Electric Current.—Where the operating room of the physician is provided with street current it will be found[476] more economical and cleaner to use that current for this purpose.
Usually the direct current is furnished of a voltage varying from 100 to 125 volts. To utilize such a current a wall plate is employed and connected to the circuit, as shown in Fig. 508. The resistance of an electric lamp is added to guard against injuring the patient if by any accident or negligence the circuit has been improperly closed.
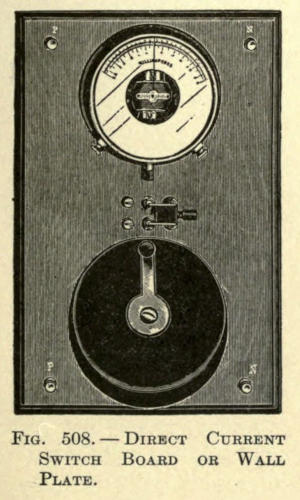
Fig. 508.—Direct Current Switch Board or Wall Plate.
Whether the street or battery current is used with such a plate makes no difference except that with a battery circuit the lamp is not used. The connections are given in Fig. 509.
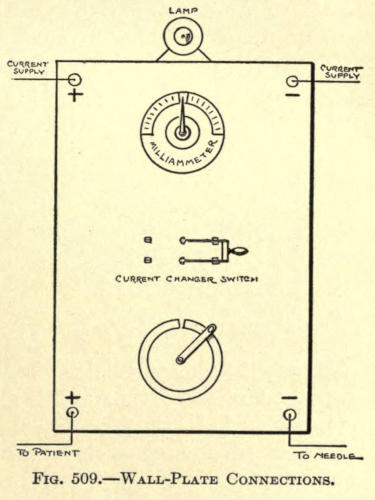
Fig. 509.—Wall-Plate Connections.
It will be observed that a current changing switch has been added to the wall plate. This is included in the circuit to permit of changing the poles to the patient without interfering or disconnecting the electrodes if desired at any time during treatment.
Portable Batteries.—The above instruments and circuits refer to those to be used in the operating room and are stationary. The physician may be called upon to treat a patient at a distance and for this purpose must have a portable battery.
There are many such instruments on the market of both dry and moist cell type. The moist cells usually[477] require a bichromate of soda or potash solution and are so constructed that the carbon and zinc poles are taken out of the electrolyte or solution and placed into water-tight compartments provided for them. Such an apparatus is shown in Fig. 510a.
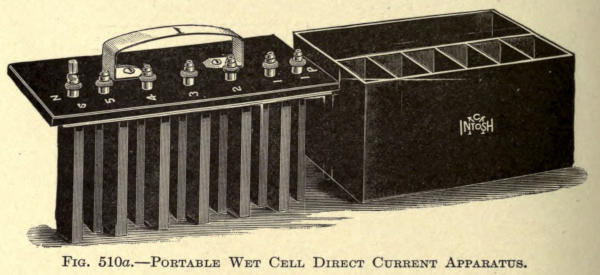
Fig. 510a.—Portable Wet Cell Direct Current Apparatus.
The best cell for this purpose is the silver chloride battery. It is compact, light in weight, and gives a steady current. The only objection is the high cost.
Portable batteries should be furnished with a milliampèremeter. A type of a compact dry cell direct current apparatus is shown in Fig. 510b. In the end the best apparatus proves the most economical.
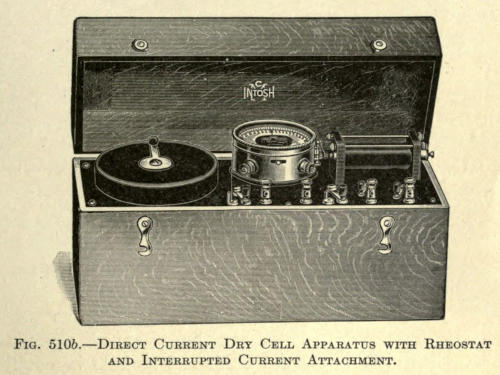
Fig. 510b.—Direct Current Dry Cell Apparatus with Rheostat and Interrupted Current Attachment.
Electrodes.—Having the circuit or current under control, it now becomes necessary to attach electrodes to the free poles to be able to properly apply it to the patient. These electrodes vary considerably according to their use. The author will refer to only those that are of service in electrolysis.
Sponge Electrode.—The one electrode held by the patient is usually made of a metal disk covered with felt[478] or sponge attached to a wooden handle and is shown in Fig. 511.
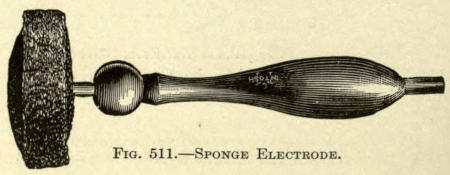
Fig. 511.—Sponge Electrode.
This electrode represents the positive; the negative pole is held by the operator. When used, the felt or sponge is moistened with warm water to which a little salt has been added and is placed into the palm of the hand, sponge inward.
The author prefers to use a plain metal disk with the sponge and places a piece of absorbent cotton or gauze over it when in use for hygienic reason.
When the operator prefers he may resort to arm or wrist electrodes which can be clamped upon the limb and be held in position and shown in Fig. 512.
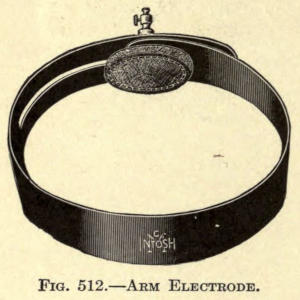
Fig. 512.—Arm Electrode.
The hand electrode is of greater service since the patient can regulate or make and break the current at will, a matter of no small consequence when fairly large currents are being used to destroy a growth upon the skin of the face.
Needles and Needle Holders.—For the negative electrode the operator uses a needle holder with a needle of proper form and material.
Two needle holders are shown in Figs. 513 and 514.
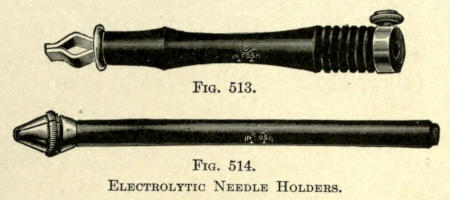
Fig. 513. Fig. 514.
Electrolytic Needle Holders.
When the operator desires he may employ an interrupting[479] needle holder with which he can make and break the current at will during the operation. It is shown in Fig. 515.

Fig. 515.—Interrupting Current Needle Holder.
Such a device is not advocated, since the patient is liable to jump as the current is made suddenly, because of the sharp stinging pain felt at the point when the needle has entered the tissue or hair follicle, often resulting in the breaking of the needle and possible injury to the patient.
Other operators employ a small magnifying glass which may be attached to the holder, as in Fig. 516, and by a sliding arrangement be moved up or down the handle to adjust the lens to the proper focus. This arrangement is indeed novel and may be of service in removing fine superfluous hairs, but the author has never resorted to the method.
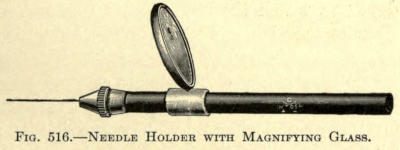
Fig. 516.—Needle Holder with Magnifying Glass.
The proper kind of needle to be used for electrolysis varies with the device of the operator. The ordinary cambric needle usually advocated is too stiff and thick. Jeweler’s broaches are better, but are very brittle and easily broken. The ideal needle should be very thin and made of platinum or irido-platinum. The author prefers the sharp to the bulbous-pointed. For the removal of other blemishes than hair from the face the sharp needle only can be used.
The moistened sponge electrode connected to the (+) positive pole of the circuit is placed into the hand of the patient, who lies in a chair with her head on a level with the physician’s chin when operating. The light should be southern, or such that the shafts of the hairs show plainly.
The operator turns on the current, holding the needle holder in the right hand which is connected by a flexible cord to the (-) negative pole. The rheostat handle is brought back so that just the least current is flowing. The needle is now thrust down into the follicle containing the hair. This must be done very gently so as to feel when the papilla has been reached by the needle. The depth to which the needle goes varies very much according to the size and place of the hair. It may be less than one eighth and more than one fourth inch.
The patient holding the sponge will at once feel a stinging sensation when the needle enters the skin, which is later not as objectionable. The current is now increased by advancing the handle of the rheostat until about eight milliampères are shown by the index on the dial.
Within a few seconds a white froth will issue from the follicle, showing that decomposition of tissue is taking place. The operator must familiarize himself with[481] the time and amount of current required to destroy superfluous hairs. Coarse hairs may require as much as fourteen milliampères, but it is advisable to use a moderate amount of current and to leave the needle a little longer in the follicle to avoid scarring of the skin.
The papilla having presumably been destroyed, the patient loosens her grip on the sponge and the needle is withdrawn.
The operator now takes up an epilating forceps, such as shown in Fig. 517, and removes the hair. If the hair does not come out of the follicle readily it shows that it has not been destroyed, and the same treatment, just described, must be repeated, but for a shorter duration.

Fig. 517.—Epilating Forceps.
When the hair is removed it will show more or less bulb according to its size and nourishment.
The physician now proceeds to remove the coarse hairs first. Hairs should not be removed too closely placed, as the current will destroy the tissue between the follicle and cause scarring. It is better to remove the hairs some distance apart, leaving the remaining hairs for later sittings.
About forty or fifty hairs may be removed at one sitting. This will require from half to an hour and a half of time, but the operator will soon accomplish considerable work in a minimum of time.
Some of the hairs removed will return, showing as black or dark specks in the skin, in from five to ten days. The number returning depends on the operator’s skill. At first he should not be surprised to see fifty per cent come back, but this ratio is reduced so that only three or four hairs out of fifty may return, and perhaps these stunted in growth.
The electrolytic removal of hair does not stimulate the growth of the finer hairs of the skin; that general belief has been erroneous.
Where there is considerable hair to be removed, as with a beard on a woman’s face, several sittings may be given a week and at different parts of the face, but with the average patient only one sitting should be given each week.
More or less edema follows the removal of hair, which may remain for a day or more. Warm applications will help to remove it.
The operator should at no time state a definite fee to remove the hair on the face, unless he is certain of the number present. Such judgment is, indeed, very misleading.
Moles, warts, fibromata, fungoids, and other excrescences are best removed with this method, especially where they are of the nonpedunculated type. It is hardly necessary to state that very light currents should be used for the light flat growths, such as a dark freckle or a small yellow mole. The amount of current required varies from 6 to 24 milliampères, according to the size of the body to be removed.
The same procedure as with the removal of hairs is followed. Positive electrode in the hand of the patient, negative pole to the needle holder. The needle is thrust through the growth on a plane with the skin and slightly above it. The current will at once produce a pale color in the mass and white froth will issue about the shaft of the needle. A comparatively greater amount of current is needed for this purpose than with the destruction of hairs. The operator must judge the amount and time required from experience.
The mass is punctured in stellate fashion to assure an even necrosis, as shown in Fig. 518.
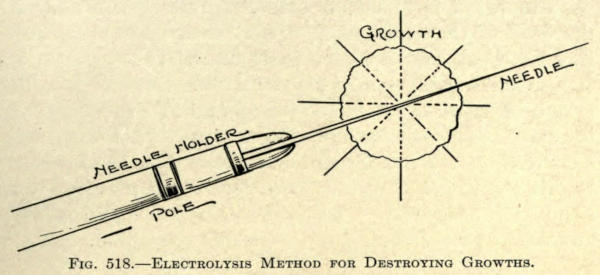
Fig. 518.—Electrolysis Method for Destroying Growths.
The mass will appear much softer after this treatment, is in some cases, as with flat moles, quite friable, but this disappears in a few hours and the mass begins to shrivel and dry up, forming a scab, which is between brown and almost black in color. This scab falls off in several days, according to its size, leaving a pink eschar, which gradually turns white and shows very little, if the growth has not been too large and the electrolysis carefully done. If little tumefactions, or tips of tissue, still appear, they are removed as soon after the scab falls off as deemed advisable by the same method. Warts show more or less recurrence.
In this condition there appear in the skin one or many dilated capillaries. It is quite common about the sides and lobule of the nose and just inferior to the malar prominence of the cheeks. To destroy these the fine platinum needle is thrust through the skin and directly through the canal of the vessel. The same disposition of the electrode is used as heretofore described.
Immediately the current is made, a series of bubbles of hydrogen will run through the vessel which presently becomes pale and empty, as a result of the electro-chemical action.
The needle should be allowed to remain in the vessel from five to ten seconds, according to the size of the latter.
The object is to set up sufficient irritation in and of the walls of the vessel so as to occlude it when cicatrization has been established. Some edema follows such a treatment, subsiding in a day or more. Several vessels may be treated in the same sitting, and at either side of the face. The operator should guard against too strong a current, to avoid scarring of the skin. The final result in this treatment shows fine punctate scars, as after the removal of coarse hairs, and sometimes pale linear scars, but these are observable only on close inspection.
Birthmarks, port-wine marks, and other pigmentary conditions may be entirely or partly removed from the skin of the face, according to the size of the area treated and the nature of the case. For this purpose the single needle attached to the negative pole is hardly sufficient, unless the spot is exceedingly small, therefore a bunch needle electrode is used. This electrode has a number of fine steel needles set into it, as shown in Fig. 519.
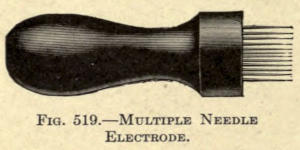
Fig. 519.—Multiple Needle Electrode.
In this treatment the needles are made to puncture the skin at right angles to them to a depth corresponding to the papillary layer. These pigments lie above that, so that it is not necessary to include the derma. At each point of puncture a white spot will appear which soon turns red. In a day’s time a number of fine scabs, or a single scab, will form over the parts treated, which fall away in about five days eventually, leaving the parts[485] paler than before, owing to a number of minute punctate scars.
The amount of treatment given in each case varies with the extent of the lesion. If the result from the first sitting has not accomplished as much as desired, it can be repeated over and over until the parts assume a normal tint. There may be more or less bleeding following the treatment; this is easily checked by pressure. If the part worked on is quite large, dry aristol dressing should be used to avoid infection. The scab should not be picked off by the patient, but allowed to fall off.
The best method of removing such pigmentations of the skin is to remove them with the knife when possible, and to cover the wound by sliding flaps made by subcutaneous dissection at either side of the wound, as in the Celsus method. Some authorities advocate their re-tattooing with papoid solution, while others prefer caustic agents, with the object of destroying the pigmented area. These methods are not to be preferred, since they leave unsightly burn scars.
Electrolytic needling may be tried and is quite successful when the marks are very small, but, as with gun-powder stains, they are best removed by punching, or cutting out, a little cone of skin containing the pigment. The secondary wounds thus made leave only very small punctate scars that are hardly noticeable. Of course a number of such removals would not be advisable.
Where the pigmentation is very pale, recourse may be had to the peeling method, as will be later described.
Not infrequently the cosmetic surgeon is called upon to remove or improve unsightly scars about the face,[486] the result of injuries or burns and after the careless coaptation of such wounds. The scars vary in extent and degree, from a mere pit due to varicella or variola to the broad areas following the cicatrization of lupus and burns. Surgical scars vary also from a mere line to areas of greater or less extent, dependent upon the ablation of neoplasms or the granulation of wounds due to any cause.
The treatment of scars depends upon their size and location. A mere linear scar may be reduced by electrolysis, the needle, negative pole, being introduced equidistantly, from one sixteenth to a quarter inch apart, with the hope of causing a breaking down electro-chemically of the scar itself and waiting for secondary cicatrization. In other words, making a scar within a scar.
This mode of treatment may be repeated in two or three weeks and has the tendency of breaking up the shiny line of light that makes the scar stand out prominently from the skin.
Such scars, where nonadherent, or flat with the plane of the skin, may also be tattooed to reduce their white color.
For this purpose, the red or carmine pigment used for tattooing is diluted and pricked into the scar tissue with a fine cambric needle by hand or electric process.
When the scar is small the line is punctured here and there and the aqueous solution of the pigment is painted over the area, which is again worked over to make it take.
For larger scar surfaces multiple needles are used. These are composed of from four to ten needles soldered together at their eye ends, leaving the points at an even level.
The electric method is the most serviceable for tattooing large scars.
These instruments are electro-magnetic devices made[487] to accommodate single or multiple needle points and can be obtained from instrument makers.
The author has had a special electric synchronous reciprocal apparatus made, as here shown in Fig. 520, which is much more compact than the ordinary electric apparatus found on the market. It works on the principle of the sewing machine needle.
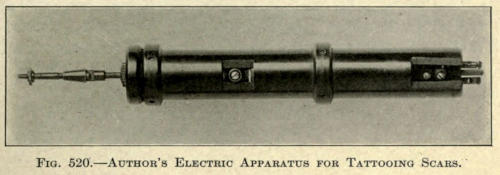
Fig. 520.—Author’s Electric Apparatus for Tattooing Scars.
In using the electric apparatus the needle ends are dipped into the pigment paste, to which a little glycerin is added to bind it, and this is tattooed or pricked into the scar.
If, after the parts are healed, the color is too light, the scar may again be gone over until the tint matches somewhat the tint of the skin. Other pigments may be used, according to the complexion of the patient.
Some scars, the resultant of negligent coaptation, are to be excised according to the Celsus method and are brought together with a number of fine silk sutures.
If the skin is found to be attached too closely to the subcutaneous structure, it must be dissected up to render it mobile.
When the scar cannot be removed by excision the hypodermic use of thiosinamin may be tried.
Thiosinamin or rhodallin is only slightly soluble in water, but the addition of antipyrin according to Michel renders it useful for hypodermic use. The formula preferred by the author is made as follows:
| ℞ | Thiosinamin | grs. ij |
| Antipyrin | grs. j | |
| Aqua dest. | gtts. xx. |
The above solution makes up a single injection, which is to be made directly under the scar or into the muscular tissue below it. Two injections are given each week.
The treatment is to be continued until the texture of the cicatrix is equal to that of the skin.
These injections are more or less painful and may be supplanted to advantage with the hypodermic use of fibrolysin (Mendel), in which each 2.3 c.c. correspond to three grains of thiosinamin.
For very small scars, as those occasioned by blepharoplastic operation, the author employs the twenty-per-cent thiosinamin plaster mull made by Unna. These are to be applied every day or night, according to the convenience of the patient, and allowed to remain on for several hours each day.
At first these plaster mulls are inclined to cause erythema and exfoliation of the epithelium, therefore they might be used on alternate days to keep the parts more sightly.
For scars of large extent the above method will answer best. If there is considerable contraction, the parts should be massaged daily to soften and stretch them. Eventually the depression of contour may be corrected by hydrocarbon protheses introduced subcutaneously following subcutaneous dissection, if deemed necessary.
Small pits, where discrete, are best removed with a fine knife and brought together by a fine suture which is to be removed on the fifth day.
Confluent pittings, as after variola, must be removed by decortication or peeling methods.
The pits, if spread about the face promiscuously, may be treated separately by the peeling method, but when[489] they lie less than one inch apart, it is best to treat the skin of the whole face.
This is done by applying pure liquid carbolic acid to the skin with a cotton swab. The skin at once assumes a white color. If the pittings are not very deep, one application of the acid is sufficient. If deep, one or two more applications are made as the preceding one dries. In very deep pits, the surgeon should apply the acid to the pit proper several times, blending off the application at the periphery.
When the surface thus treated has become dry, adhesive plaster, cut in half-inch strips of desirable length, are put on the face, one above the other, slightly overlapping, until the whole treated surface is well covered, mask-like.
The author uses Unna’s zinc oxide plaster mull for this purpose, as it is backed with gutta-percha, which readily adapts itself to the curvatures of contour.
The adhesive plaster mask is not removed until about the fourth or fifth day, when it will be practically forced away from the skin by the excretions thrown out from the derma. In some cases there is considerable pus.
After removal of the mask the skin, now very red and tender, is cleansed with a solution of bichloride, 1 in 10,000.
After the cleansing a mild soothing ointment, such as zinc oxide in vaselin, is used for several days until the skin takes on its normal epitheliar layer and appears normal in color.
No water or soaps are to be allowed during the latter period. In the later days of the treatment the skin may be cleansed with a little borated vaselin or even olive oil used with absorbent cotton.
If there is a pigmentation of the new skin this should cause no alarm, as it will fade out in from six to eight weeks.
Tincture of iodine has been used for the same purpose, as well as its mixture with carbolic acid.
Resublimed resorcin is also advocated, but the resultant peeling will not prove thick enough to give a satisfactory result.
If, for any reason, the effect obtained is not as desired, the patient should wait for several weeks and have the treatment repeated.
It is hardly necessary to say that the application used should not get into the eyes. The upper eyelids should not be treated, since no benefit arises from it. If there is a redundancy of tissue, it should be removed surgically, as heretofore described.
Every case, whether of little consequence or of important nature, should be properly and fully recorded in a thorough and systematic manner. Apart from the value of such a record, to the operating surgeon it often proves of the greatest importance in cases where operations of a purely cosmetic nature are undertaken.
Patients who beg us to make them more beautiful, or less unsightly in the eyes of the ever-critical observer, are the most difficult to please, and often complain, after a few days of constant mirror study, of the parts changed by methods that are the result of years of hard-earned experience, that the nose or the eyes or the ears have not been changed as much as they desired—in fact, so little that their closest friends have failed to evoke ecstatic remarks about the improvement.
This is not unusual with the most intelligent patients and is due to the fact that cosmetic operations performed on an ugly though otherwise normal organ have not yet become very frequent, and while friends are inclined to remark a change in lesser defects, they fail to credit this to the cause, owing to a lack of the knowledge of cosmetic surgery, or their ignorance of the art entirely.
Photographs.—Where a pathological defect, wound, or scar or traumatic deformity is to be corrected, the patient is usually kind enough to permit of photographs being made of the parts to be operated on, but where the defect is hereditary, or the result of age, objections are[492] invariably raised by all concerned, for fear their pictures will be used in some outlandish way.
The objection to photographs is obvious, since it usually requires visits to a studio, and the necessary loss of time to the surgeon, whose presence is nearly always necessary to secure the proper negative.
This is especially true of the nose. Very few photographers will make a satisfactory sharp profile picture. It is less artistic, but most desired by the surgeon, and when the patient is presented for a second negative after the operation has been performed, the picture varies more or less in pose from the first taken.
It would be well for physicians to have a camera for use in the operating room, and those who can manipulate one will find that taking a 5 × 7 negative the most suitable.
Stencil Record.—For those who cannot provide themselves or bother with a photographic apparatus, the stencil record is recommended.
For this purpose a picture of a normal eye and its[493] lids, a nose, lip or ear, is drawn upon a piece of oiled or stencil paper, or upon any thick, stiff book board.
The paper is laid down upon a plate of glass and the outlines of the picture are cut out, wide enough to allow the sharpened point of a pencil to pass. Where the lines are long it is advisable to allow connecting links to remain at various intervals as desired to keep the stencil stiff and to prevent cut margins from slipping or rolling up. (See Fig. 521.)
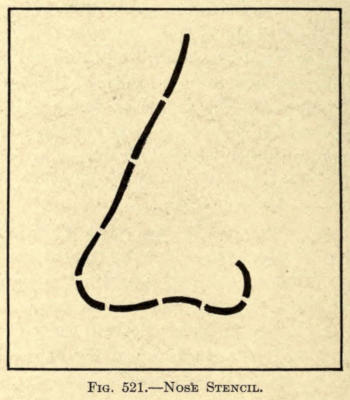
Fig. 521.—Nose Stencil.
The stencil thus made is laid upon the record card and a tracing is made upon the latter by passing the lead-pencil point along the cut outline.
The stencil is now lifted and the defect sketched into the picture of the normal organ.
If this should be the anterior nasal line, a perfect sketch can be made of the defect by placing a card alongside of that organ and drawing the outline upon it as the pencil is made to glide over the nose, the point facing the card in such a way that a true profile outline is obtained. The card is then cut along the pencil line.
The nasal section of the card is now placed upon the stenciled nose and its outer border traced into or over it, as the case may be, by drawing the pencil point along the outer margin.
The same method may be followed post-operatio. This method can be employed for the other parts of the face as well, as, for instance, the mouth, ears, base of nose, etc.
Distances in measurements should be put into the record drawing to make it more exact.
The Rubber Stamp.—Another method is to make outline sketches of normal parts of the face with India ink upon drawing board and have those reproduced in rubber stamps, using the stamp in place of the stencil and marking in the defect in the manner before mentioned.
The Plaster Cast.—The best method by far, however, and the one found most accurate, is the plaster cast. It is not[494] a difficult thing to make a cast of a nose, eyelid, lip, or ear, and the latter is much more preferable to any other method of record.
For this purpose some modeling clay is required, which is molded into a strip and laid around the part to be reproduced.
This forms a sort of raised ring or border and prevents the overflow of the semiliquid plaster, and avoids the annoyance of trickling the liquid upon other parts of the face about the site of the part worked on; at the same time it permits of neatness and uniformity in the size and shape of the casts to be filed away as records. (See Fig. 522.)
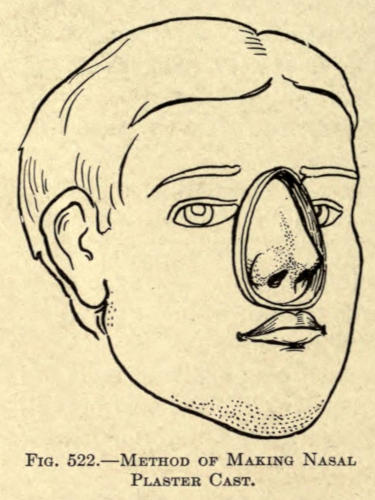
Fig. 522.—Method of Making Nasal Plaster Cast.
The skin surface, and hair, if any, within this ring area, before using this plaster of Paris, is now thoroughly coated with clean oil, or petrolatum, applied with a soft sable brush. The inner and upper part of the wax ring is also coated.
If there are openings in the parts of the face, such as the nostrils or the auricular orifice, they should be plugged lightly with dry absorbent cotton, care being taken, however, to avoid distending the alæ.
The plaster is now prepared in a small porcelain or soft rubber bowl by adding warm water to it until the powder, upon stirring, forms an even semiliquid paste.
This is poured first upon the area to be reproduced to fill all the finer crevices and to avoid air holes, and is then put on with a spatula, or wooden slab, until the[495] space within the clay boundary is properly filled, covering the organ all over with a layer ¼ to ½ inch in thickness on all sides. Over the eyelids a thin coating of plaster should be used, whereas over other parts of the face a thickness of half an inch can be allowed without discomfort to the patient.
It is well at first to make the plaster thick, as the mold is liable to be broken upon removal or in drying. After a little experience splendid results are obtained with very thin walls of plaster.
The plaster is allowed to dry and harden, while the patient is instructed to remain still and silent. If a cast of the nose is made, the patient should refrain from talking and breathe gently through the mouth.
Tapping on the plaster now and then with a lead pencil will show when it has hardened sufficiently to be removed.
A firm, quick pull relieves the mold.
In molds of the ear an anterior and posterior impression should be made, if a cast of the entire organ is desired. This can be done by first applying a layer of plaster to the posterior surface up to the outer rim, allowing this to harden and painting the anterior ear and the exposed plaster border with petrolatum before putting the plaster over it. Upon traction, when set, the plaster will separate readily at the point of the separation.
The removed piece of set plaster is called the mold.
It is allowed to dry thoroughly and then preferably coated inside with a thin coat of liquid petrolatum, which is found to be much better than oil.
A thinly prepared paste of plaster is poured into it at the outer brim and allowed to harden. The best results are obtained by setting the mold into a small pasteboard box in which it is held in proper position and prevents the thin plaster from running over the depressed edges.
By gently tapping the mold when the cast has set, it is made to separate from the latter sufficient to permit of separating or cutting away of the mold inside of it.
The cast, when removed and dry, is coated with white shellac varnish. Upon its reverse side a note is scratched into it, giving the case number, or such information as the surgeon may desire.
The author advises the addition of a small quantity of Armenian bole to the plaster used for the cast, as it gives a less ghastly tint and aids much by its color in the cutting away of the white mold from the cast. Several of these casts, taken before and after operation by the author, have been shown in the preceding chapters.
After operation and healing of the parts a second cast is made.
Hooks can be inserted into the casts, when still soft, to hang them up by, or loops of string or wire are stuck into them, while setting for the same purpose.
Such a collection is not only of great value to the operator, but is a means of constant and absolute record, even to the extent of reproduction by photography.
The necessary data in respect to the method employed in operating, dressing, etc., is to be added to the record as generally done with medical or other surgical causes.
Preparation of Photographs.—There are some cases of which no other permanent record can be made, except by photograph. If these can be obtained, the negatives are to be printed without retouching, the prints being made on silver printing paper of the glossy type to permit of reproduction in half-tone when desired at some future time.
In printing such pictures, the eyes, or other part of the face not operated on, may be obliterated by laying strips of paper next to the negative, the part thus covered coming out white in the positive.
The photographs made of parts to be operated on[497] should be made as near as the normal size, for obvious reasons of accuracy and measurement.
This can be done by comparing the size of the part to the picture found on the ground glass.
Cameras that do not permit of ground-glass focusing are useless as well as uncertain. Time exposures are necessary for the best results.
Dark backgrounds should be used to get the sharp outlines by contrast. Too much light on the parts, such as direct sunshine, is undesirable, as it makes the parts appear flat and lifeless; therefore a muslin screen is of great value to graduate the intensity of the light, and if this is not at hand, a sheet of paper will answer the same purpose.
In printing make note of the depth of color of the parts most desired to be shown, varying with the different parts of the face. Look to contrast, and in pathological cases have the diseased area printed so that it will stand out forcibly as compared to the fellow organ in health or the normal tissue beyond its border.
To protect photographic records, they should be properly bound in book fashion to avoid scratching, rubbing, or breaking. This not only implies neatness and thoroughness on the part of the surgeon, but also permits of ready reference at all times.
An index to the contents of such a book is a desirable adjunct.
THE END